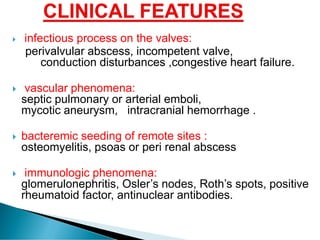
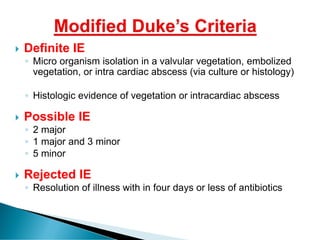
This document discusses myocarditis, including its definition, etiology, clinical features, diagnosis, treatment, prognosis, and complications. Myocarditis is defined as inflammation of the heart muscle, which can be caused by various viral and bacterial infections. Clinical features include fever, chest pain, and heart failure symptoms. Diagnosis involves electrocardiograms, cardiac imaging like echocardiograms and MRI, and endomyocardial biopsy. Treatment is supportive with medications, while prognosis depends on the age of onset, with higher mortality in newborns and potential for recovery of heart function in older children and adults.