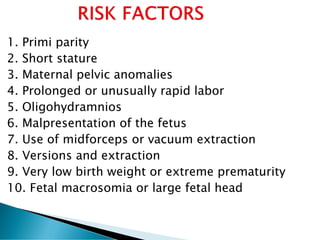
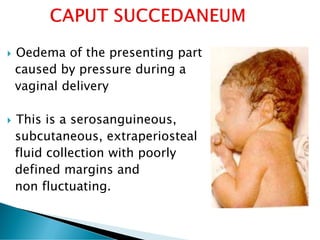
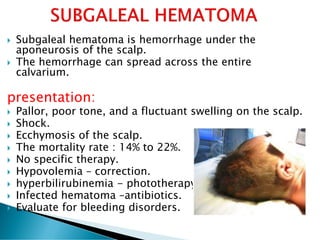
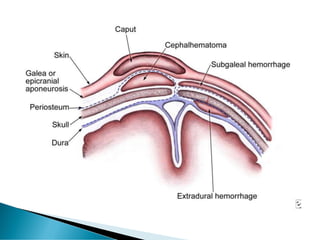
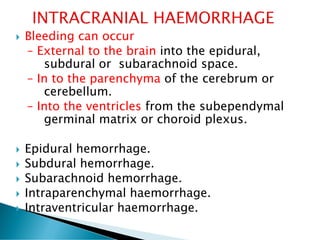
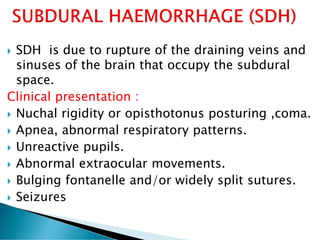
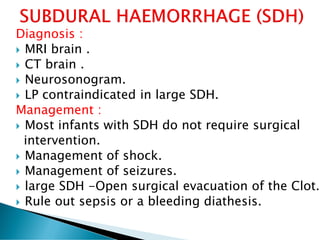
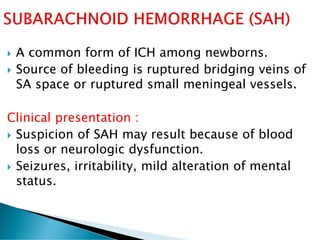
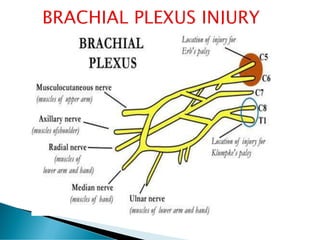
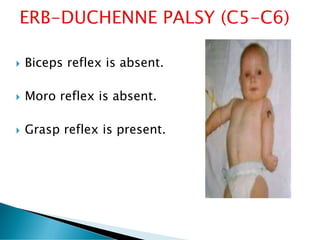
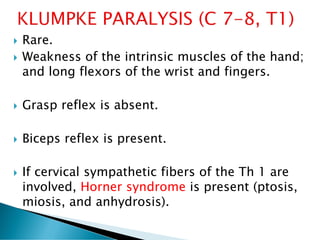
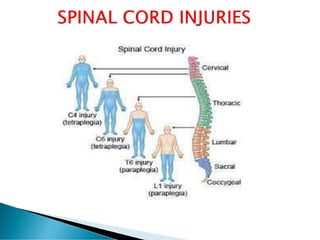
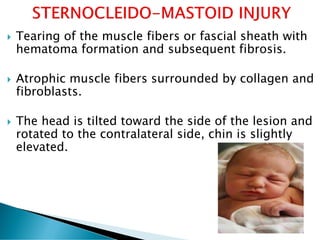
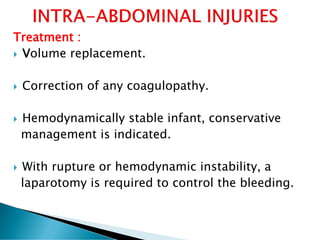
This document discusses various types of birth injuries in infants including injuries to the head, spine, shoulders, nerves and internal organs. It provides information on the causes, clinical presentations, diagnostic methods and treatment approaches for different birth injuries such as subgaleal hematoma, clavicle fractures, brachial plexus injuries, spinal cord injuries and liver lacerations. Risk factors for birth injuries including prolonged labor, large infant size and instrument-assisted delivery are also mentioned.