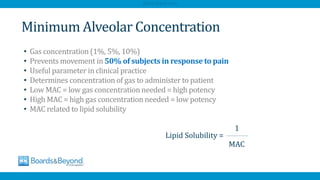
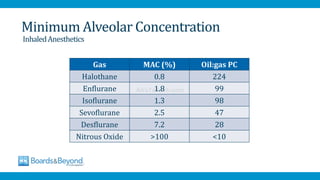
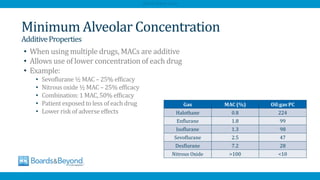
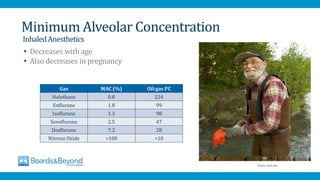
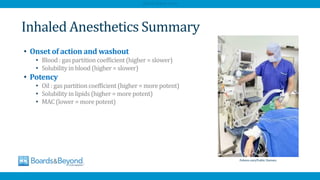
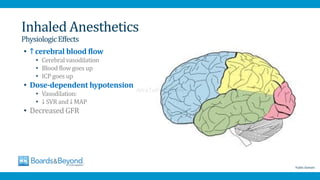
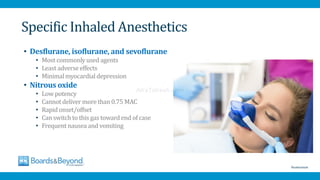
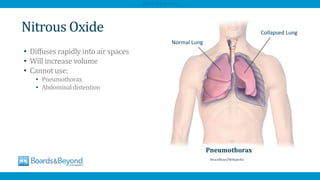
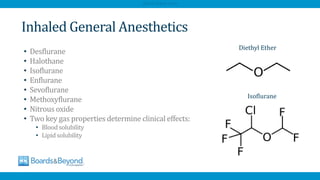
The document provides an overview of general anesthesia, its mechanisms, and the effects of various inhaled anesthetics. It discusses properties such as blood and lipid solubility, minimum alveolar concentration (MAC), and the physiological effects and specific agents used in anesthesia. Key dangers, including malignant hyperthermia and adverse effects of specific anesthetics like halothane and nitrous oxide, are also highlighted.

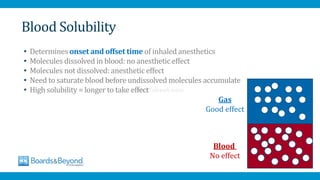
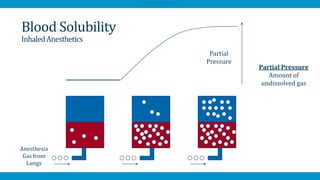
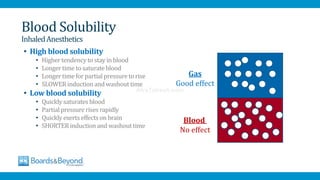
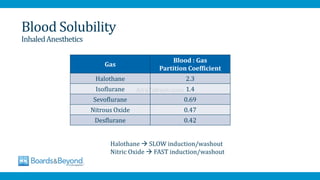
![• Blood solubility described by blood/gas partition coefficient
• Isoflurane:1.4
• [blood]1.4 > [alveoli]
• High partition coefficient = high solubility
• Low partition coefficient = low solubility
Blood Solubility
InhaledAnesthetics
Blood
No effect
Gas
Good effect
AfraTafreeh.com](https://image.slidesharecdn.com/generalanesthesiaatf-241120130829-d0ff2ba7/85/General-Anesthesia-description-for-Anesthesia-7-320.jpg)