General Anaesthetics
For Post-Graduates
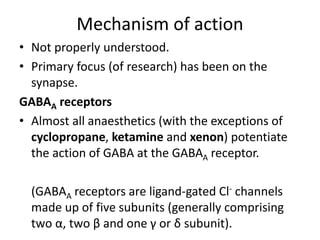
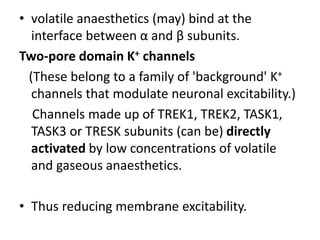
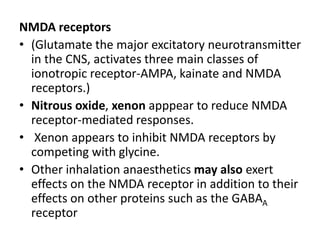
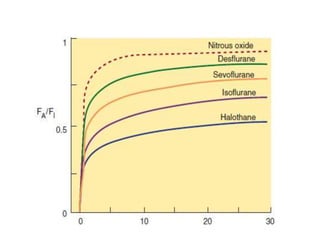
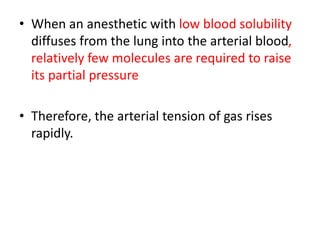
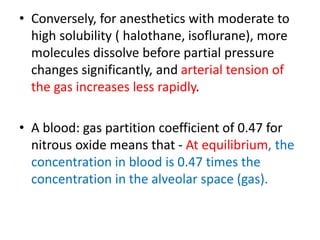
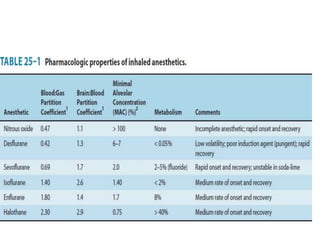
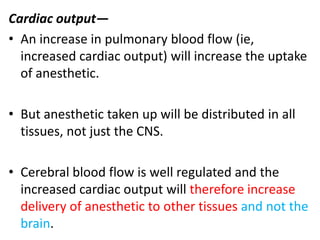
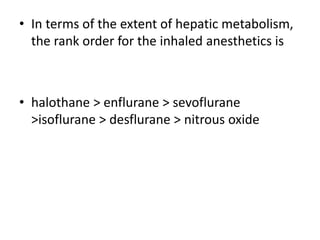
Inhalational anesthetics are either volatile liquids (e.g. halothane, isoflurane) or gaseous (e.g. nitrous oxide, xenon) that are inhaled to induce anesthesia. They work primarily by potentiating the inhibitory neurotransmitter GABA at GABAA receptors in the brain, though some like nitrous oxide also impact NMDA receptors. Their uptake in the lungs and distribution in tissues depends on factors like solubility and cardiac output. While they depress brain and cardiovascular function in a dose-dependent manner, individual agents have different organ effects. The most commonly used inhalational anesthetics today have low acute toxicity