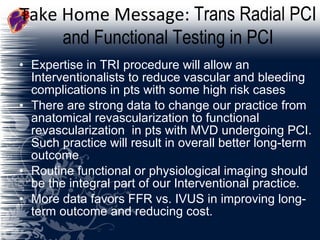
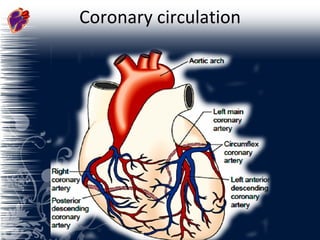
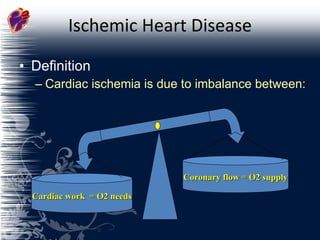
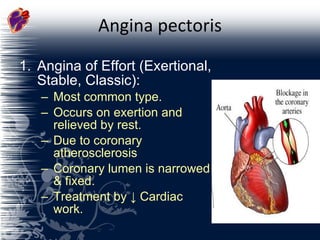
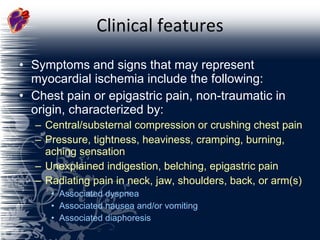
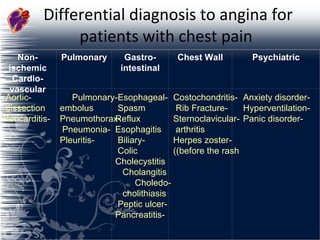
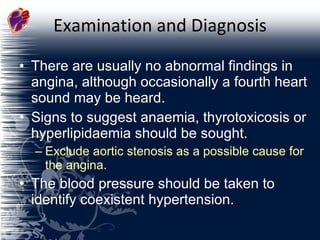
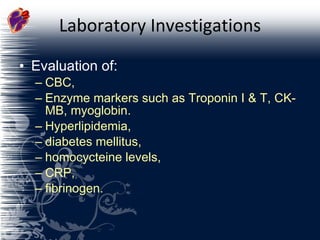
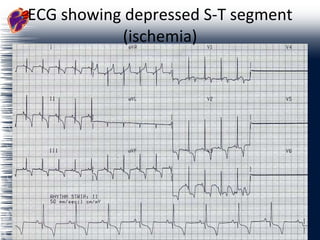
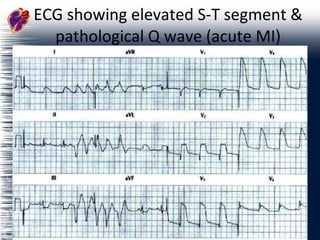
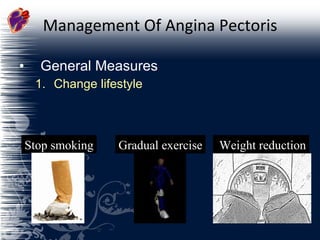
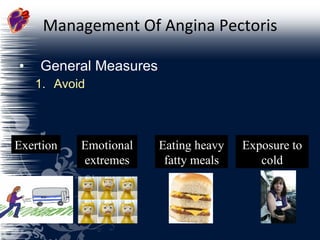
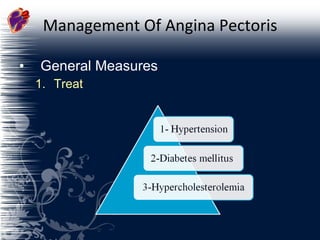
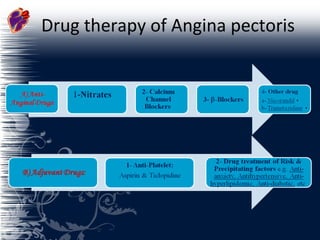
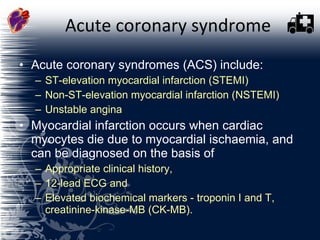
The document discusses coronary artery disease and ischemic heart disease. It defines ischemic heart disease as a lack of balance between coronary blood flow and oxygen supply to the heart and cardiac workload and oxygen demands. Risk factors for ischemic heart disease include age, sex, family history, hypertension, hyperlipidemia, smoking, diabetes, and lack of exercise. Types of angina pectoris and their causes and treatments are explained. Diagnostic tests for ischemic heart disease like ECG, exercise stress testing, and coronary angiography are also summarized.
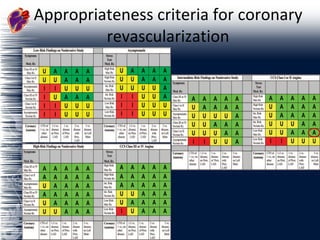
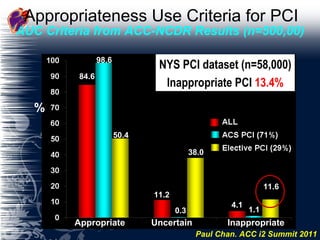
![Appropriateness Use Criteria [AUC] for PCI 84.6 11.6 1.1 11.2 0.3 38.0 4.1 98.6 50.4 Appropriate Uncertain Inappropriate % AUC Criteria from ACC-NCDR Results (n=500,00) Paul Chan. ACC i2 Summit 2011 NYS PCI dataset (n=58,000) Inappropriate PCI 13.4%](https://image.slidesharecdn.com/acd-110603234217-phpapp02/85/Acute-Coronary-Disease-60-320.jpg)