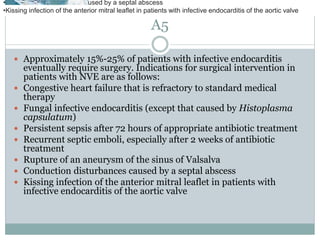
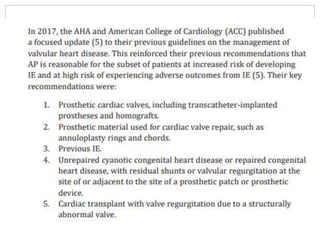
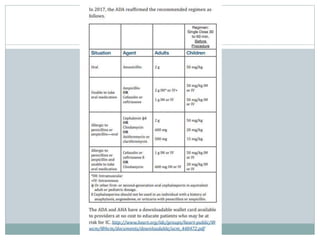
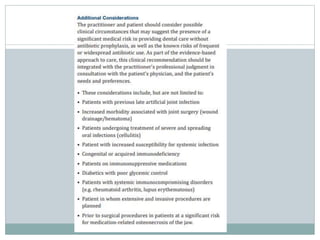
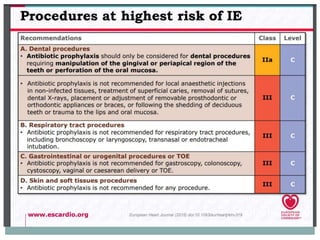
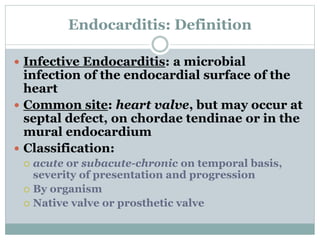
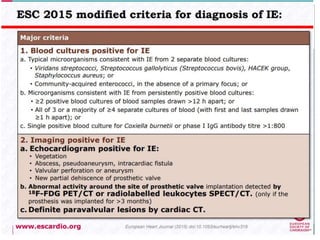
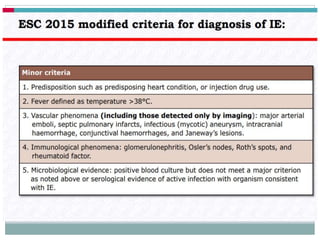
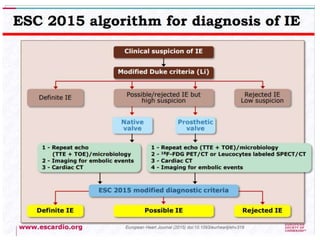
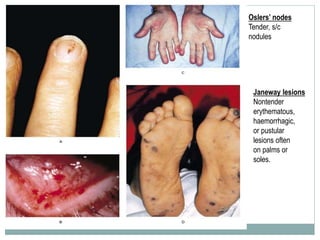
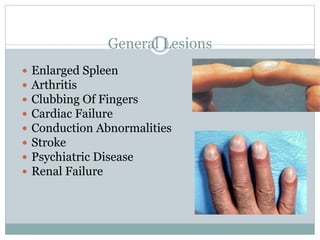
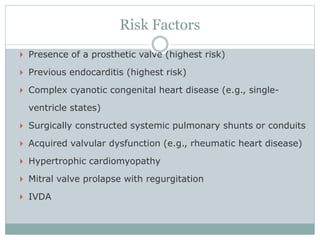
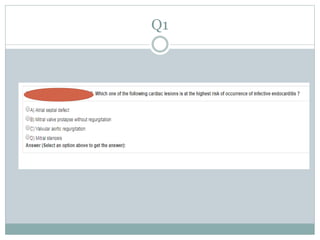
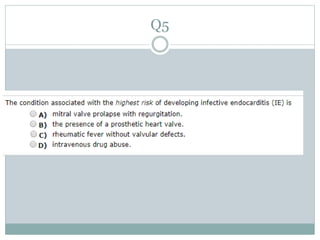
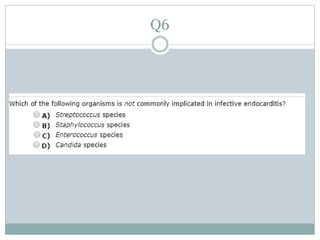
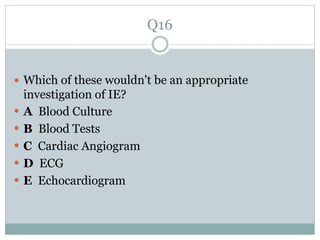
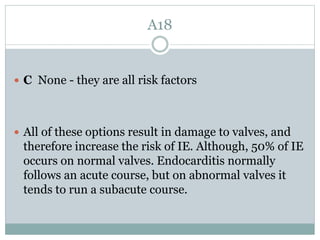
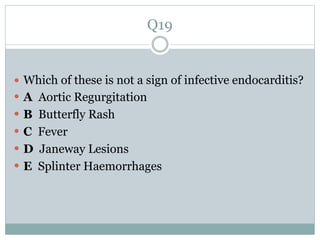
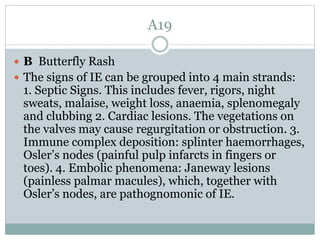
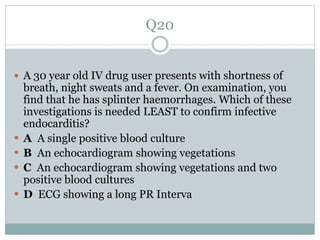
This document discusses infective endocarditis, including its definition, classification, common sites of involvement, risk factors, general lesions, mortality rates, and Osler's nodes and Janeway lesions as associated findings on physical examination. Key points covered include that infective endocarditis is an infection of the endocardial surface, most commonly involving the heart valves. It can be classified as acute or subacute/chronic based on temporal factors and severity. Overall mortality is around 40% usually due to heart failure from valve dysfunction. Having a prosthetic valve or previous endocarditis are major risk factors.