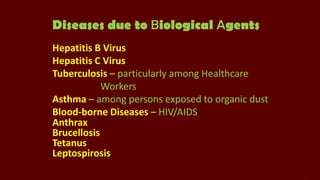
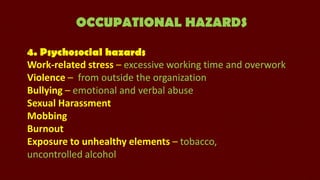
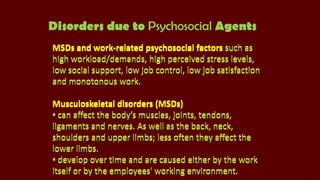
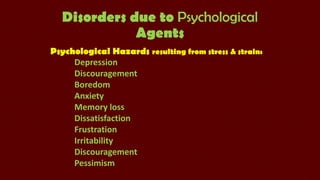
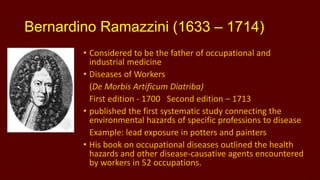
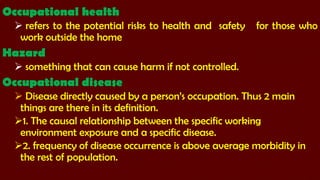
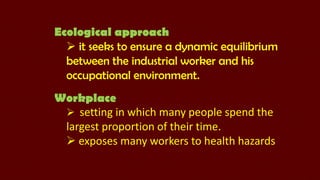
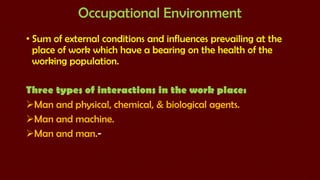
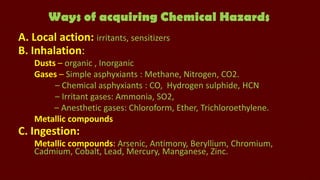
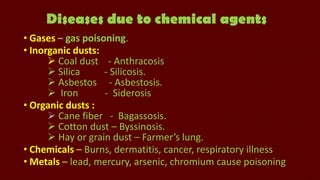
This document provides historical context on occupational health and discusses key figures and concepts. It summarizes that Bernardino Ramazzini in 1700 published the first study linking environmental hazards to specific occupations and diseases. In 1775, Sir Percivall Pott associated cancer with occupational exposure from chimney sweeping. Occupational health refers to risks and safety for work outside the home. Occupational diseases are directly caused by a person's occupation. The document outlines various occupational hazards like physical, chemical, biological, ergonomic and psychosocial factors and diseases they can cause. It also discusses prevention of occupational diseases through various medical and environmental measures.

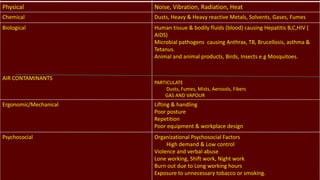
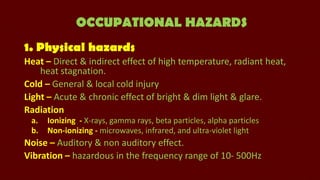
![Diseases due to Physical agents
Heat – Heat stroke, Heat hyperpyrexia, Heat
syncope, Heat Exhaustion, Heat rash.
Light – Occupational cataract, Miners nystagmus.
Cold – Hypothermia, Frost bite, Trench foot.
Pressure – Air embolism, Blast injuries.
Vibration – Osteoarthritis, Reynaud's disease [white
fingers]
Noise – Occupational deafness.
Radiation- Cancer, genetic changes, Aplastic anaemia.](https://image.slidesharecdn.com/introductiontooccupationaldiseases-131125130528-phpapp01/85/Introduction-to-occupational-diseases-13-320.jpg)