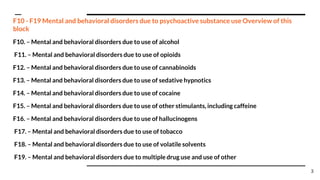
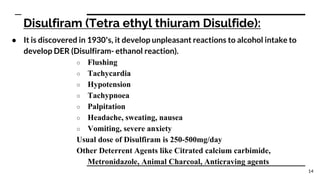
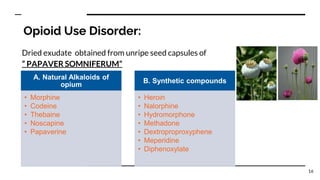
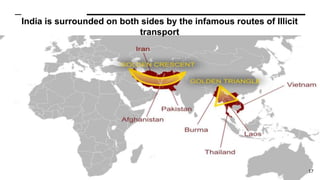
The document discusses substance use disorders and provides information on various substances of abuse including alcohol, opioids, cannabis, cocaine, amphetamines, and lysergic acid diethylamide (LSD). It covers terminology, classifications, etiology, effects of acute intoxication and withdrawal, complications, treatments, and diagnostic criteria for substance use disorders involving these classes of drugs.