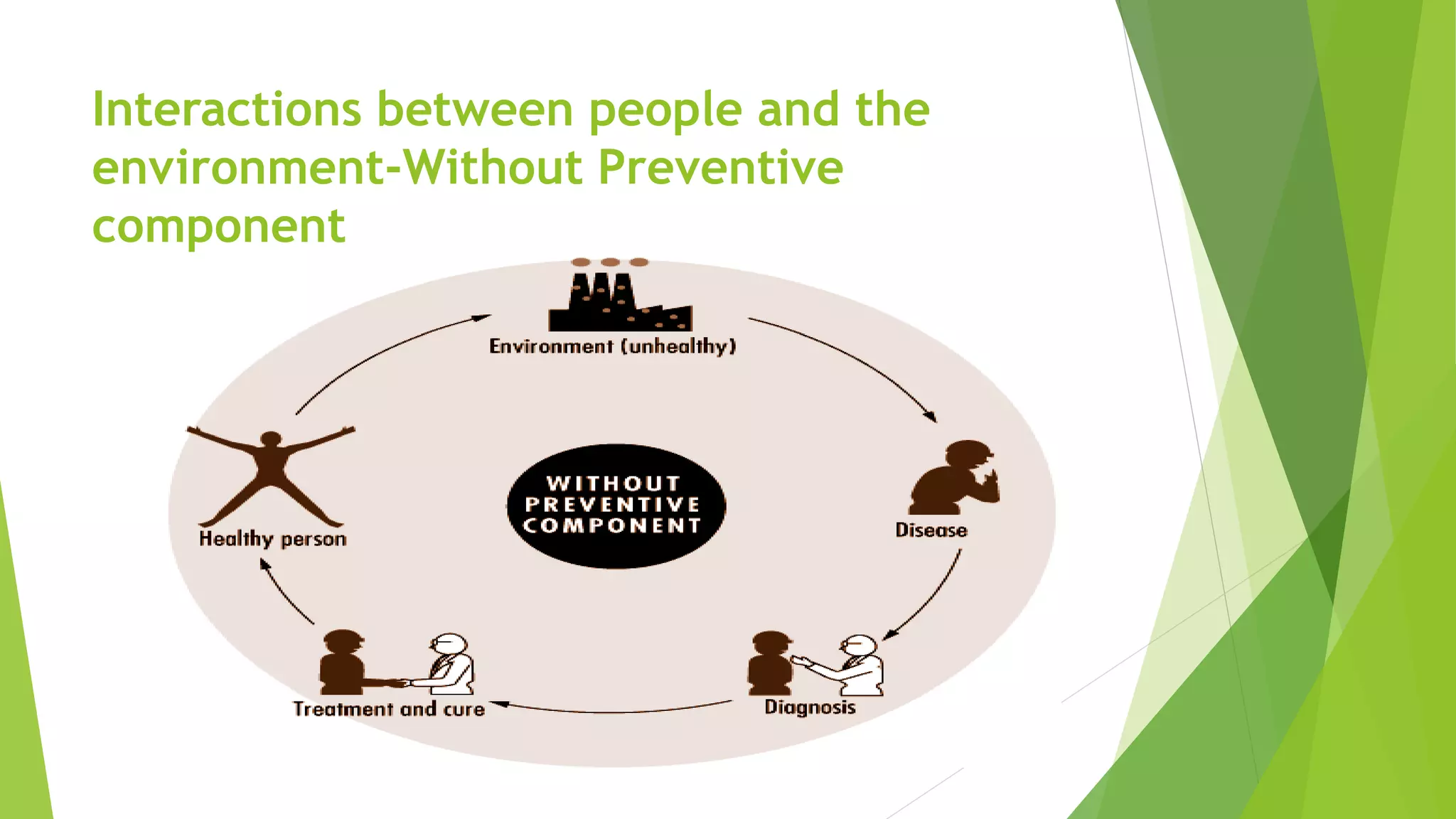
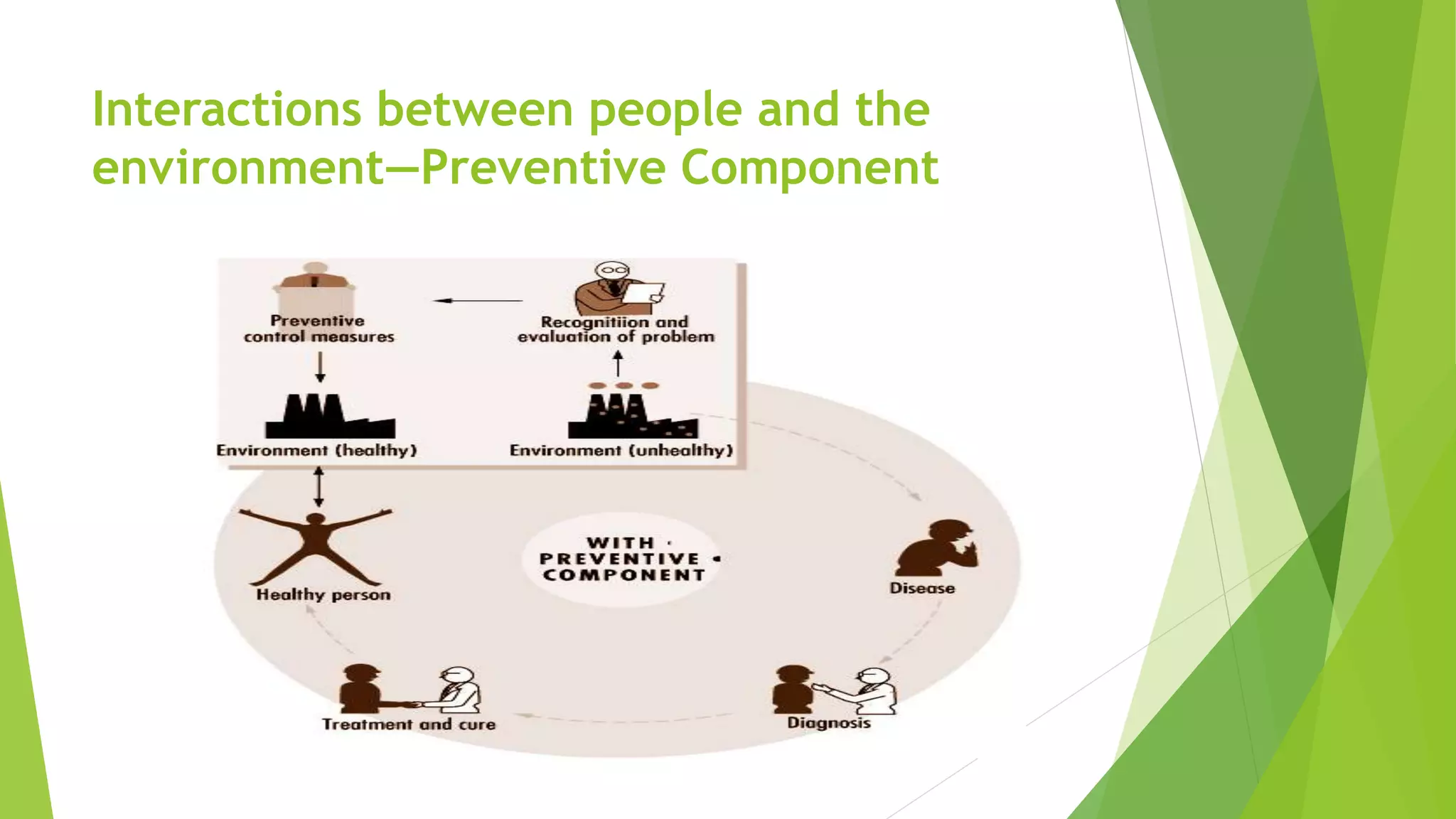
Occupational hygiene focuses on anticipating, recognizing, evaluating, controlling and preventing hazards in the workplace that can cause injury, illness or negatively impact worker well-being. It involves identifying potential hazards, evaluating exposure levels, and using controls like engineering solutions or personal protective equipment to reduce risks. Occupational hygiene benefits both workers and industry by improving health, reducing costs from injuries and absenteeism, and increasing productivity and efficiency.





![Mental Hygiene-----
A widely accepted definition of health by mental health specialists is
psychoanalyst Sigmund Freud's definition: the capacity "to work and to love".]
According to the (WHO), mental health includes "subjective well-being,
perceived self-efficacy, autonomy, competence, inter-generational
dependence, and self-actualization of one's intellectual and emotional
potential, among others. The WHO further states that the well-being of an
individual is encompassed in the realization of their abilities, coping with
normal stresses of life, productive work and contribution to their
community. Cultural differences, subjective assessments, and competing
professional theories all affect how "mental health" is defined.
The branch of psychiatry that deals with the science and practice of
maintaining and restoring mental health, and of preventing mental disorder
through education, early treatment, and public health measures.](https://image.slidesharecdn.com/industrialhygiene-170909064307/75/Industrial-hygiene-7-2048.jpg)