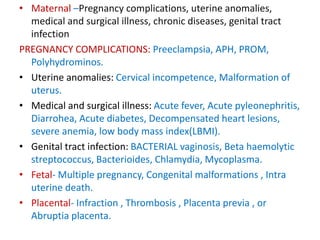
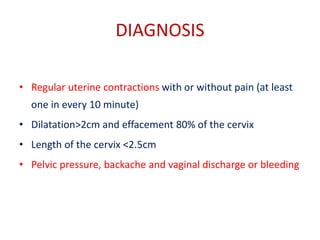
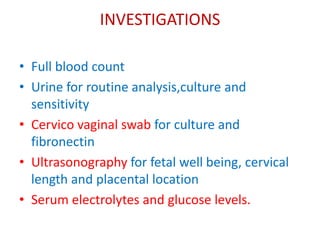
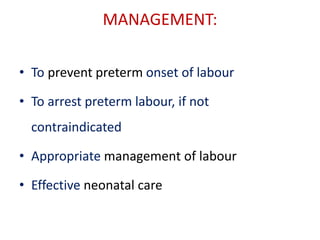
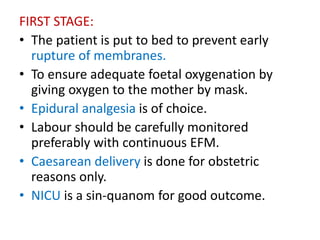
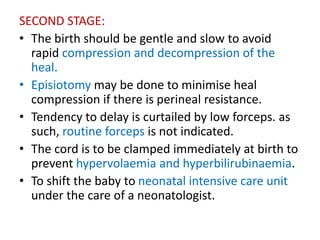
This document discusses premature labor or preterm labor. It defines premature labor as labor occurring before 37 weeks of gestation. It notes the incidence varies from 5-10% and identifies several risk factors like a history of preterm birth, infections, low socioeconomic status, and complications in the current pregnancy from maternal, fetal or placental issues. Diagnosis involves regular contractions with cervical changes. Management aims to prevent, arrest or appropriately handle preterm labor and provide effective neonatal care. Predictors include multiple pregnancy, history of preterm birth and infections while prevention focuses on reducing risk factors, early detection and prophylactic treatment.