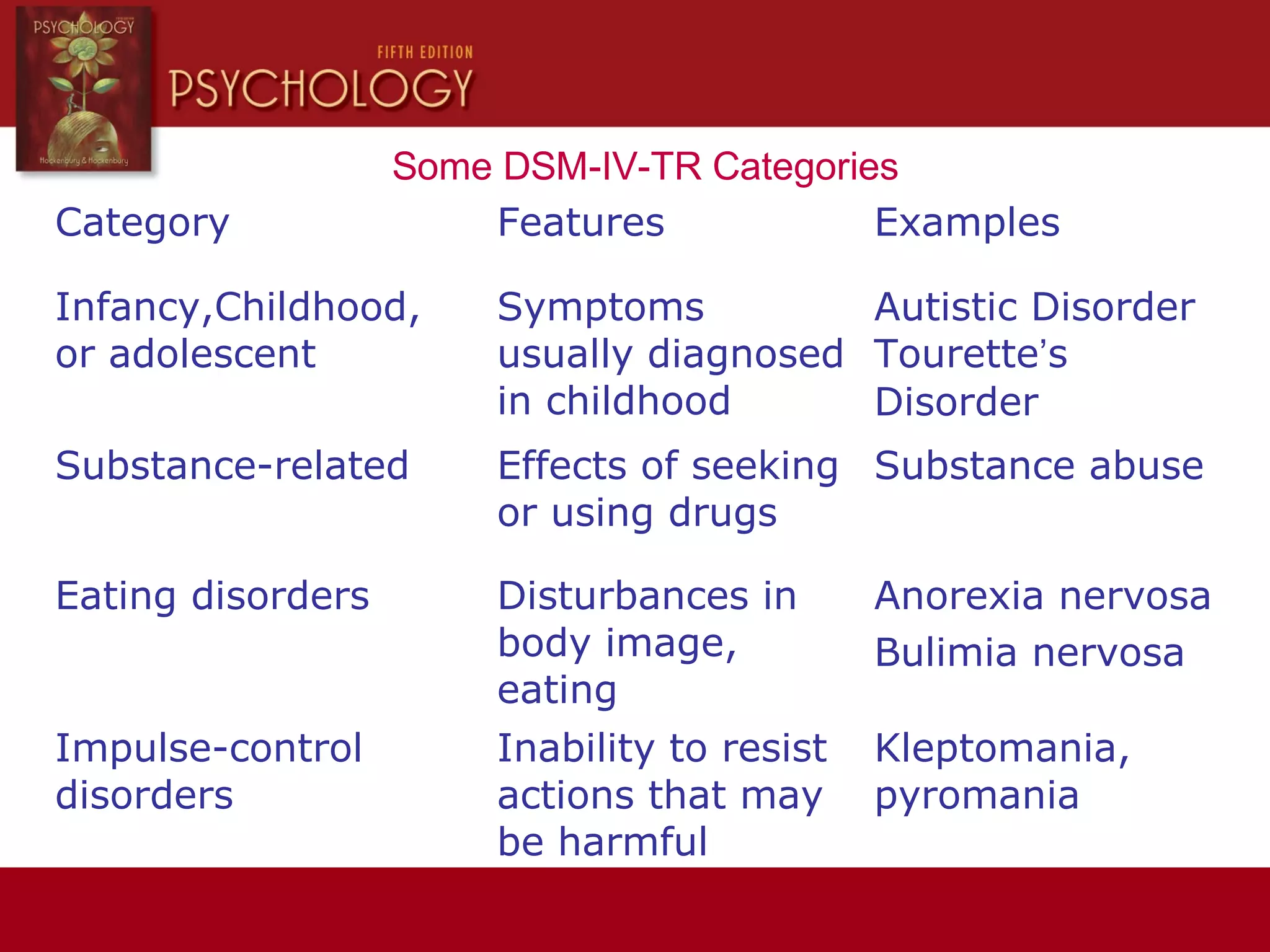
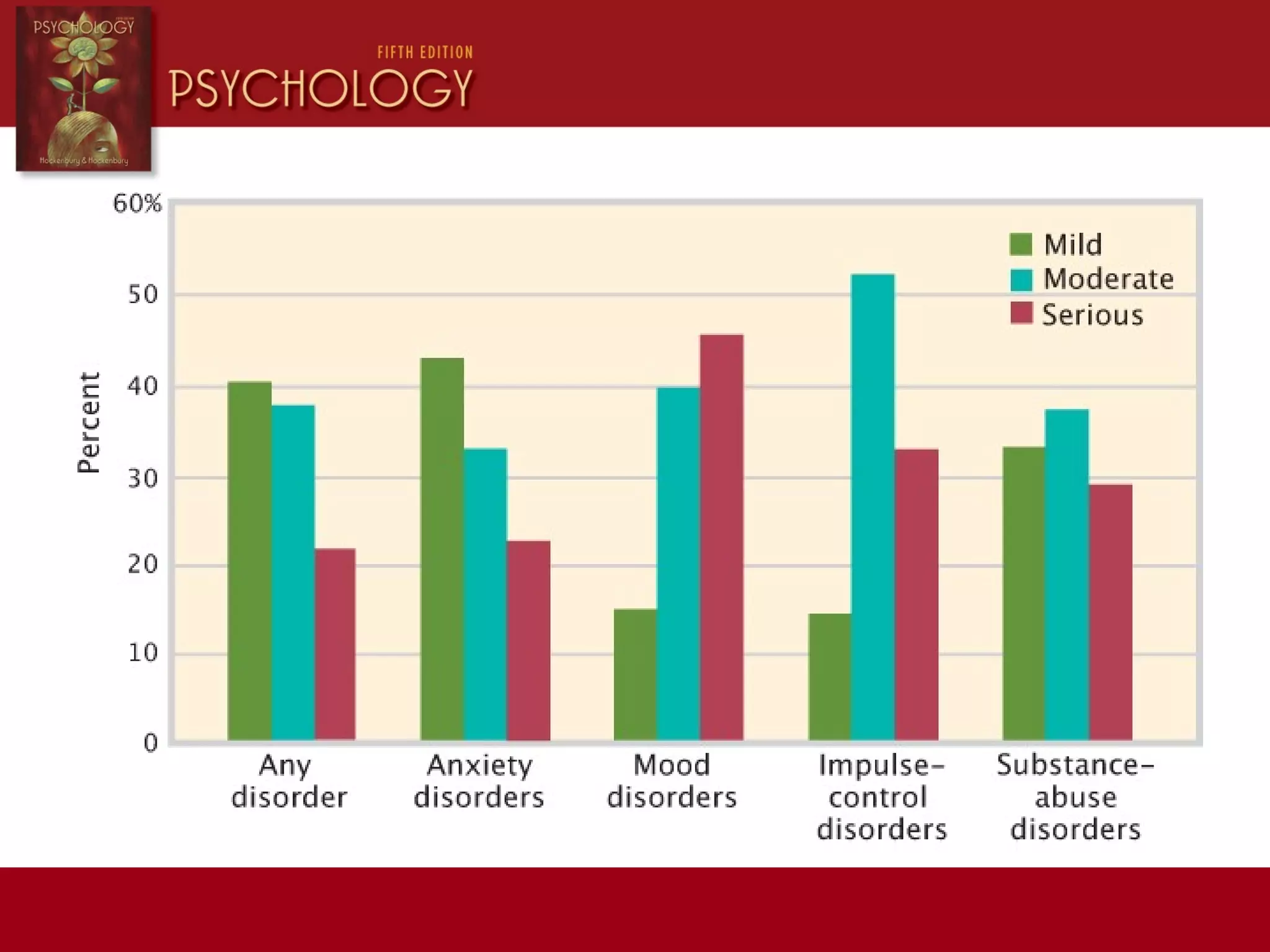
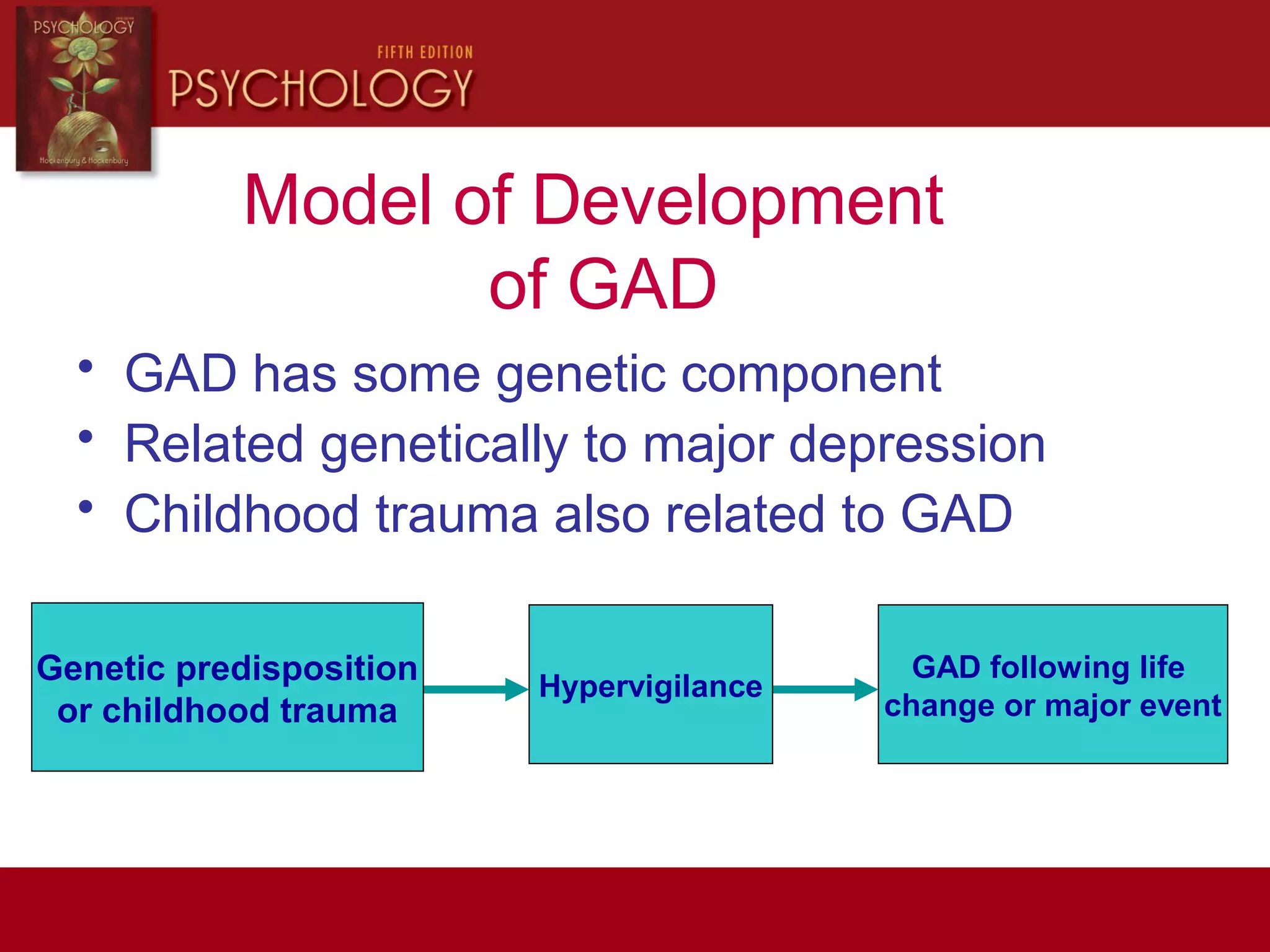
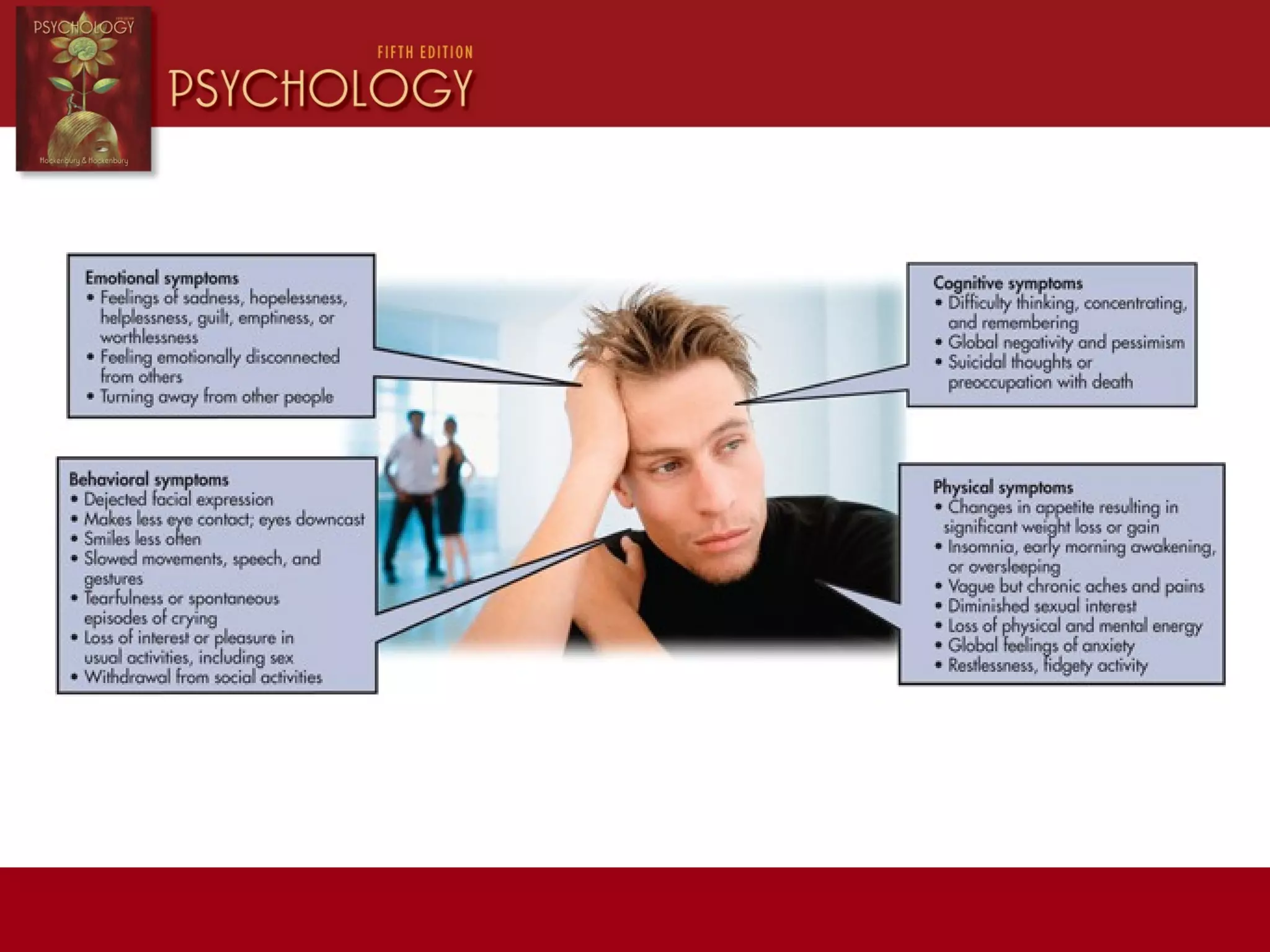
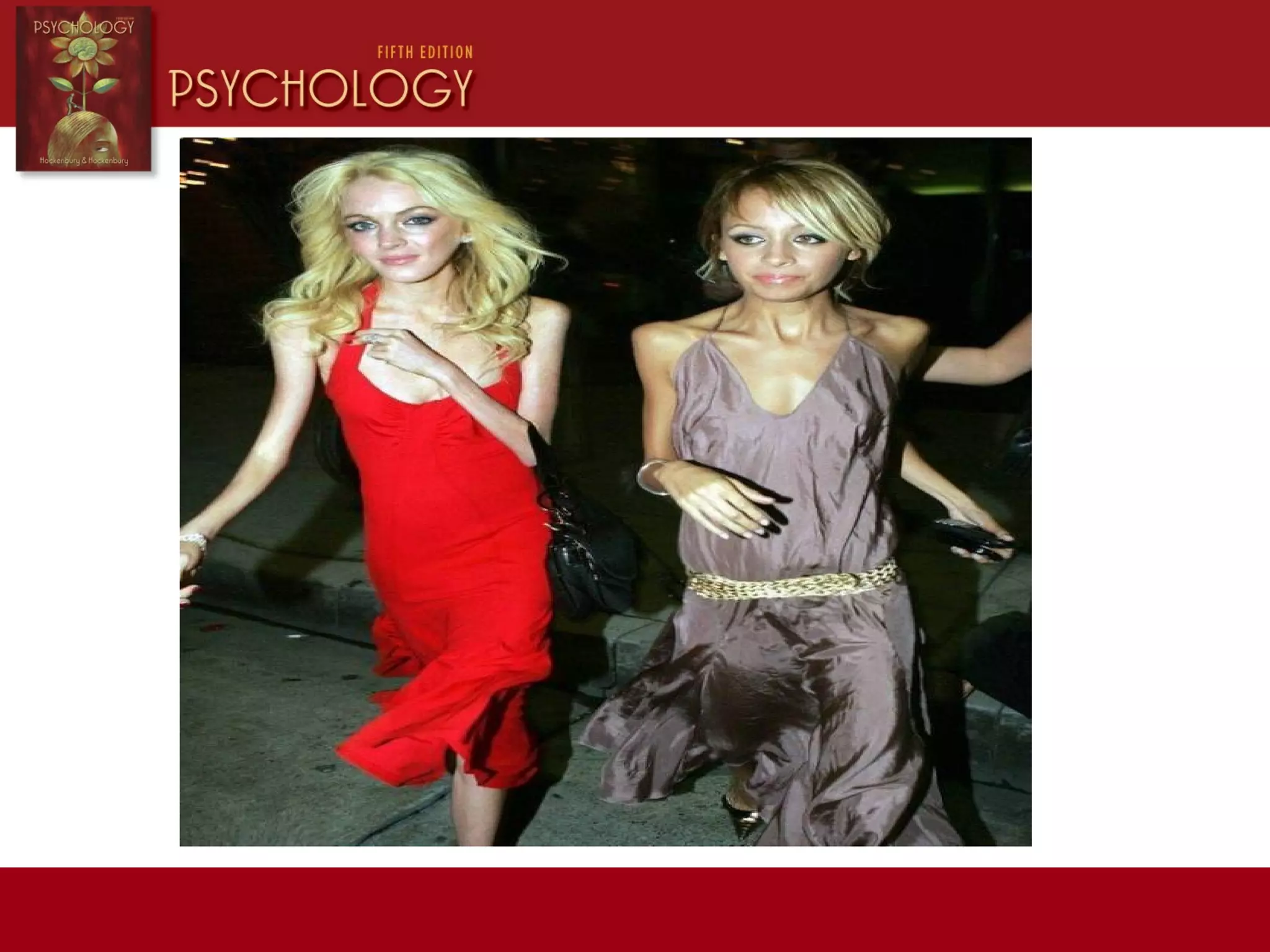
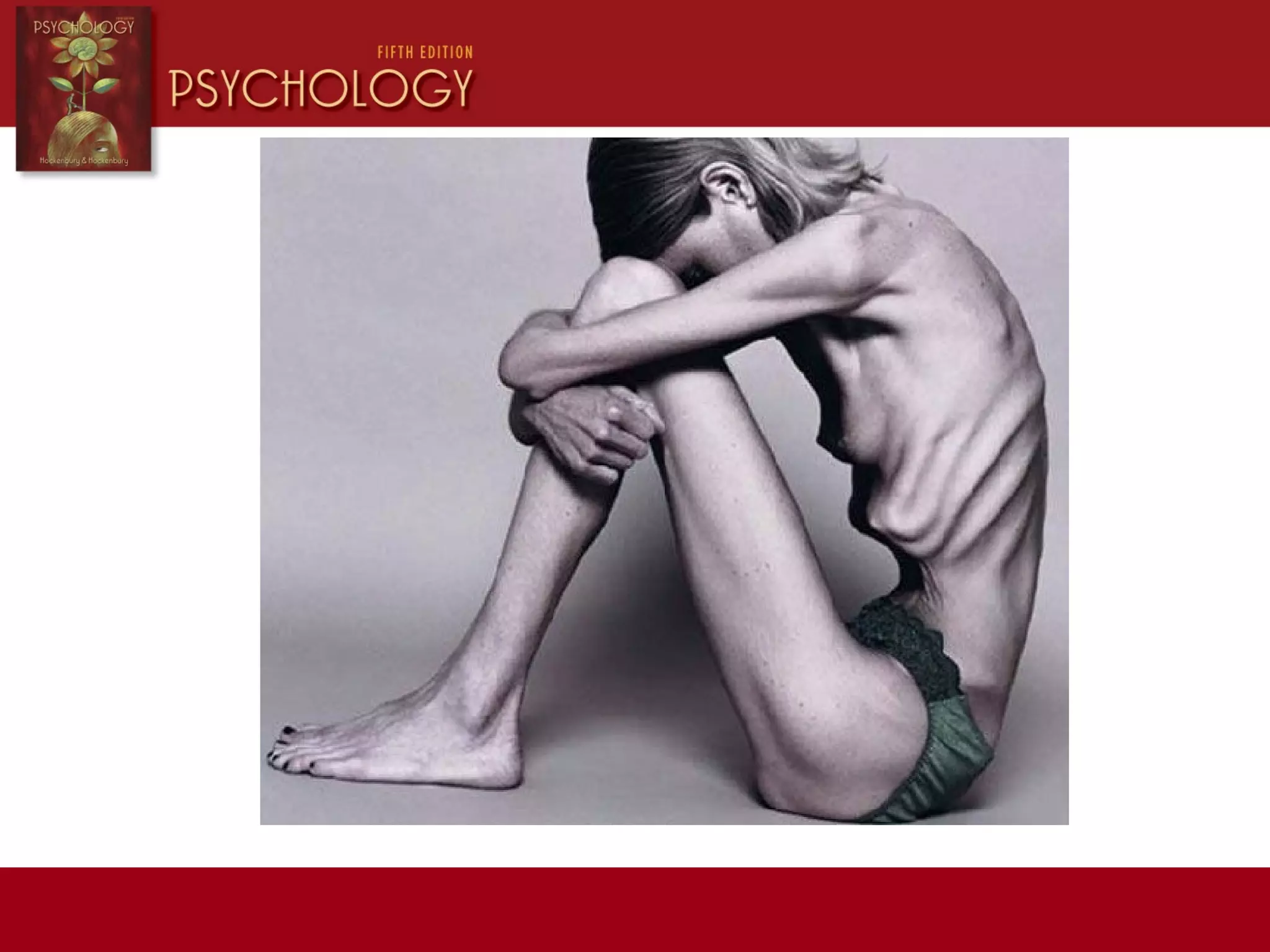
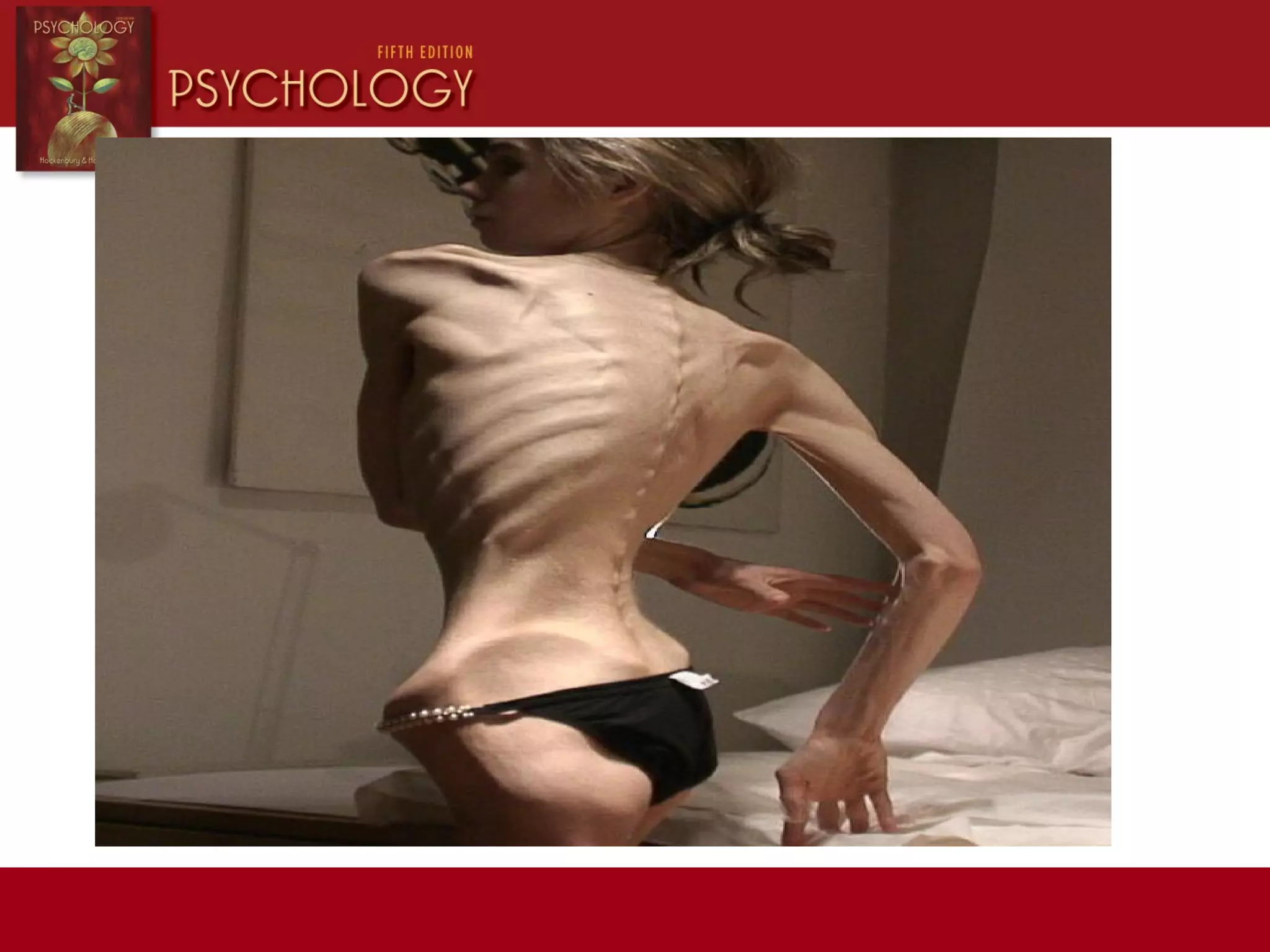
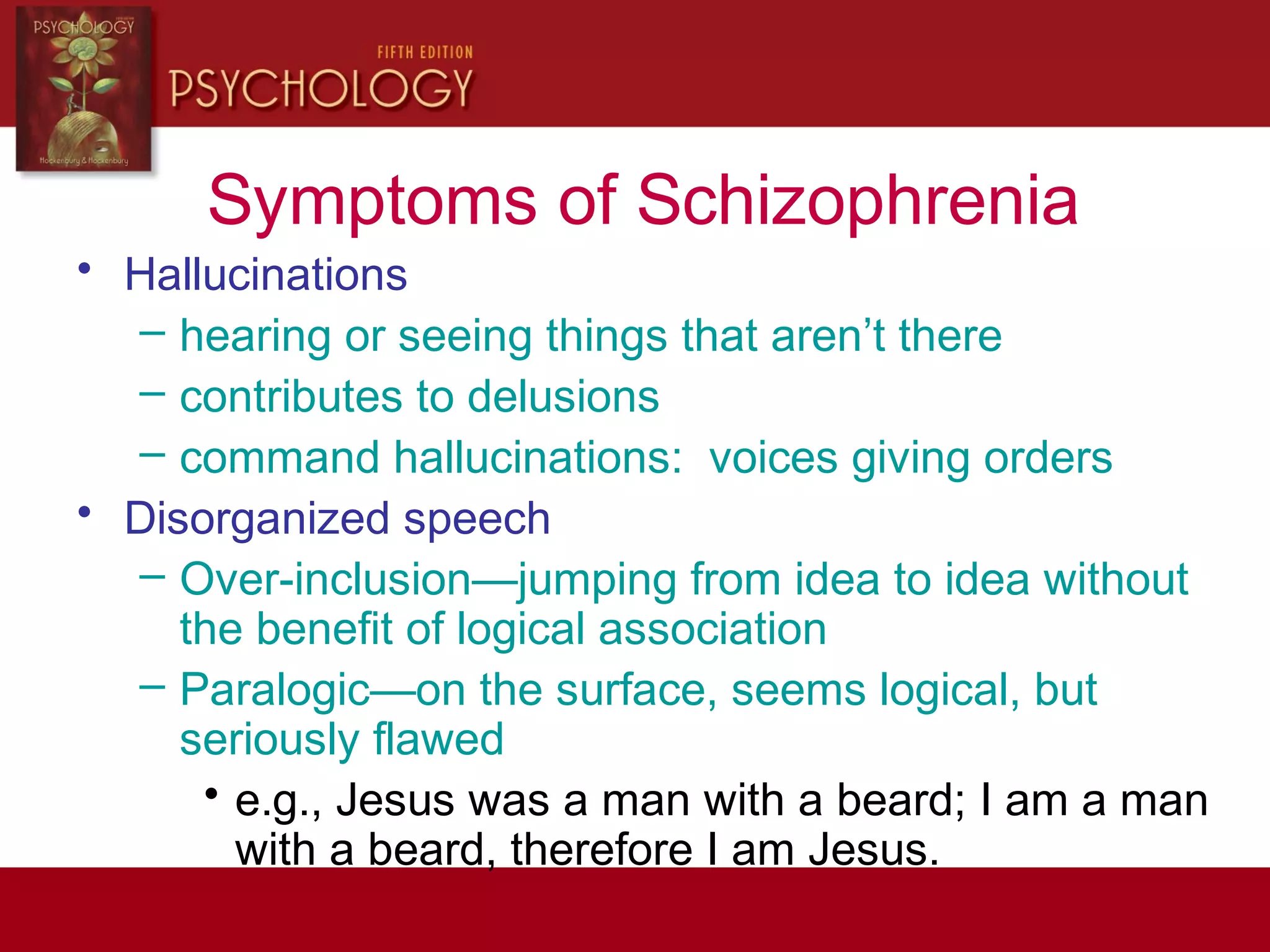
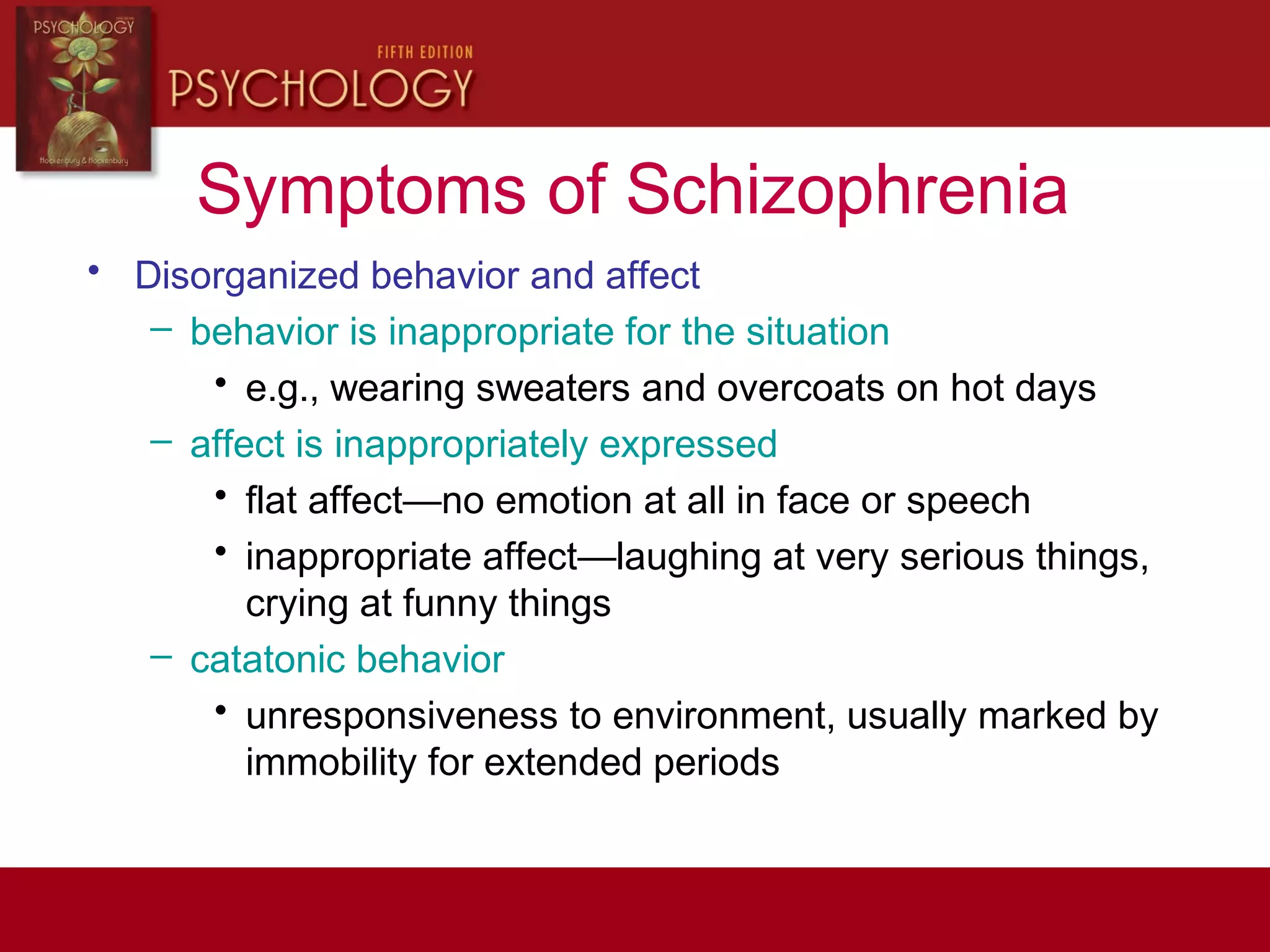
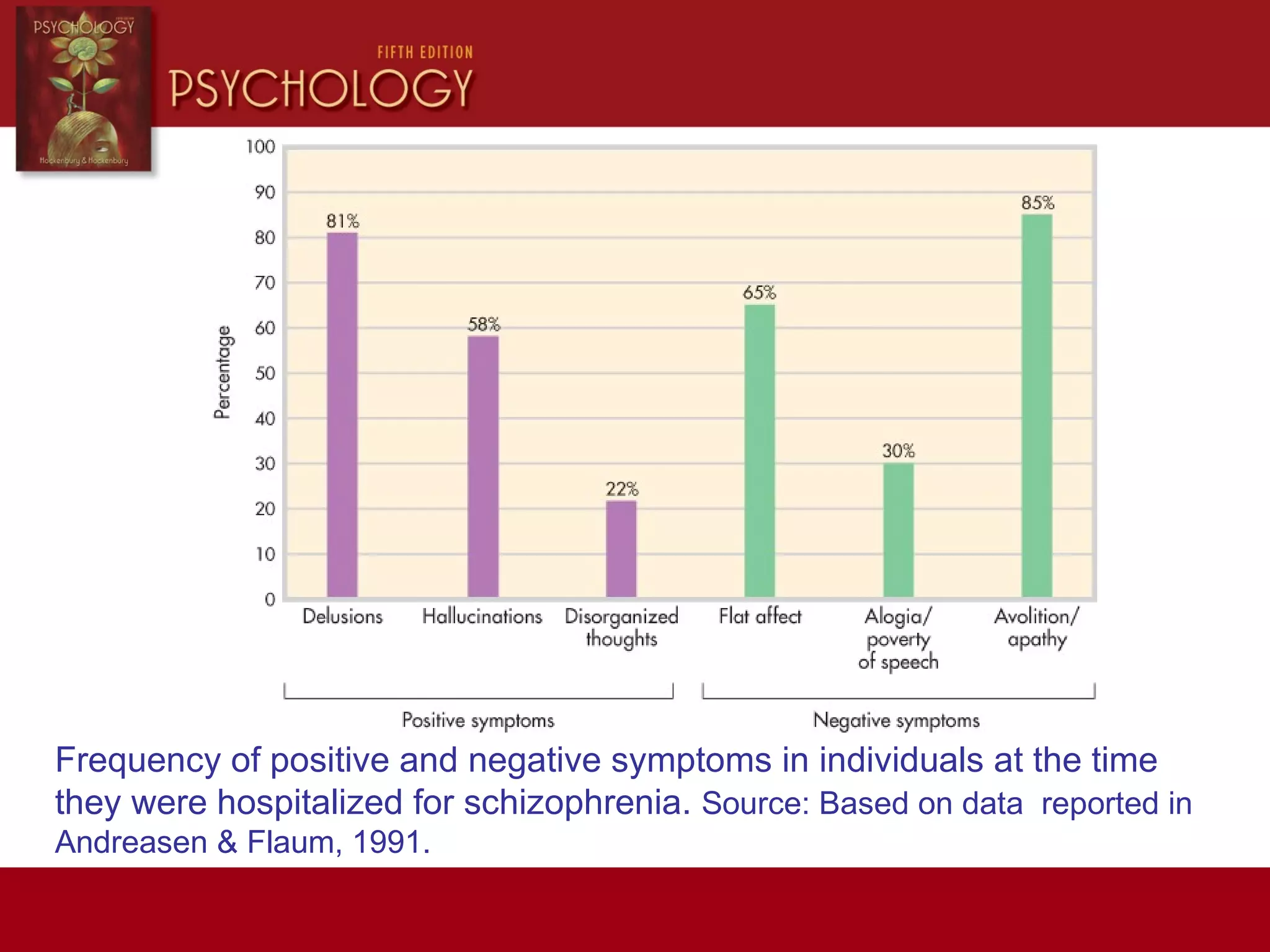
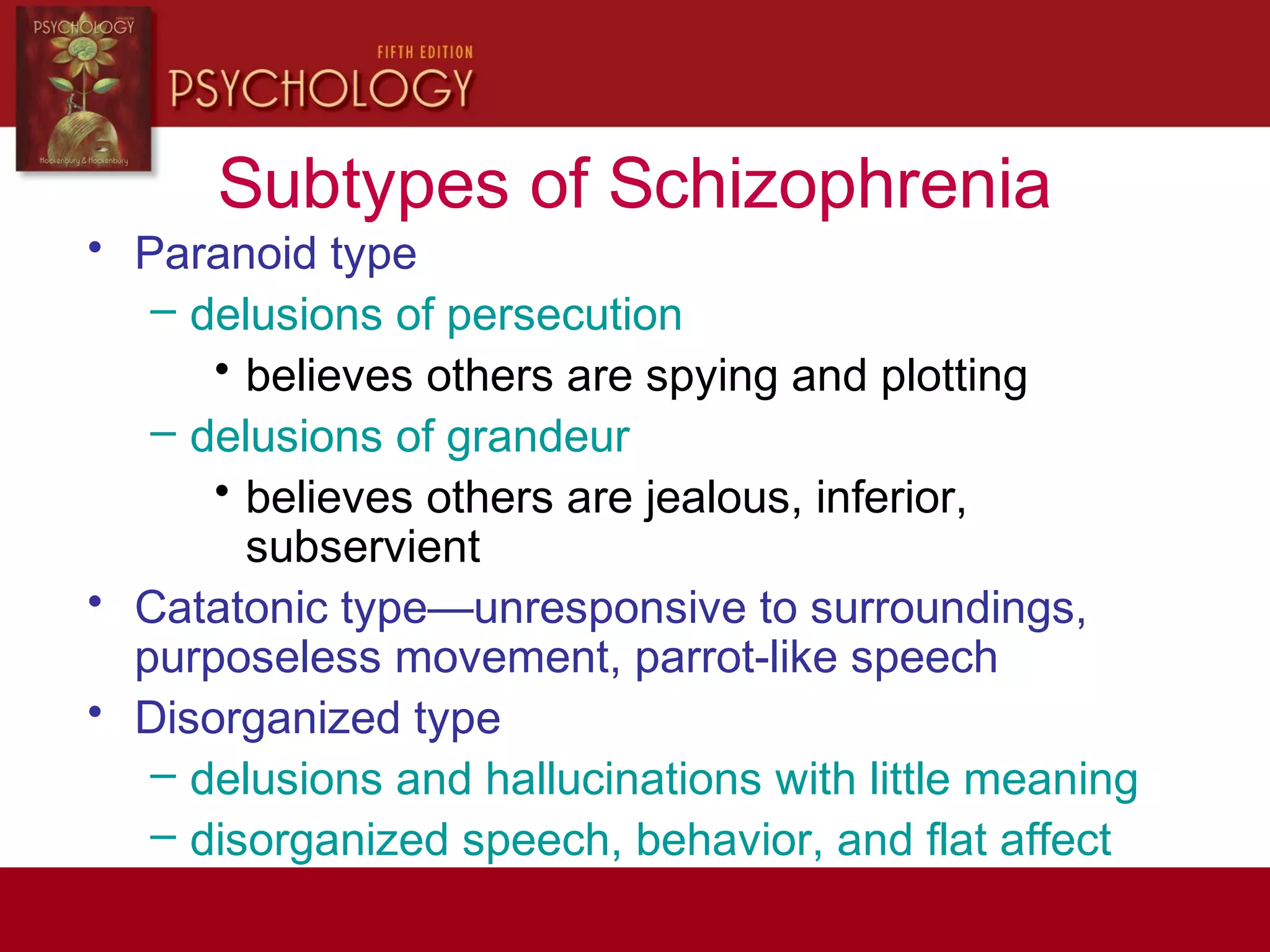
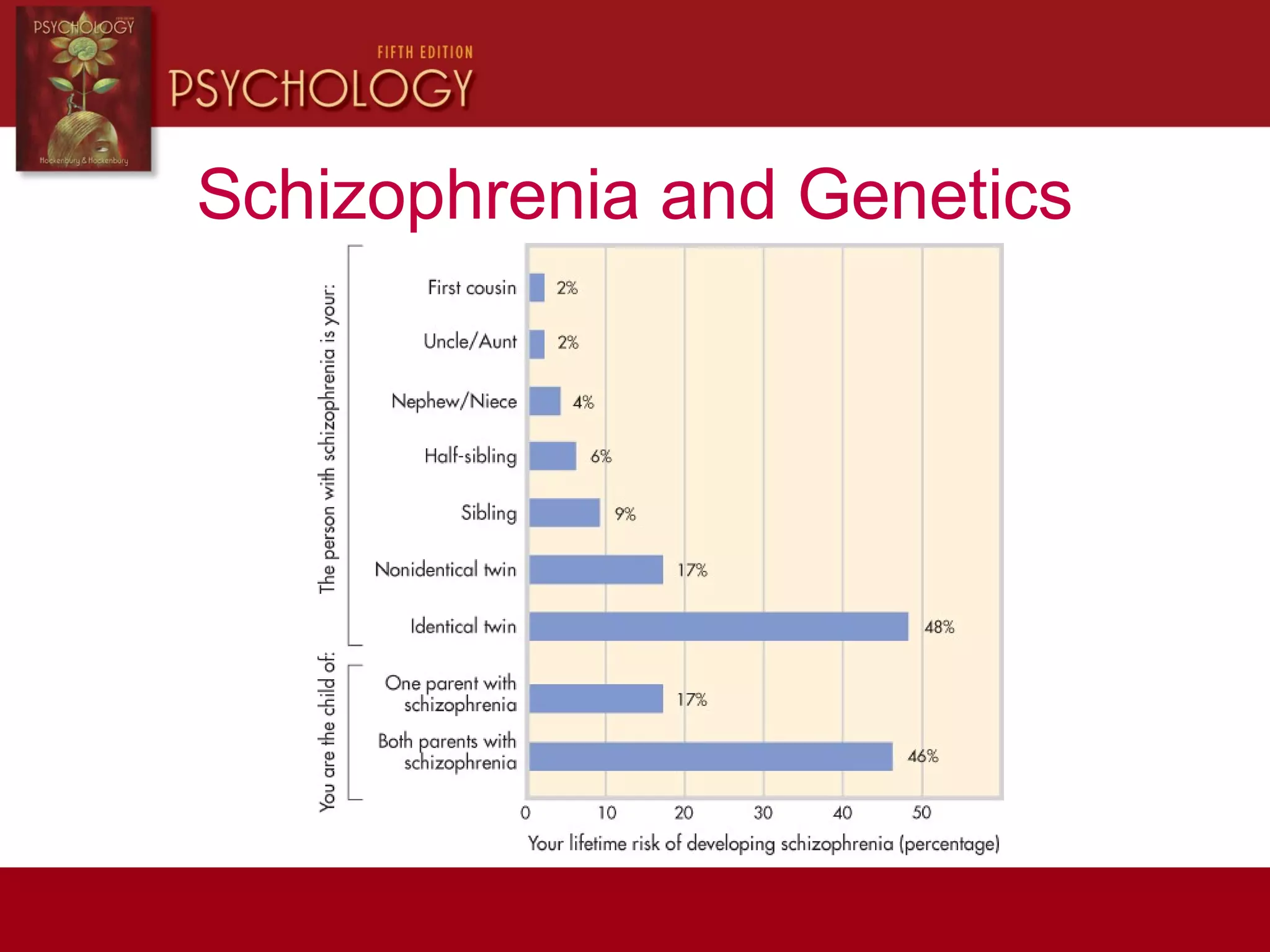
This document provides an overview of psychological disorders as described in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). It defines psychological disorders and discusses the DSM-IV-TR's role in diagnosis. It then summarizes several disorder categories and examples, prevalence of disorders, theories of anxiety, mood, eating, personality, dissociative, and schizophrenia disorders, and their potential causes.