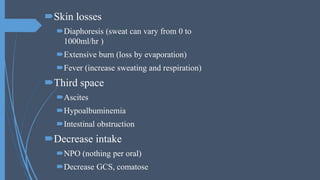
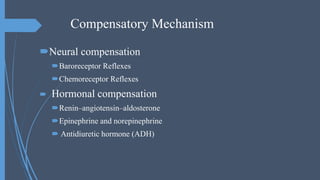
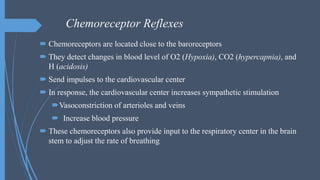
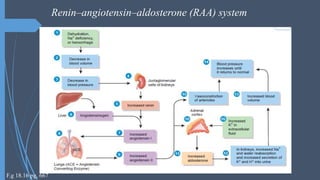
This document discusses isotonic fluid imbalance, also known as hypovolemia. Hypovolemia occurs when water and electrolytes are lost in equal proportions, keeping sodium levels normal. It can result from extra-renal losses like vomiting, diarrhea, burns, or third spacing of fluids. It can also occur due to renal losses from conditions like renal disease or diuretic use. When fluid volume is depleted, the body activates compensatory mechanisms like increasing antidiuretic hormone and renin-angiotensin-aldosterone system to conserve water and sodium. This helps maintain blood pressure and cardiac output. Symptoms of hypovolemia include thirst, fatigue, dizziness, decreased skin turgidity,