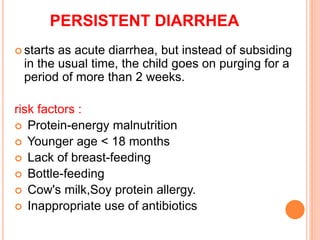
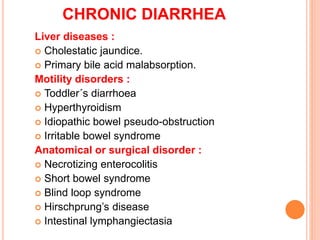
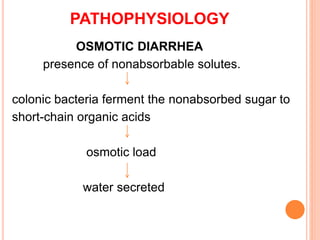
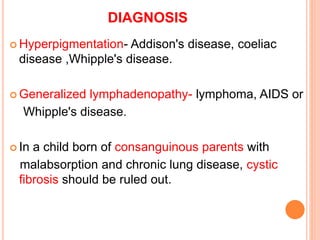
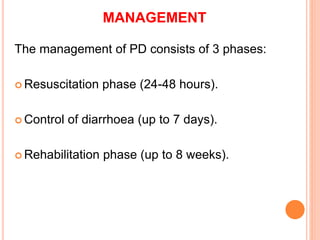
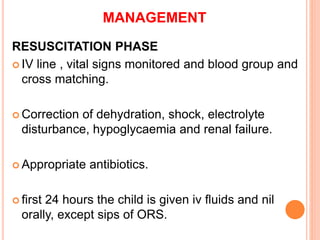
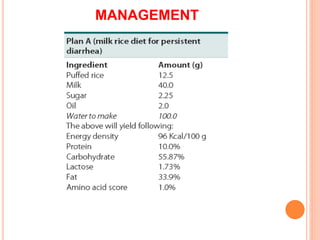
This document discusses chronic diarrhea and its causes and management. It defines persistent diarrhea as acute diarrhea lasting over 2 weeks, while chronic diarrhea has a more insidious onset and is usually due to non-infectious causes lasting over 2 weeks. Common causes of persistent diarrhea include malnutrition, infections, and food allergies. Chronic diarrhea requires further evaluation to identify underlying inflammatory, malabsorptive, intestinal, metabolic, or other conditions as the cause. Management of both involves rehydration, controlling diarrhea, identifying the cause, and rehabilitation.