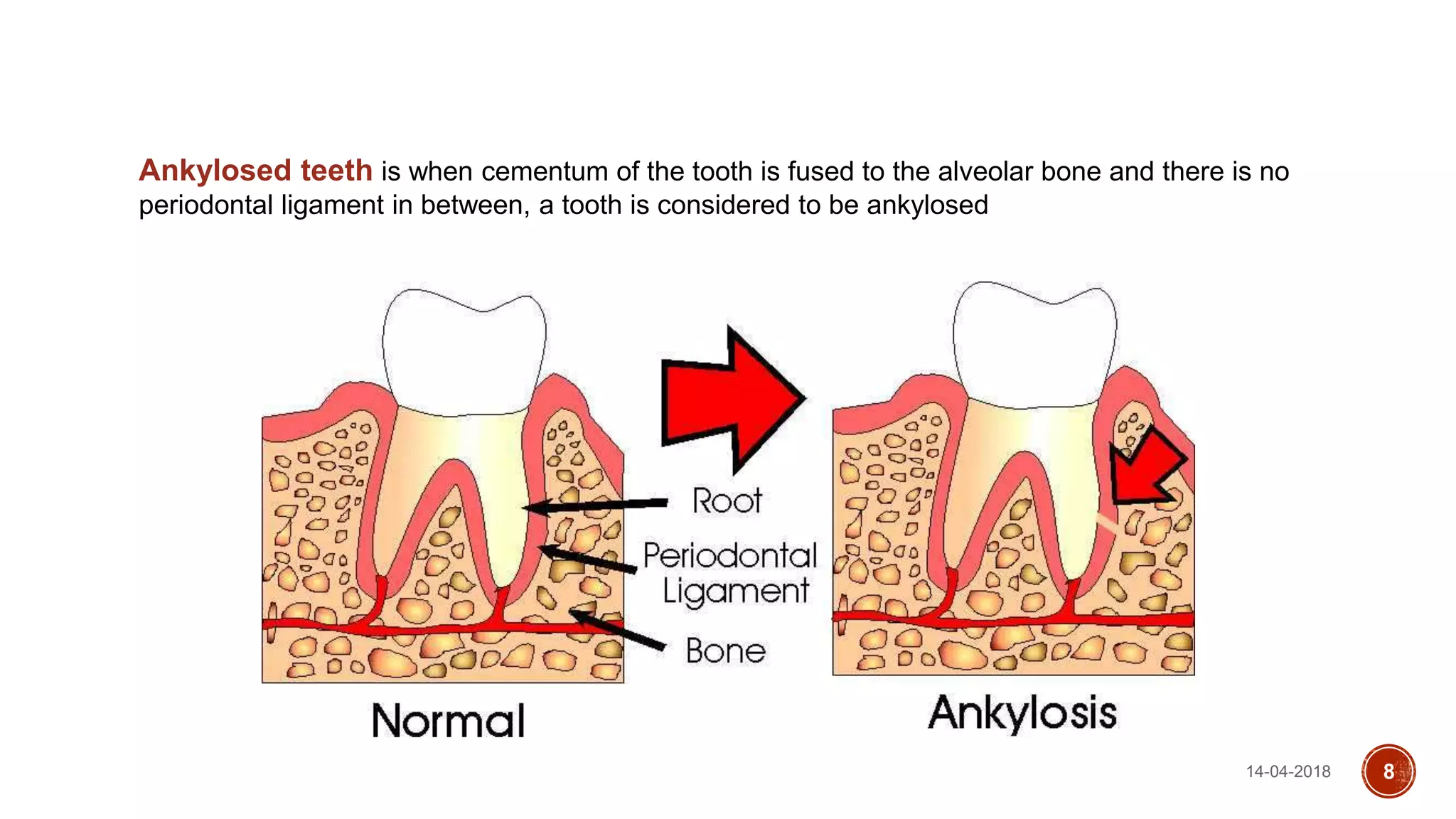
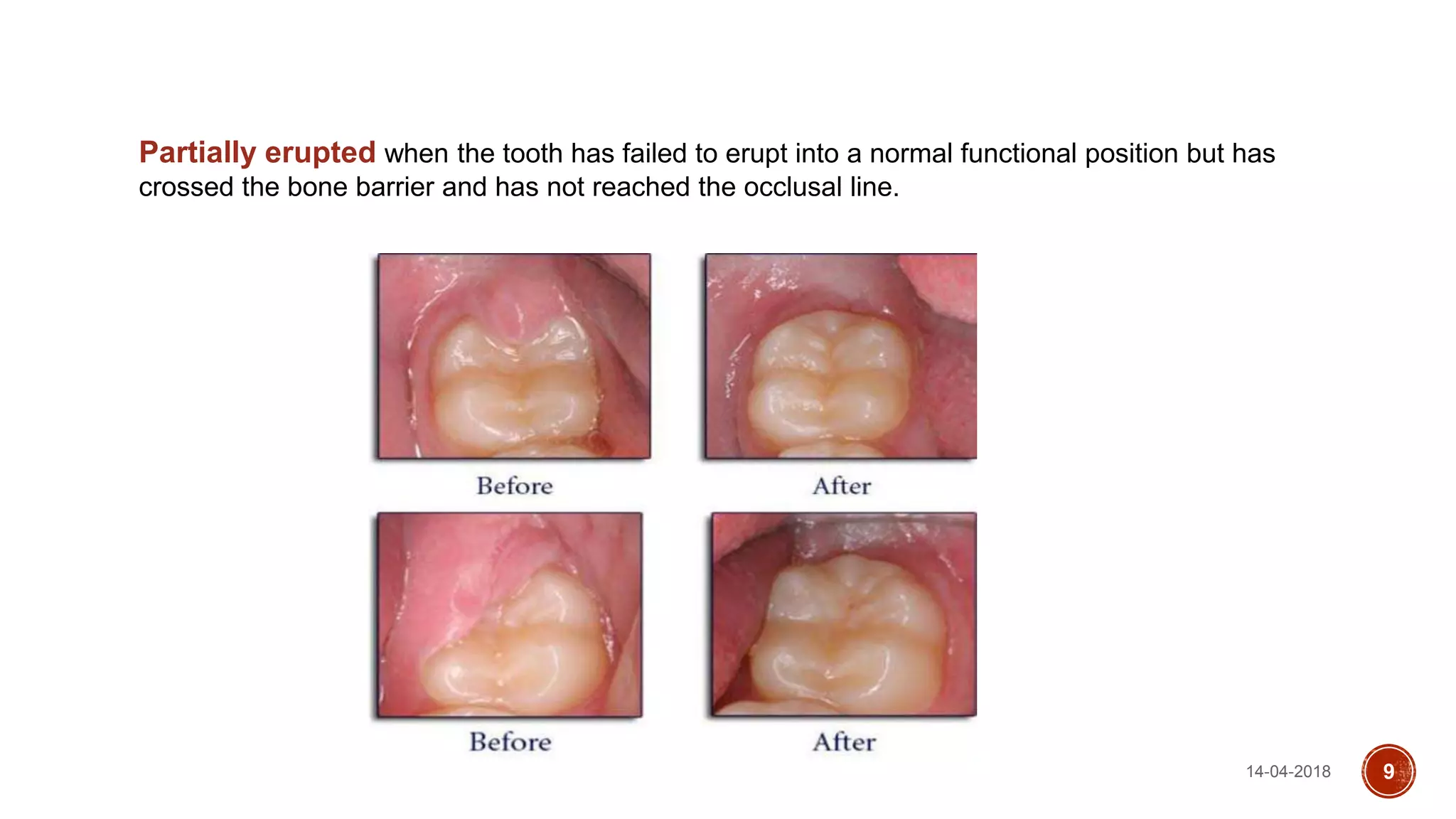
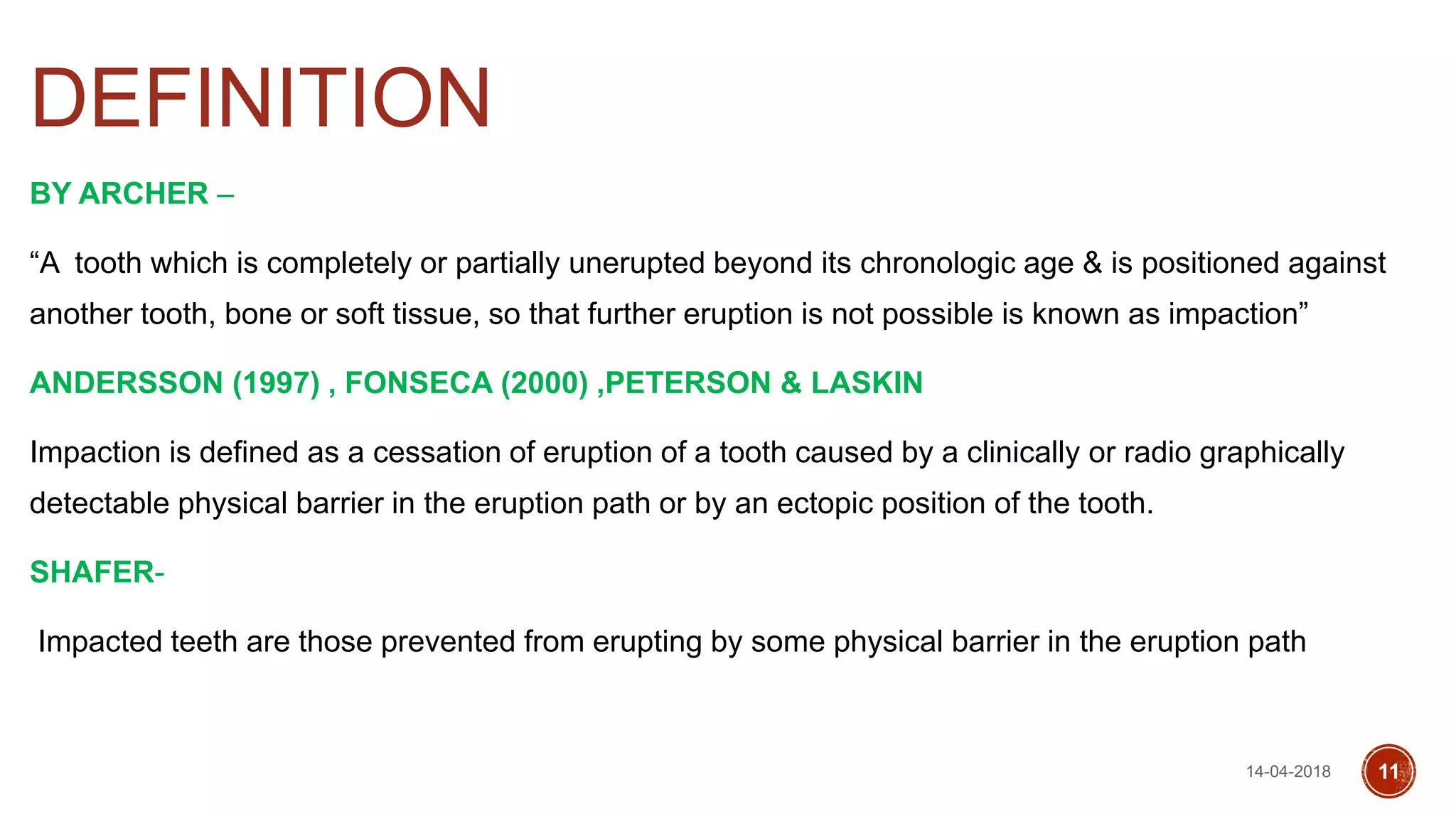
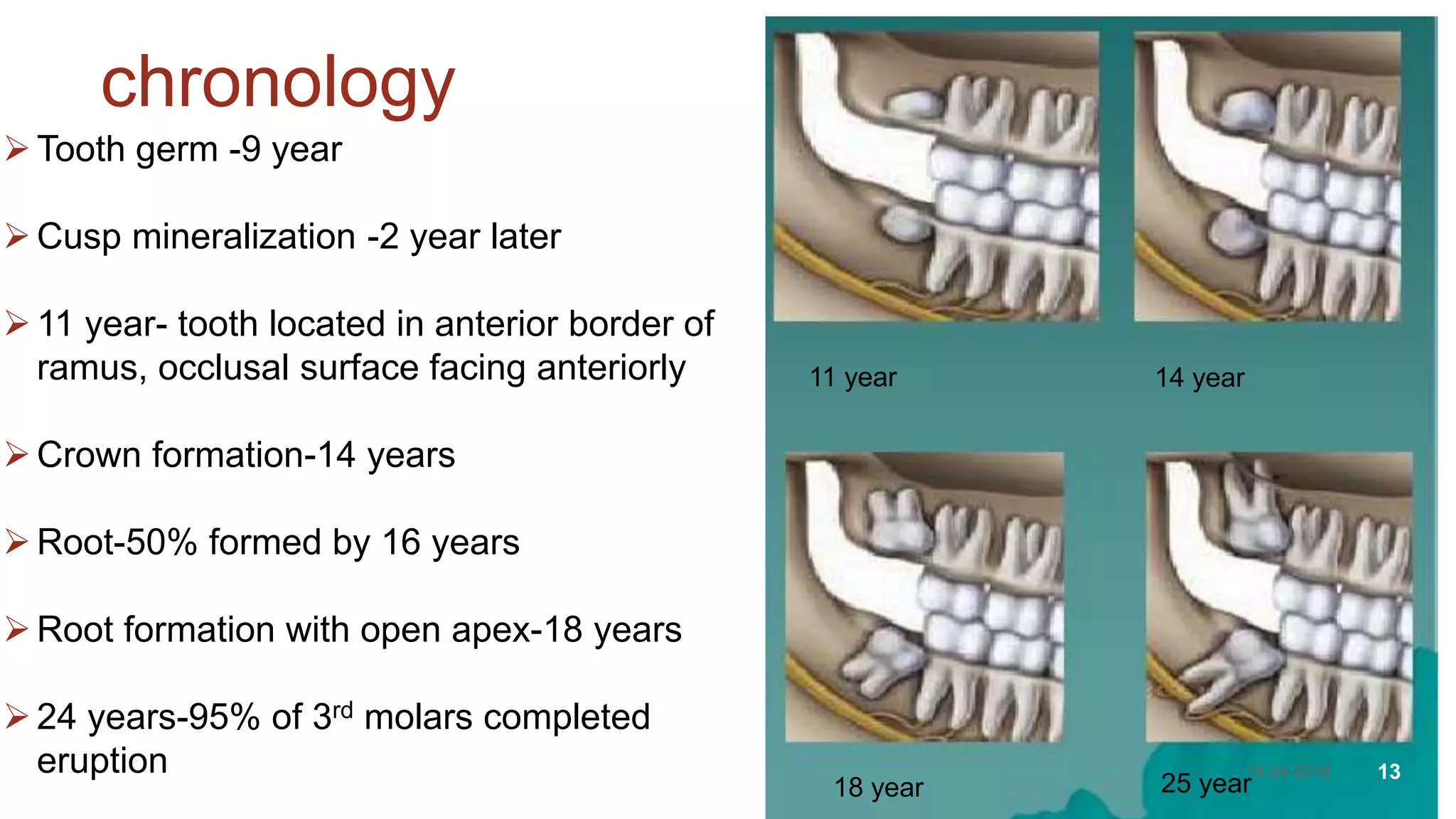
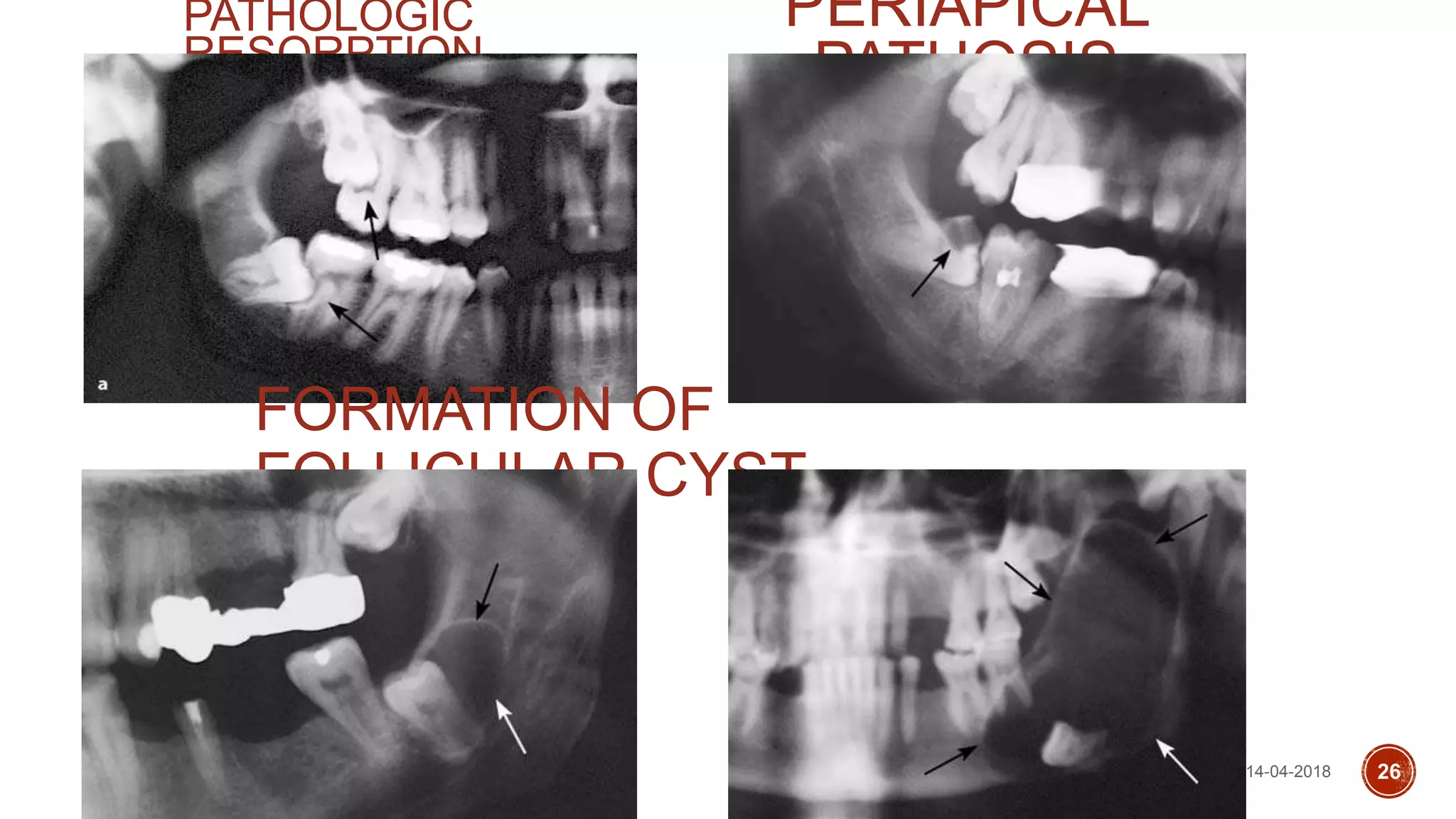
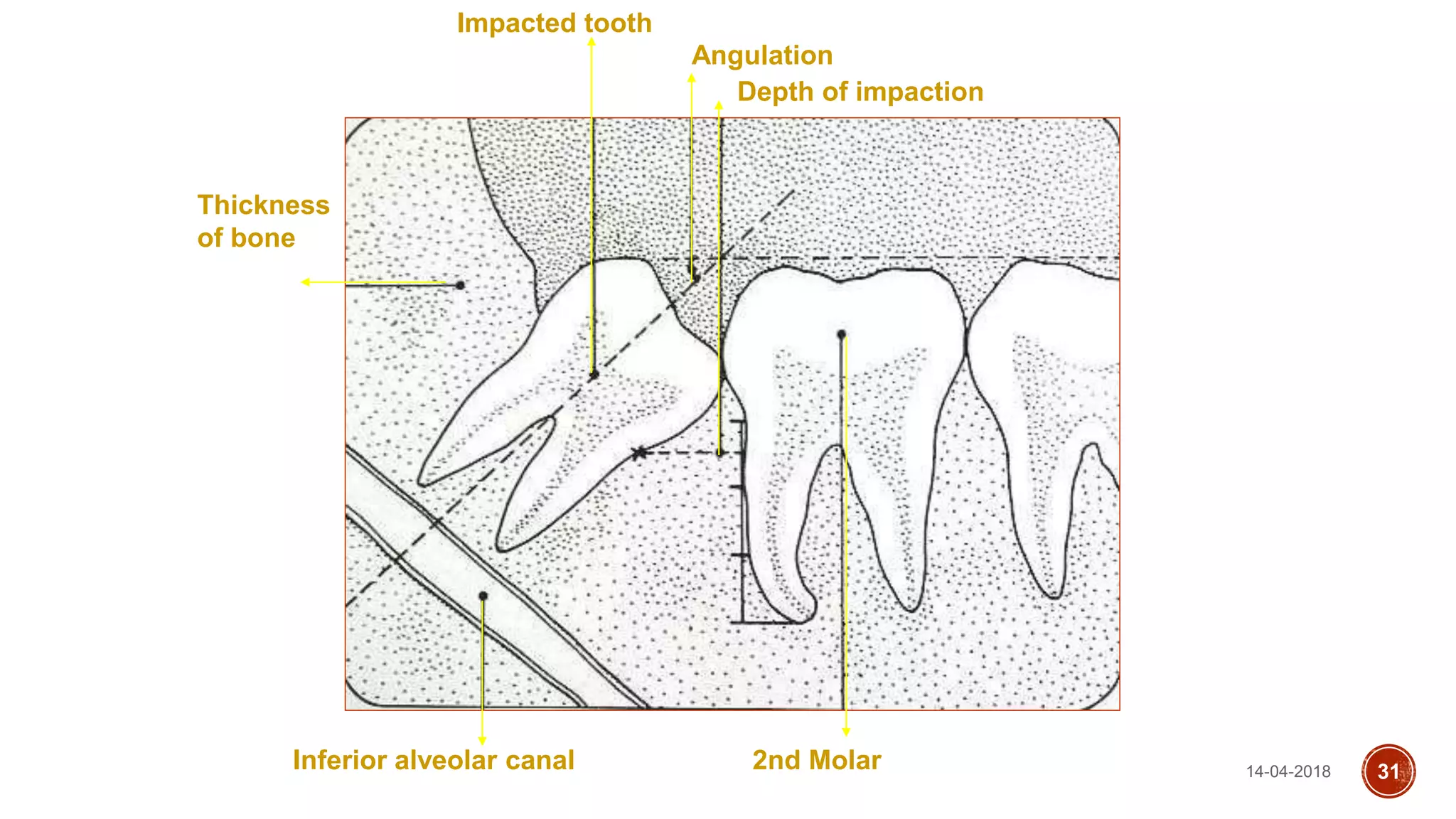
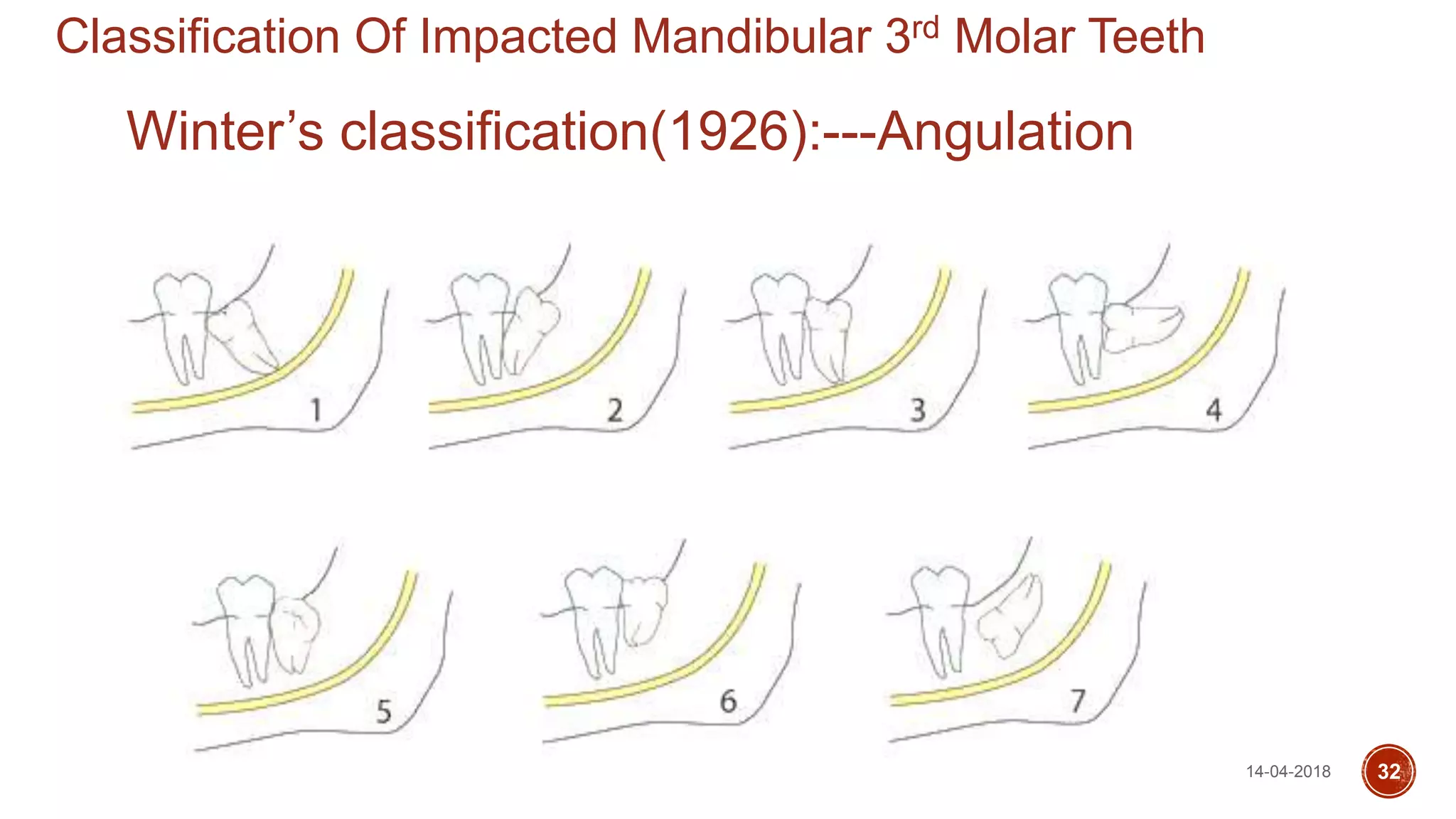
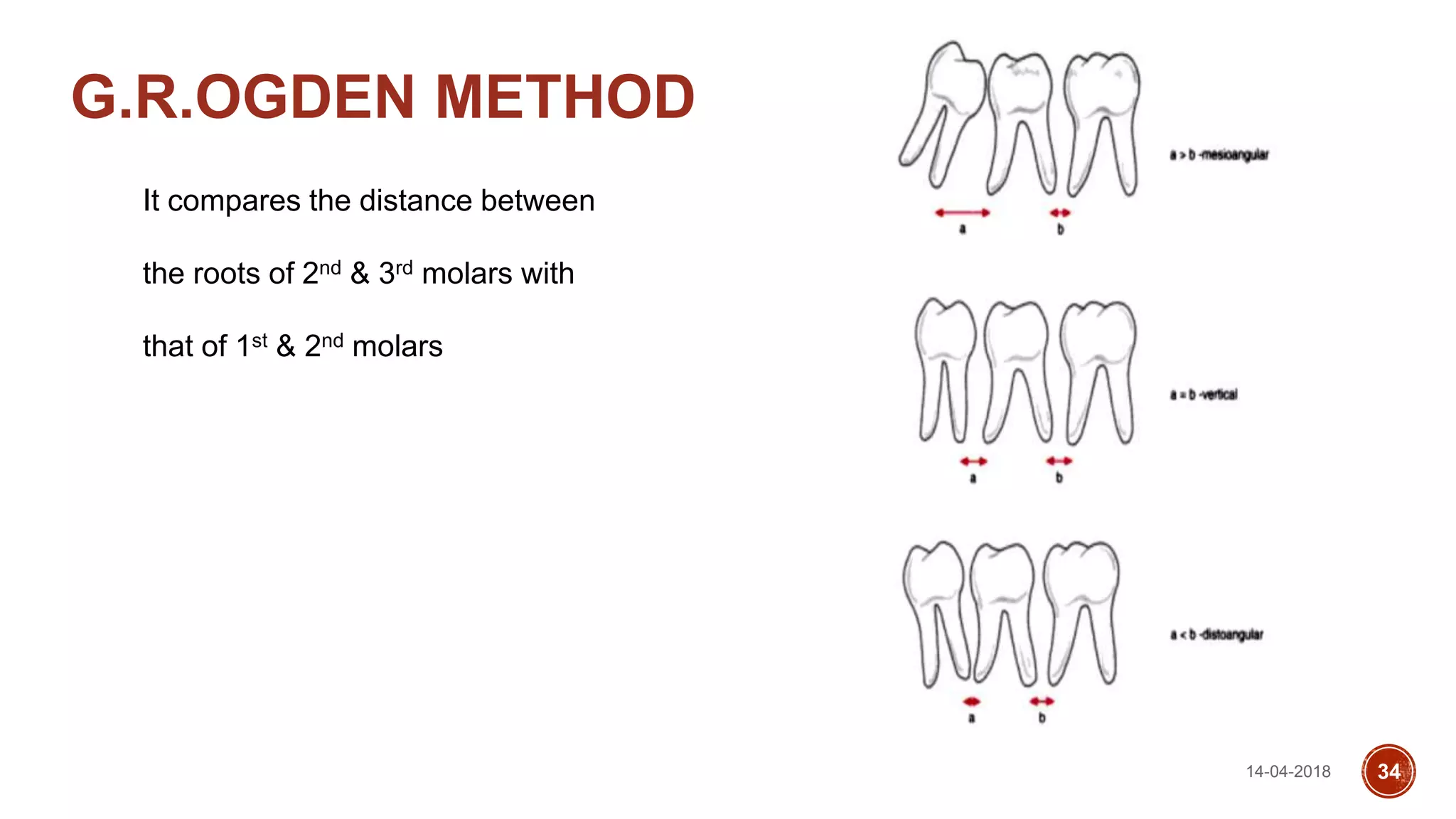
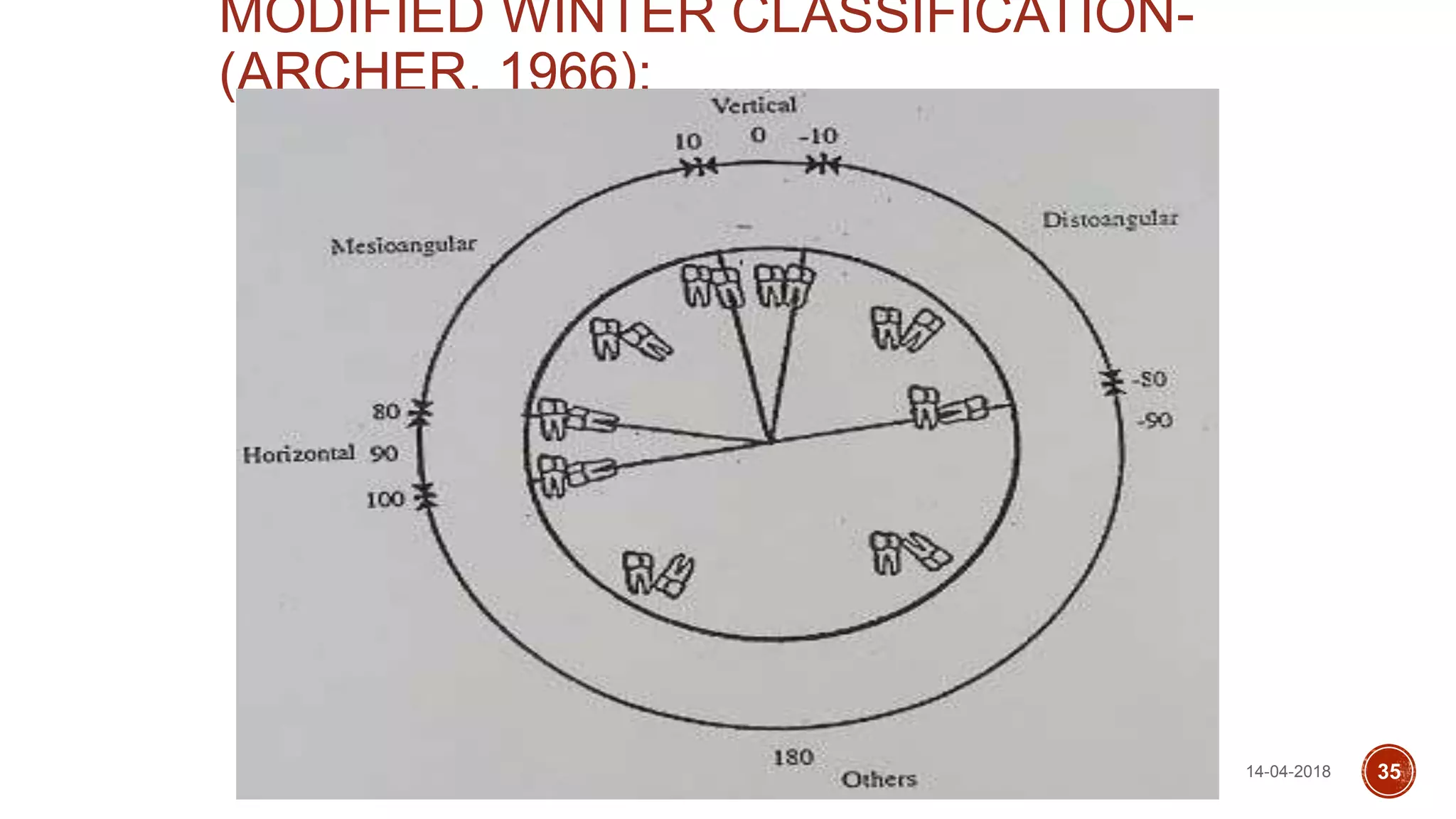
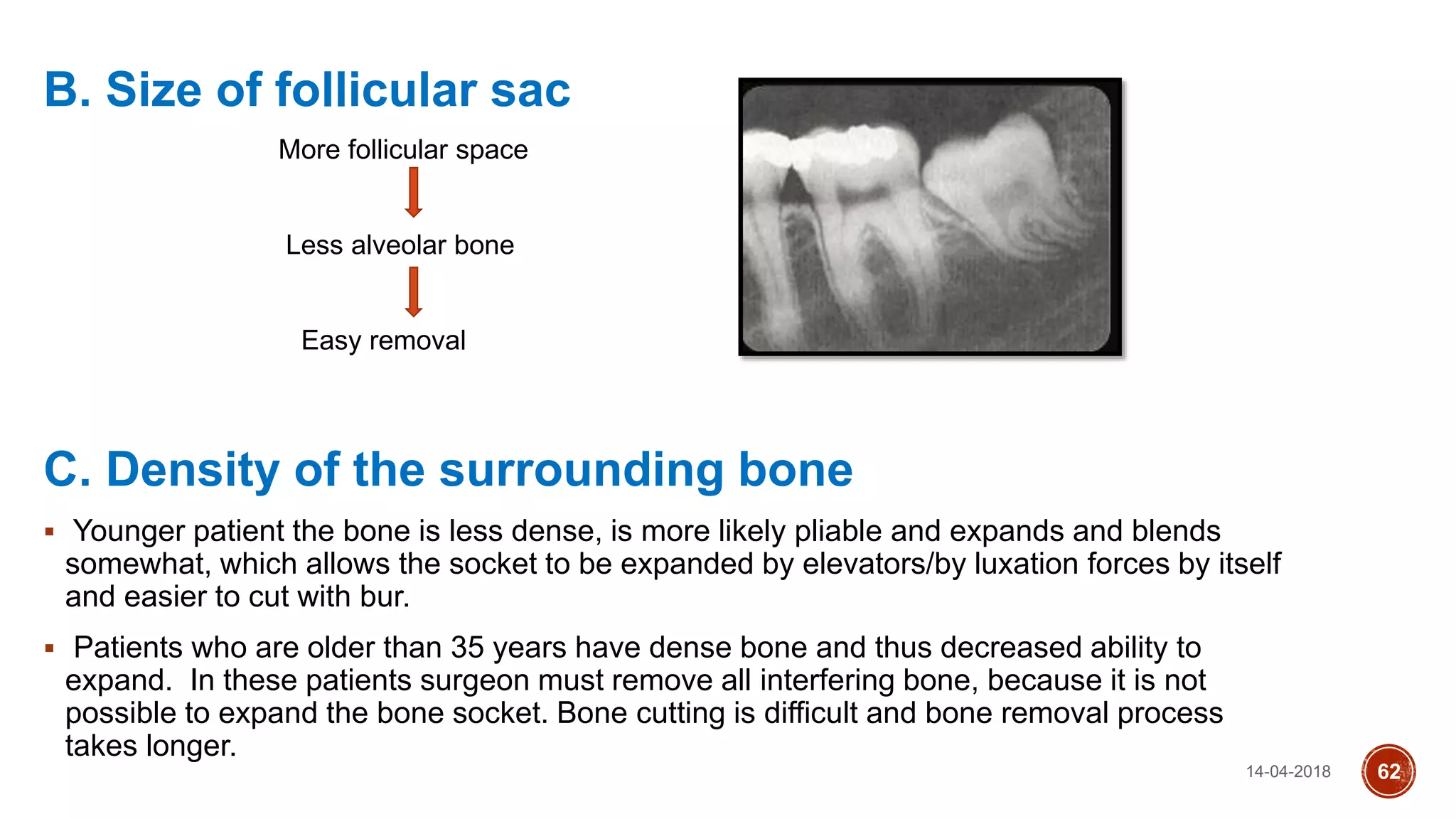
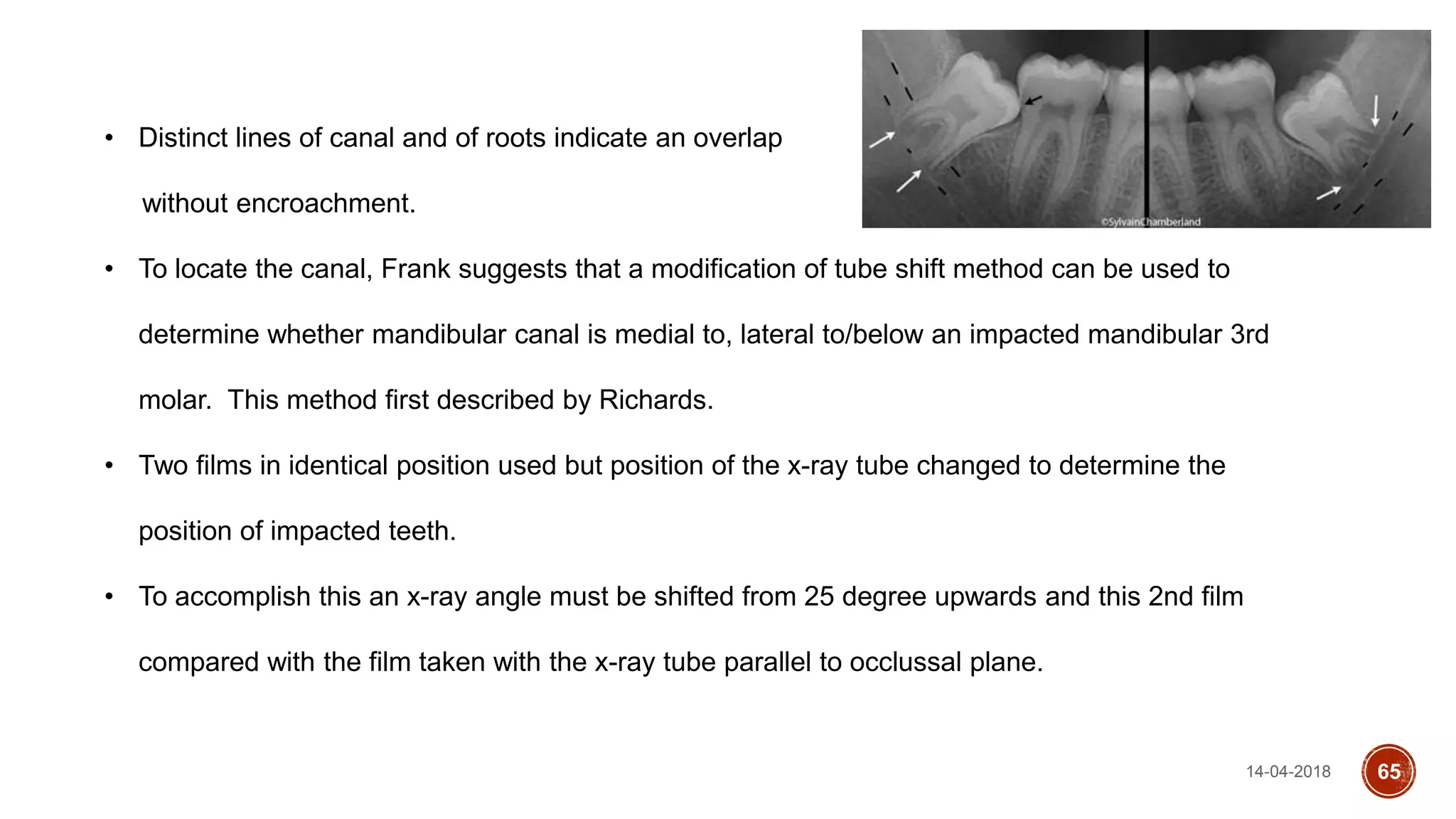
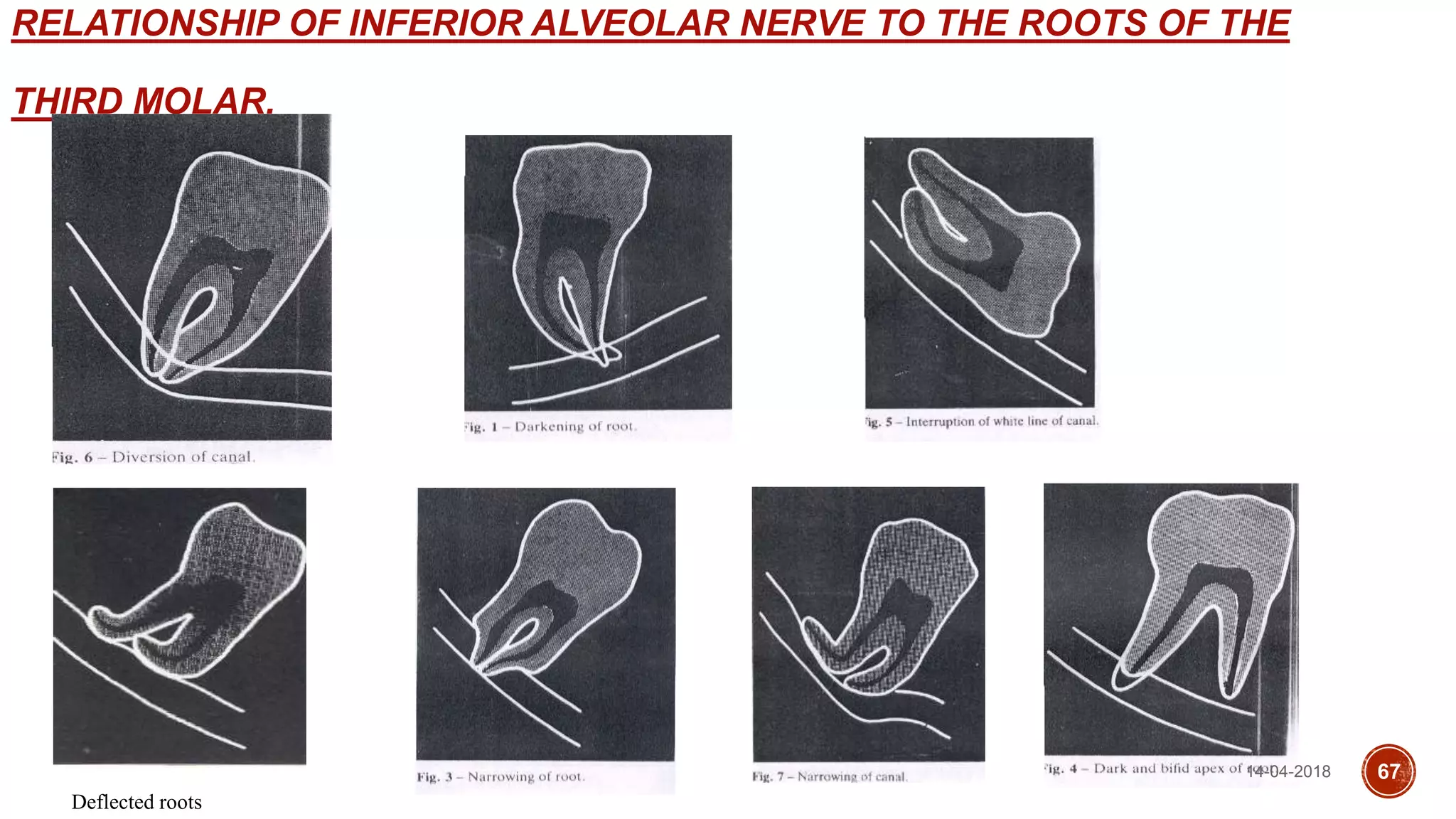
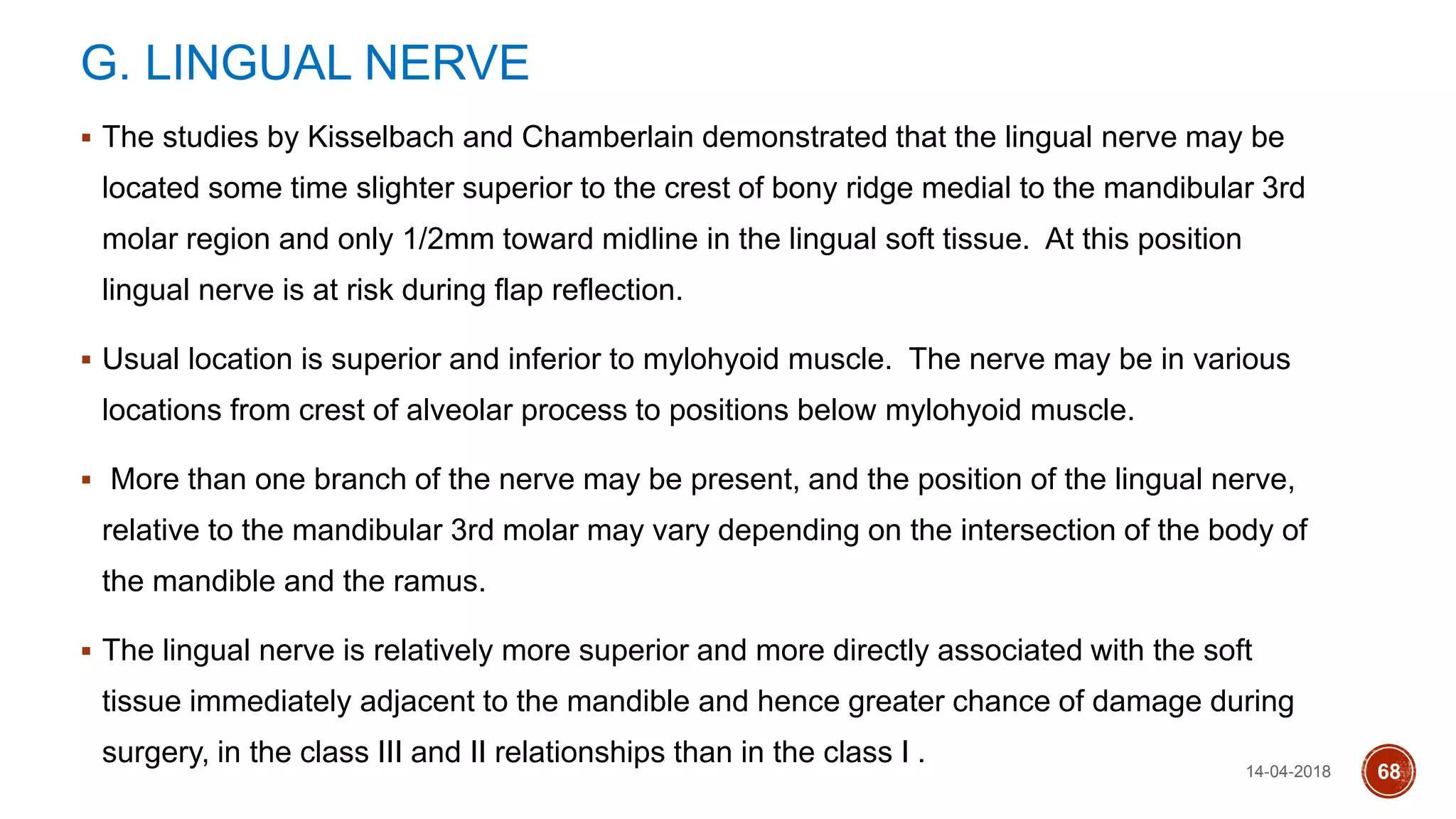
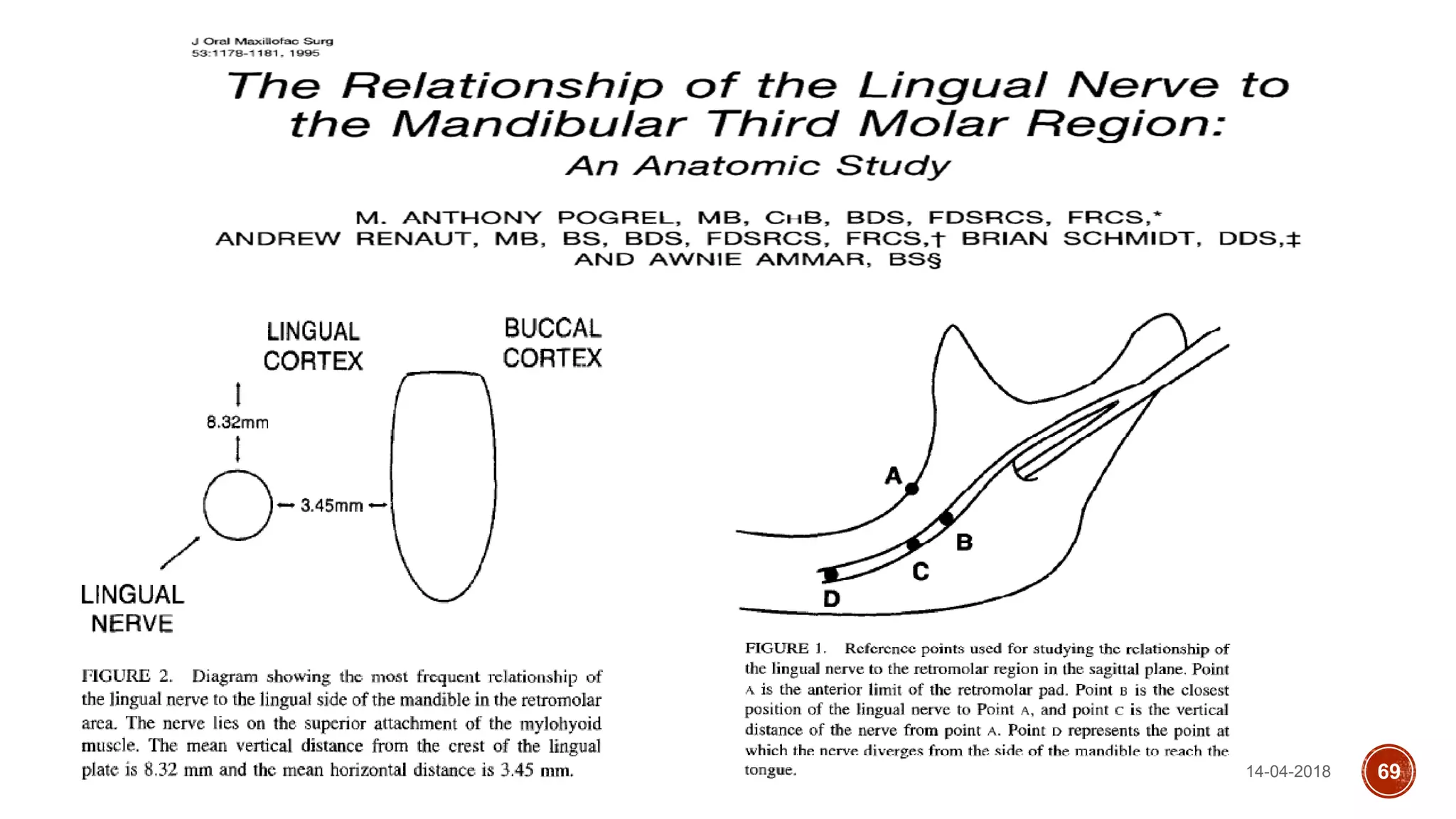
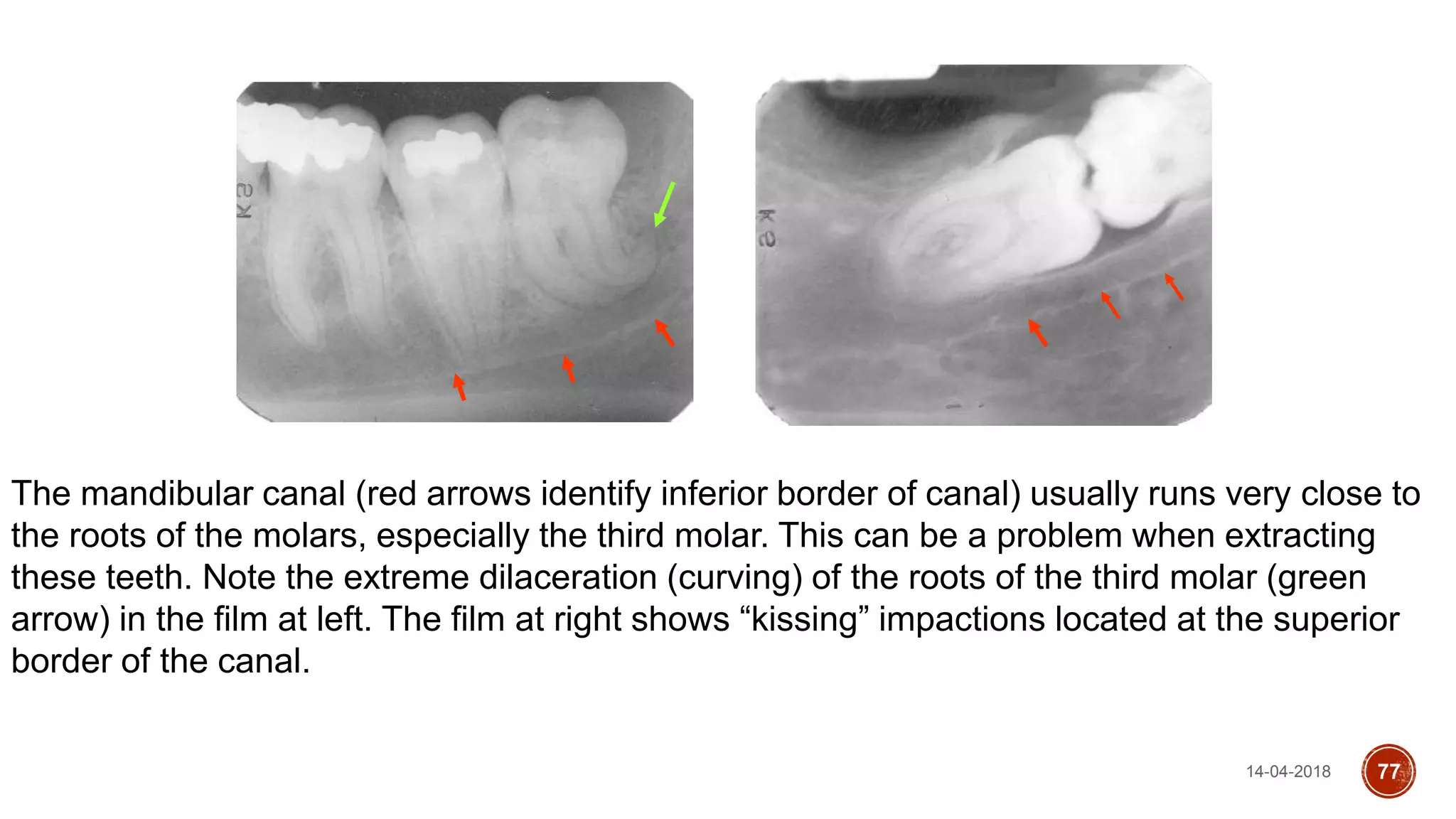
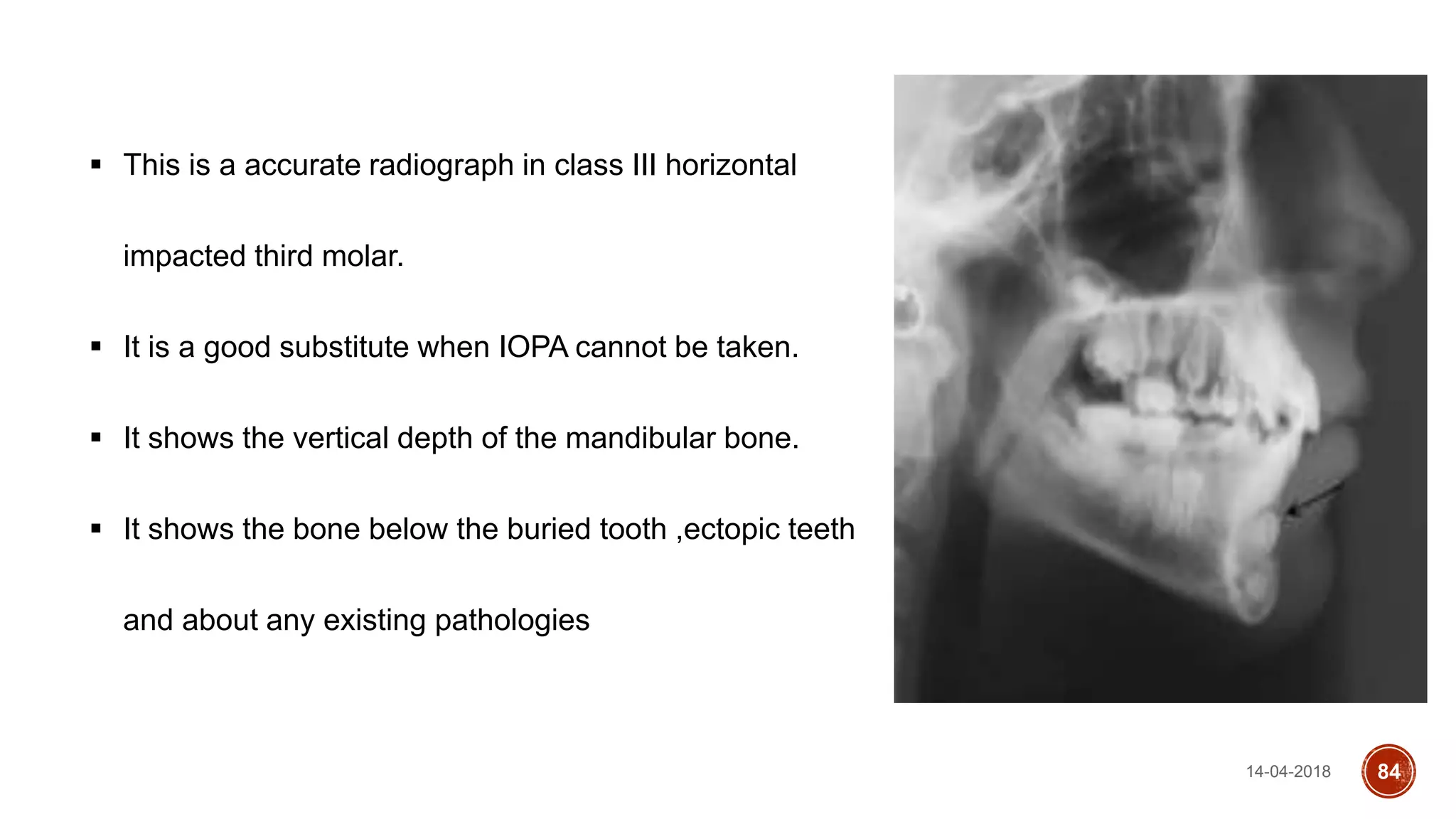
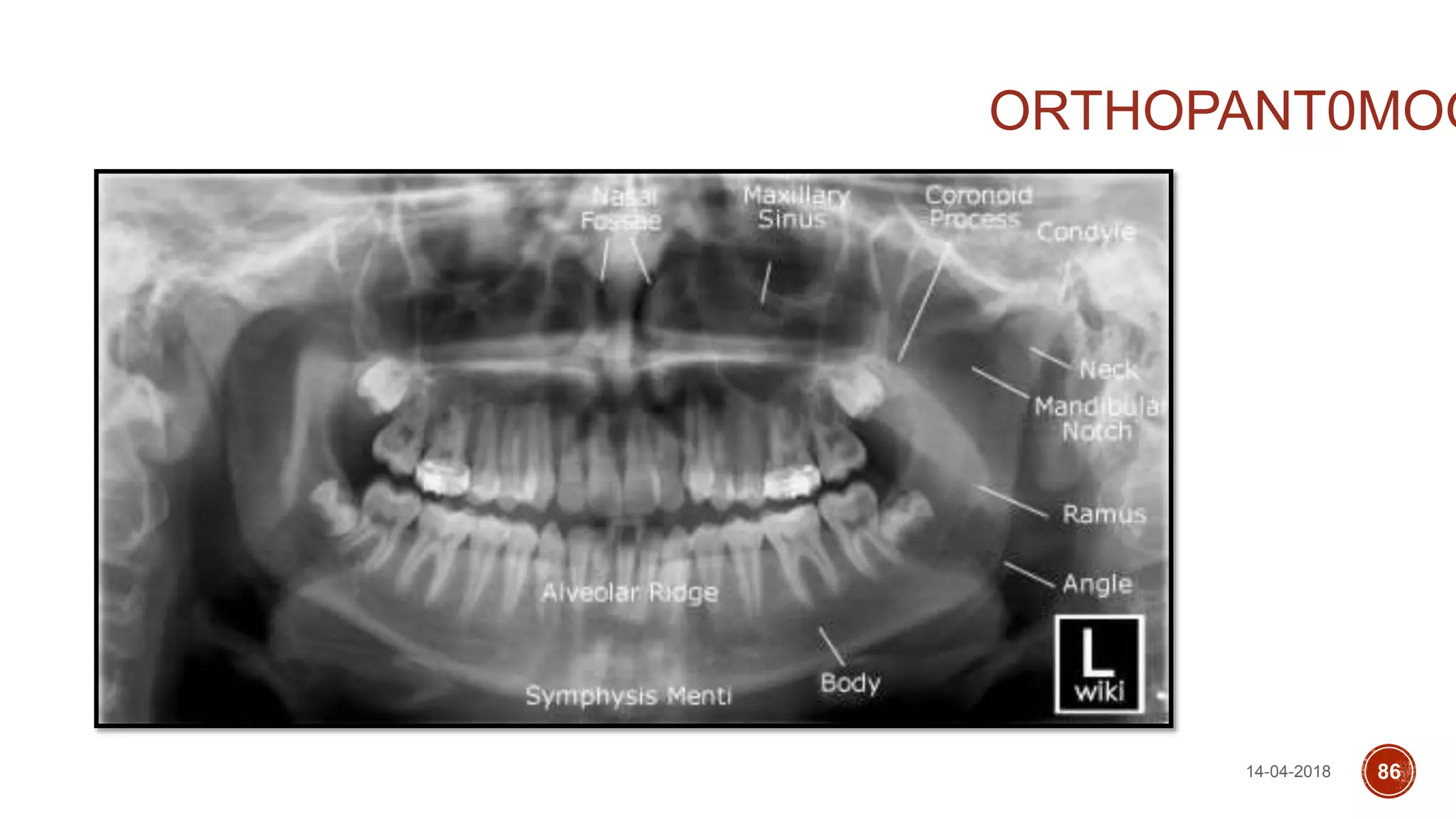
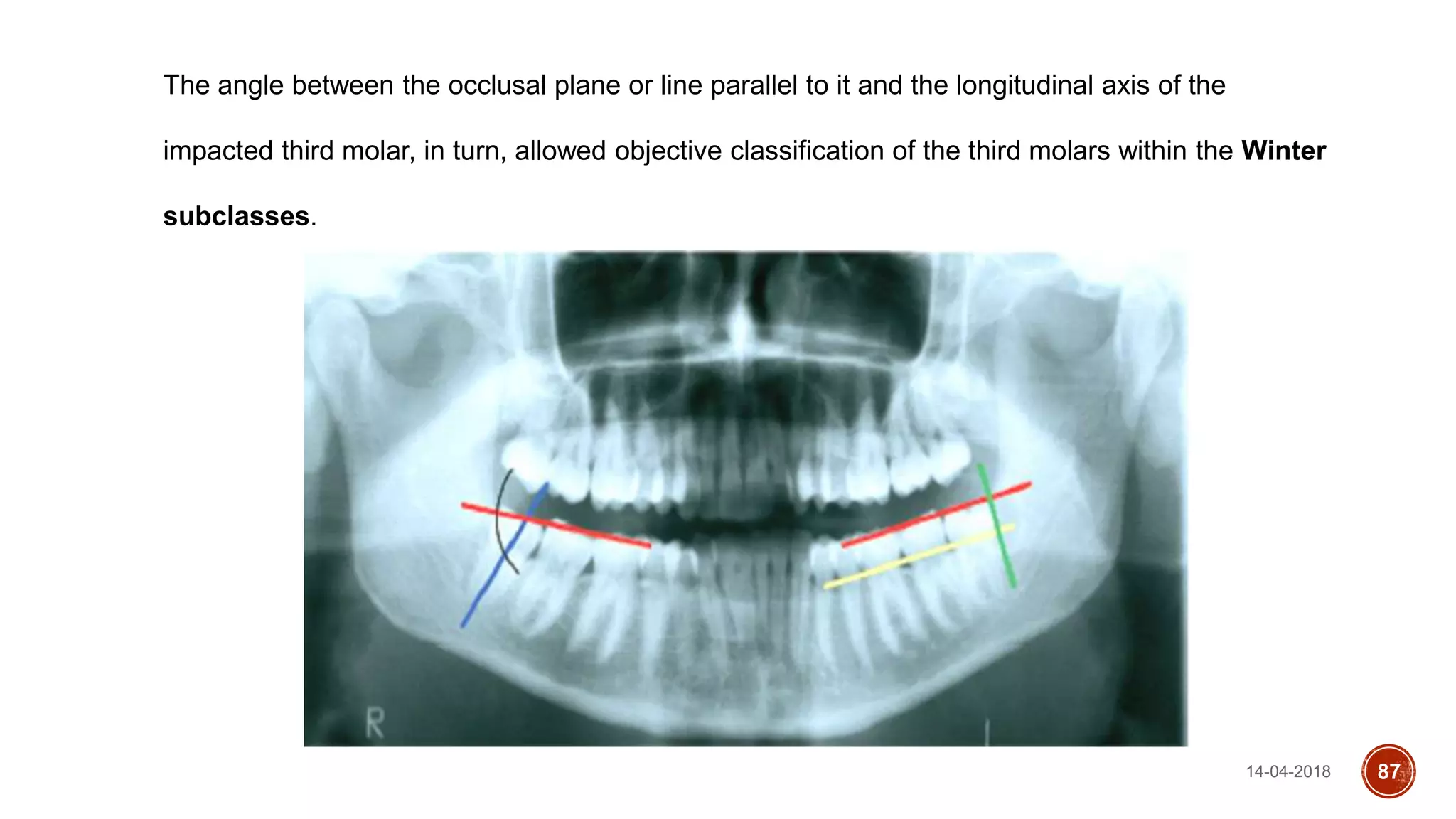
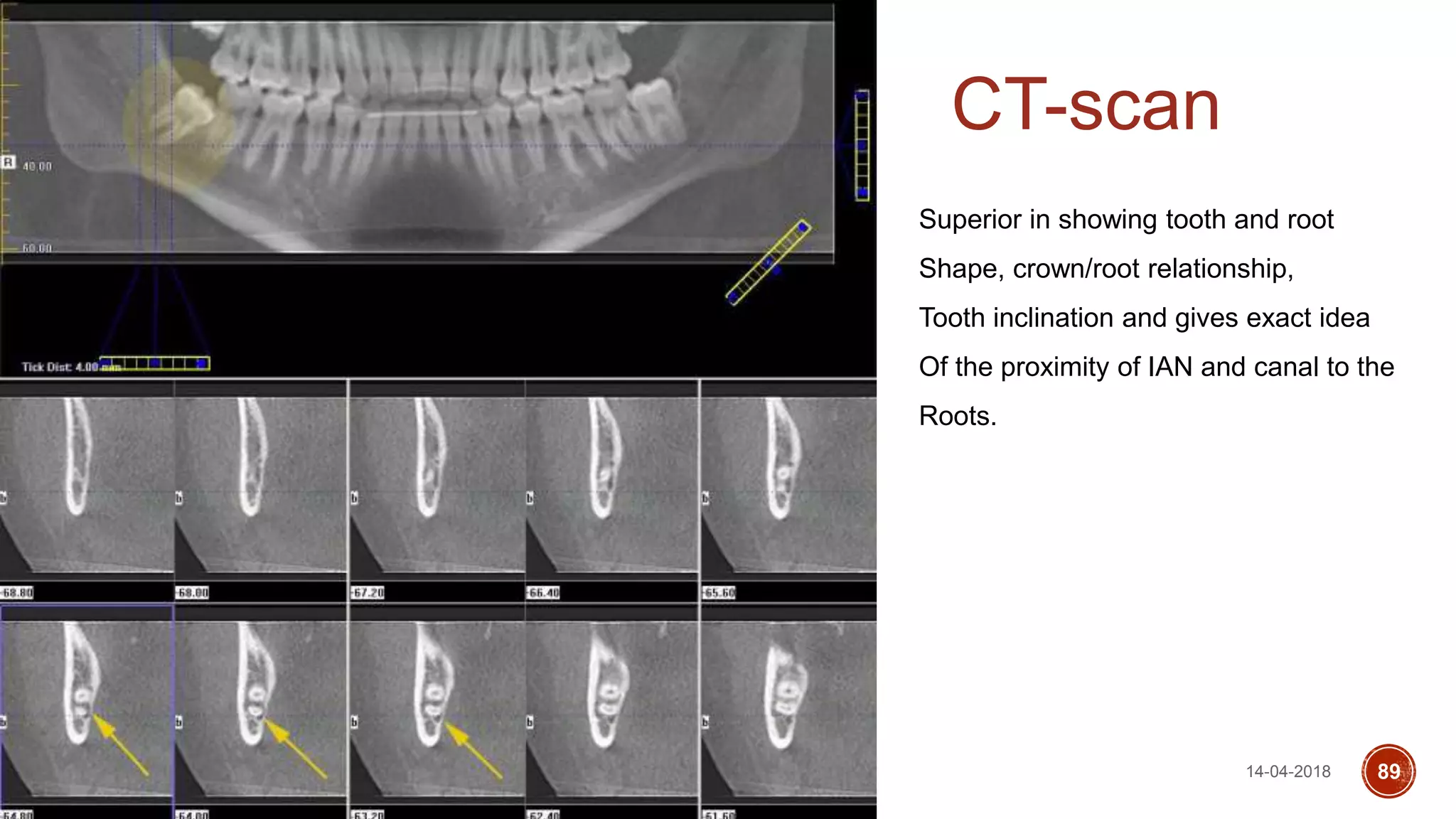
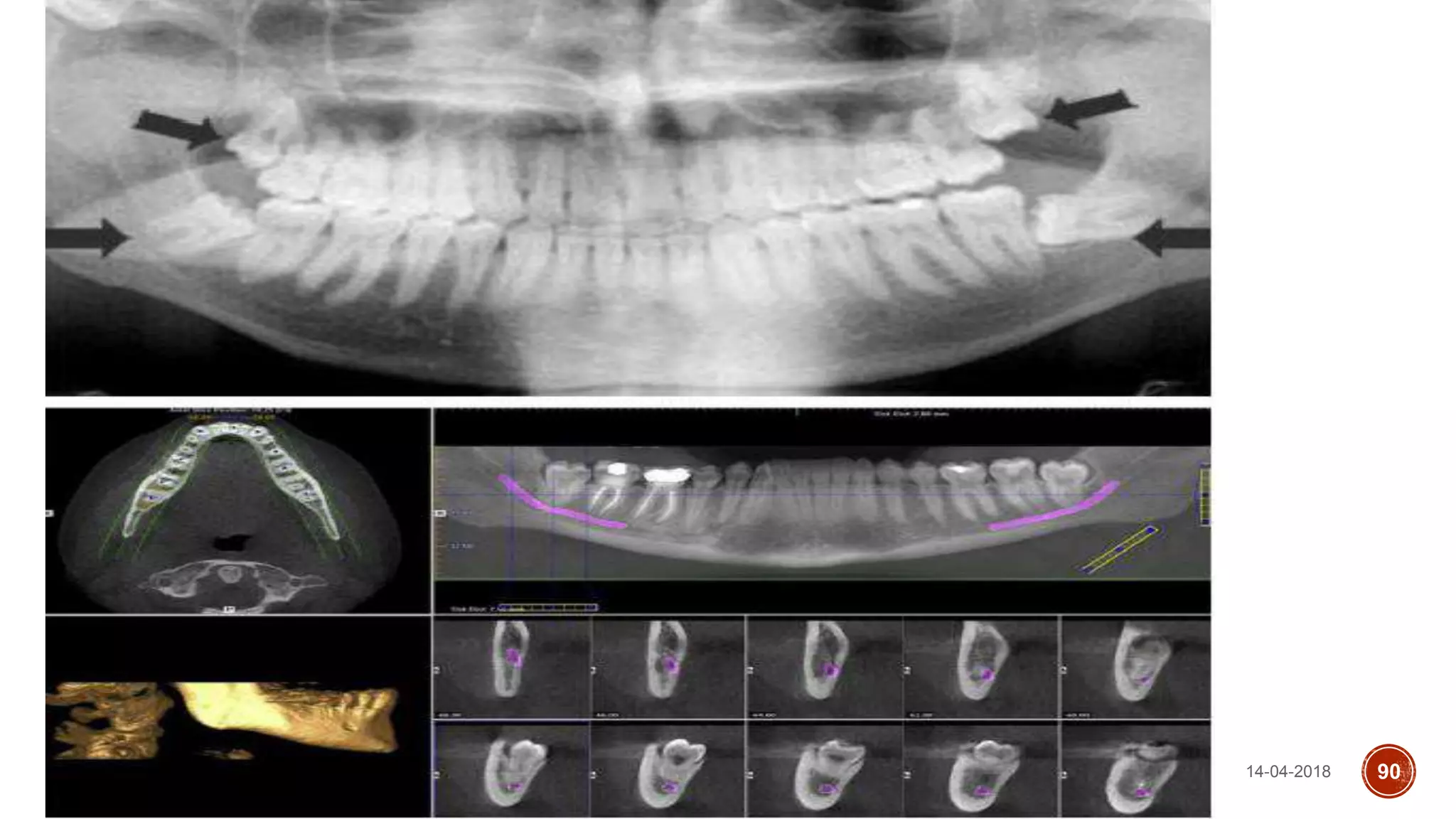
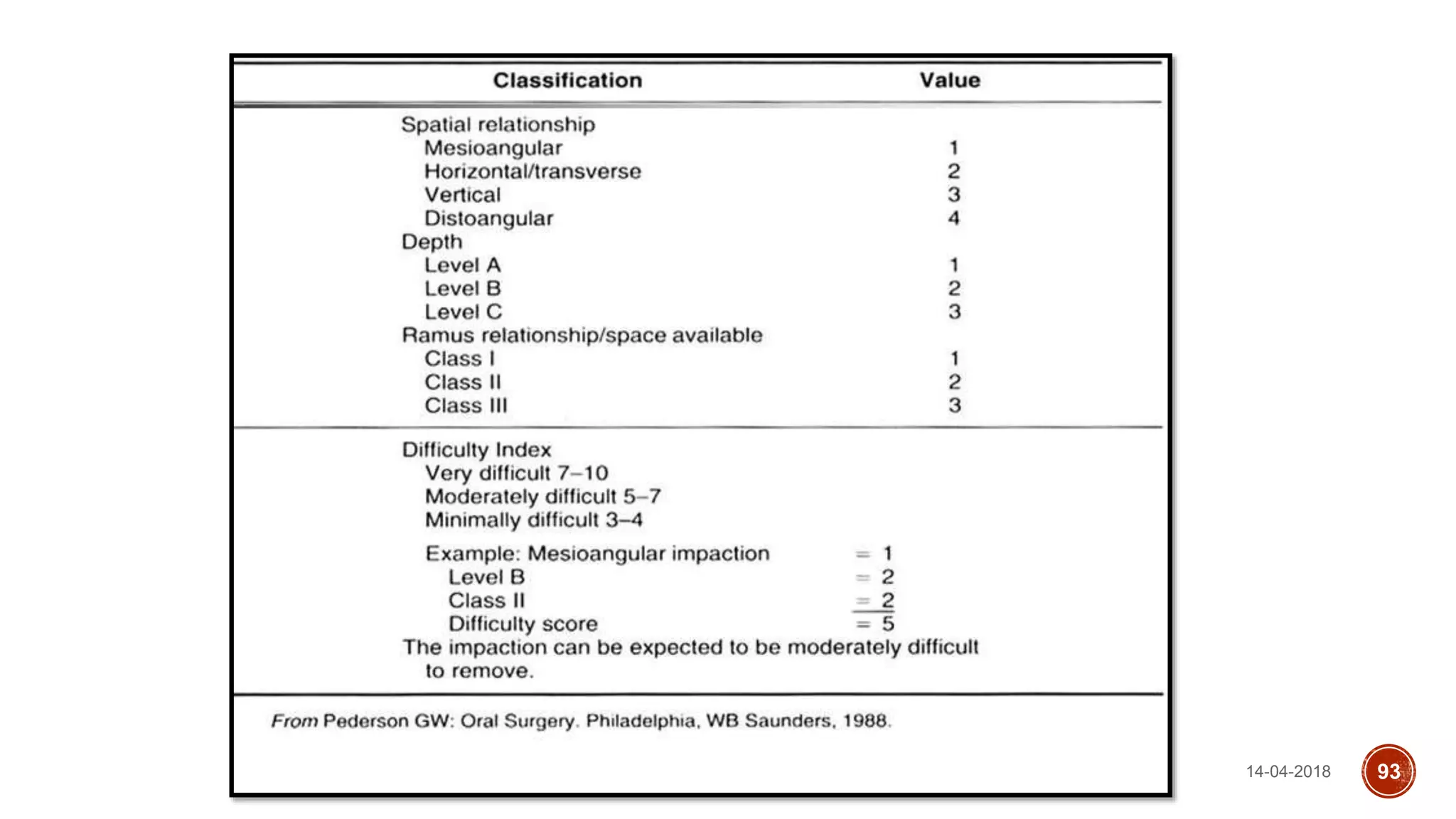
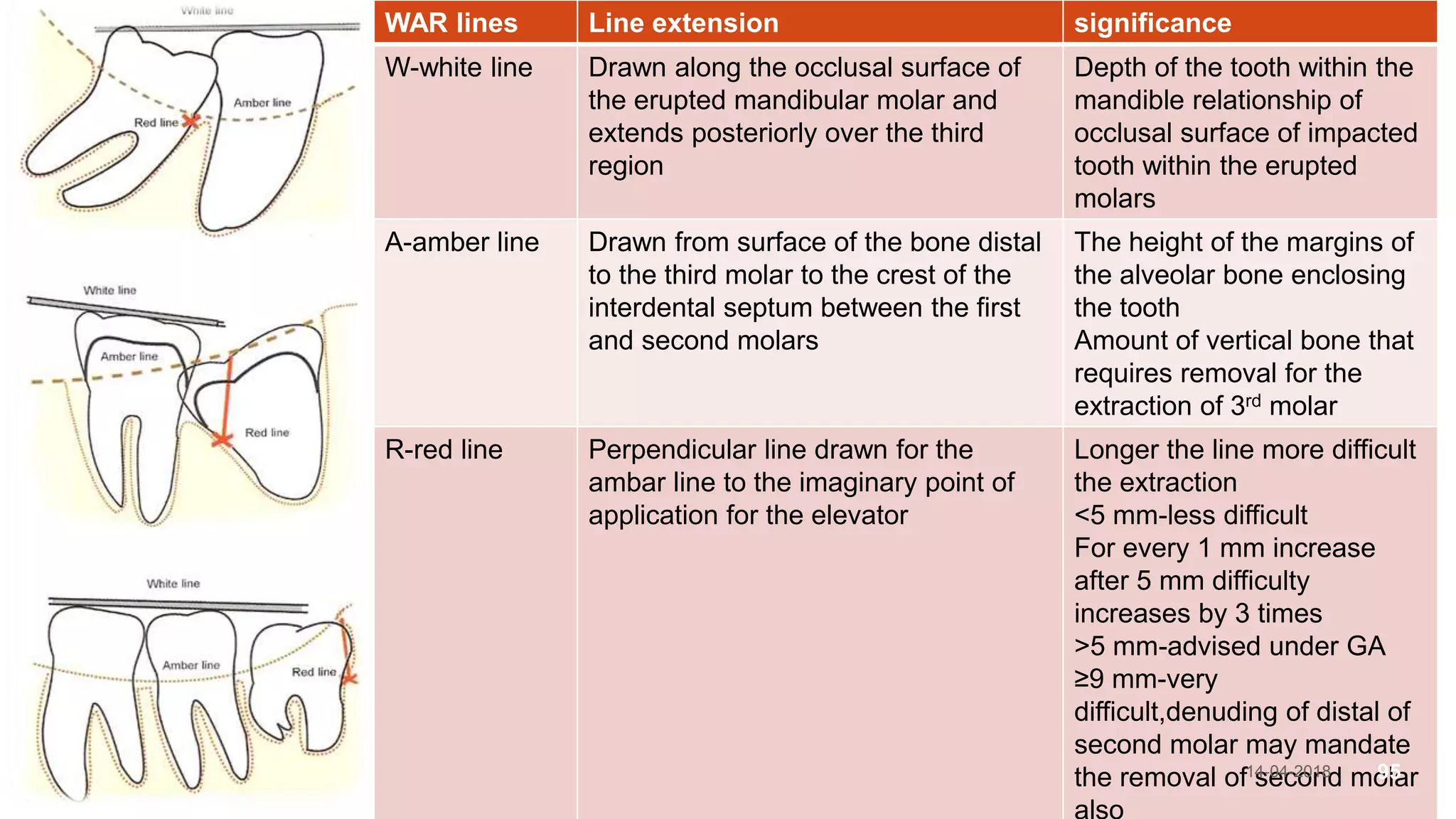
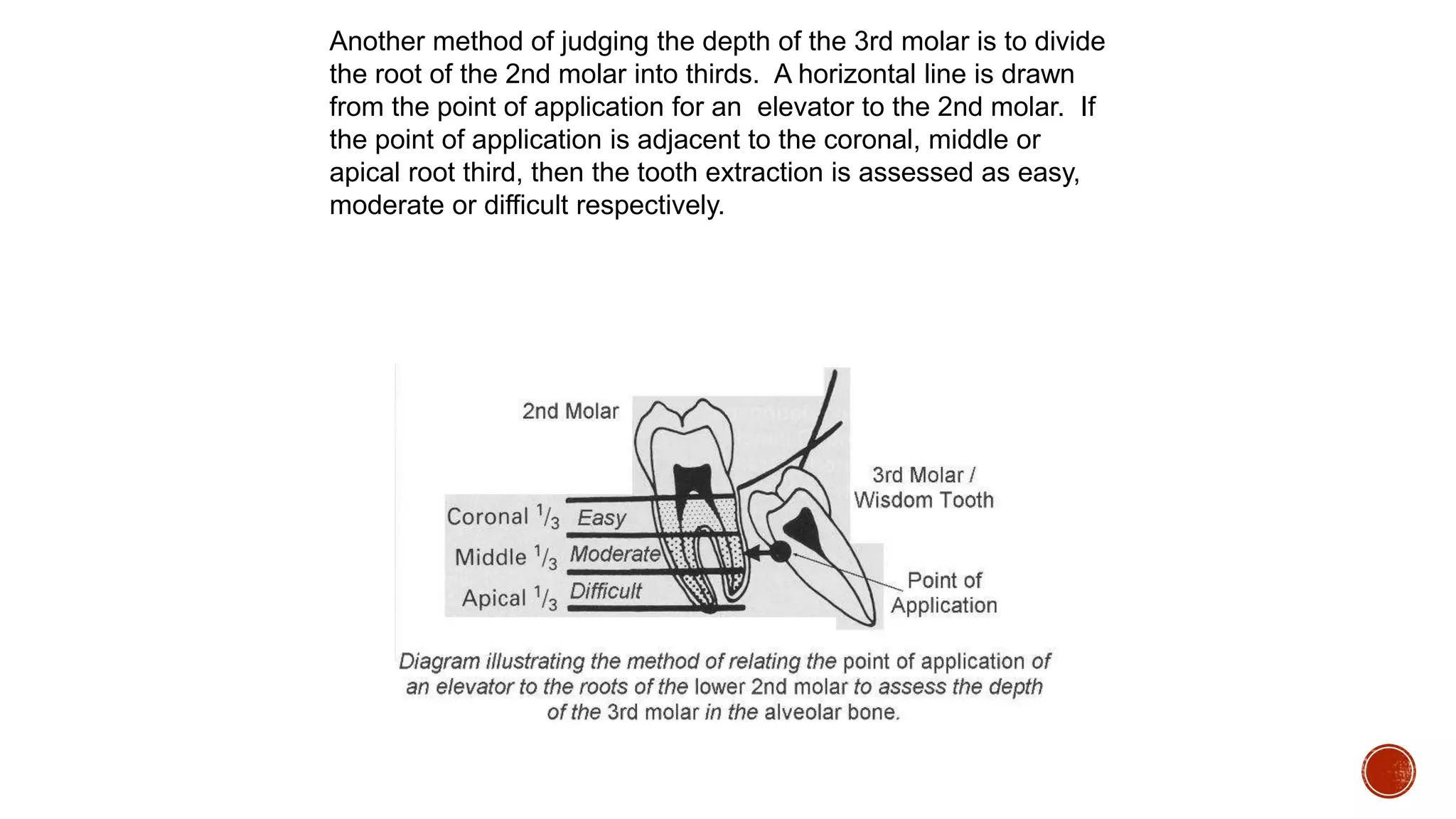
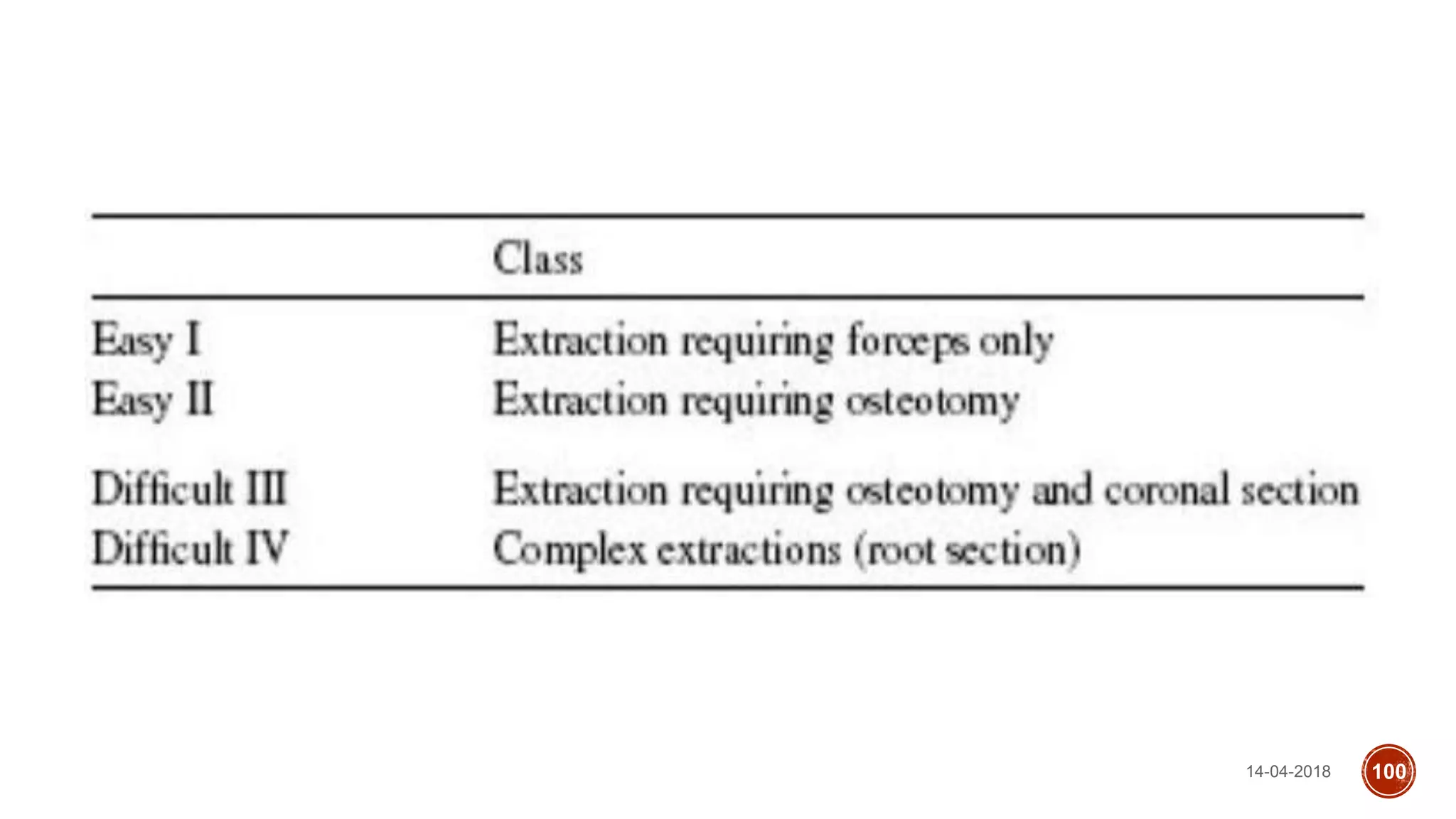
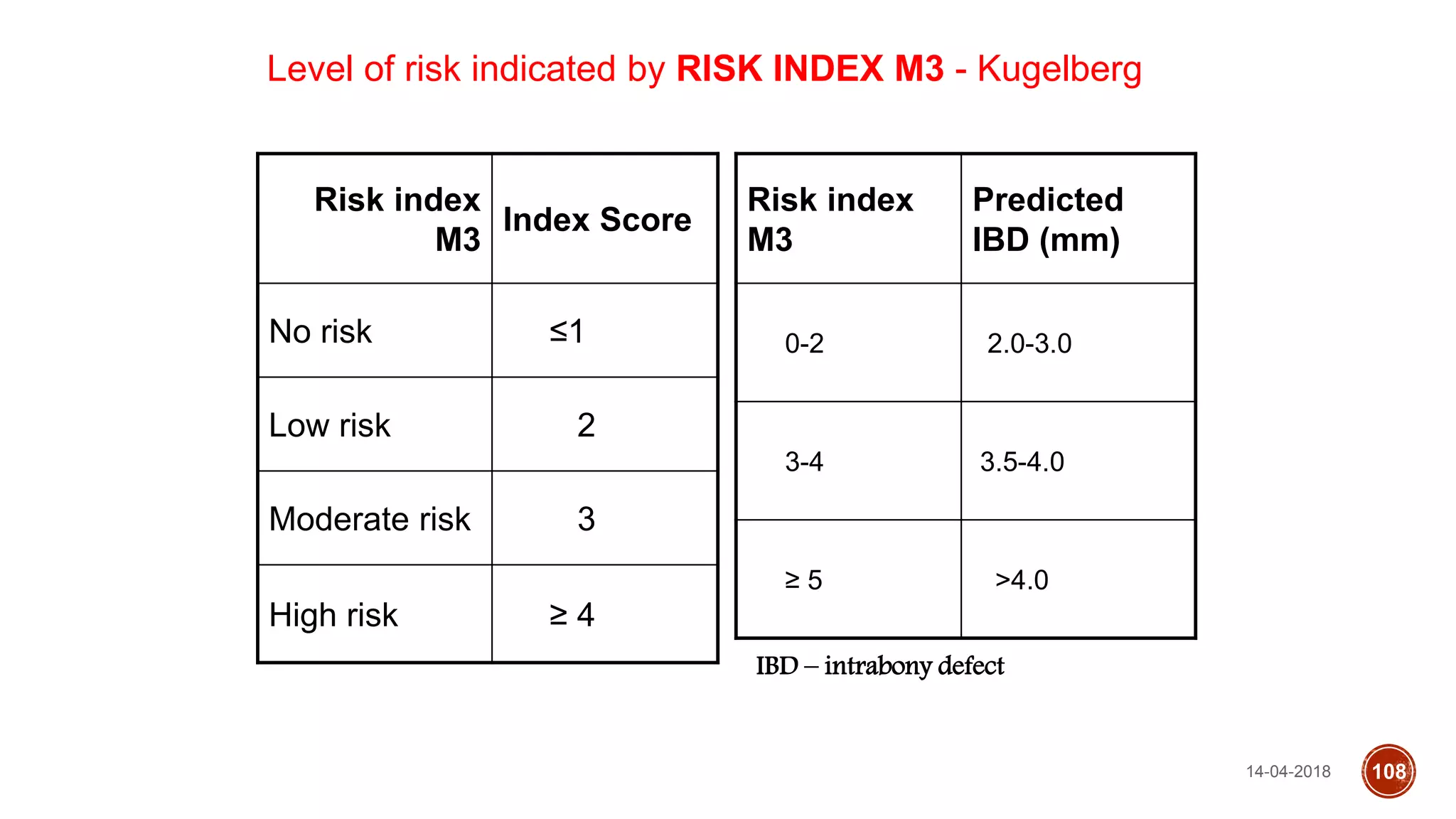
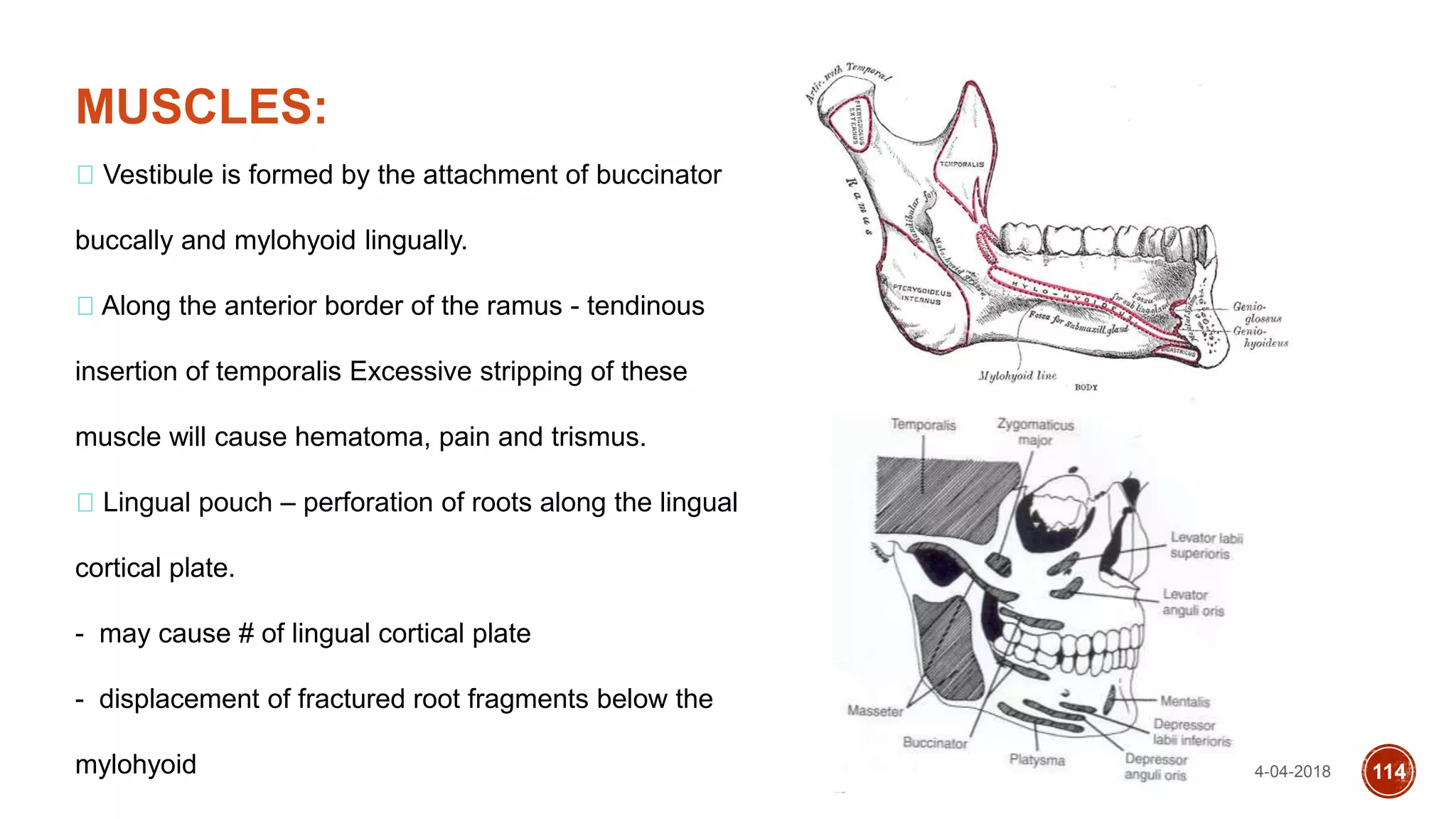
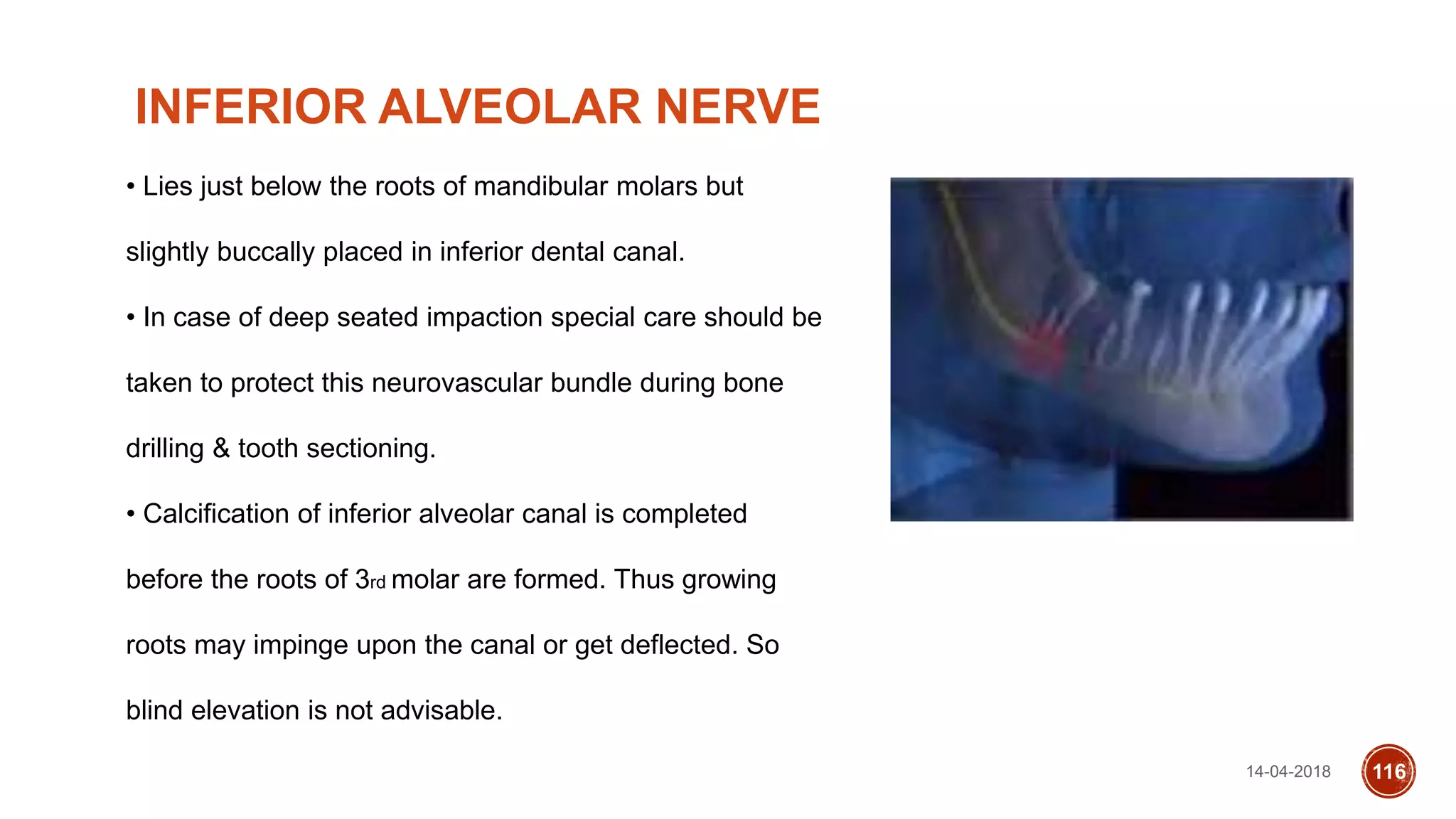
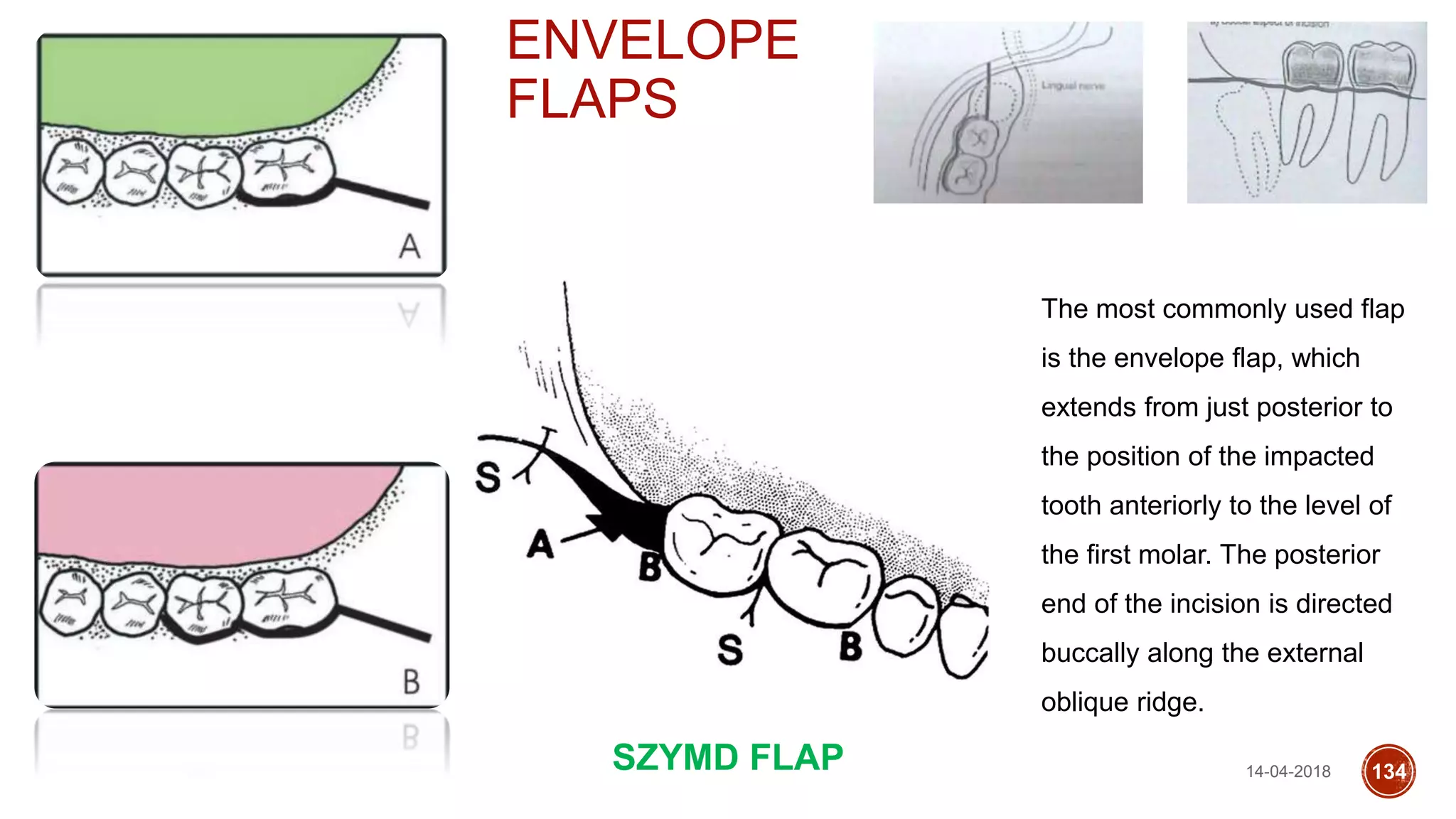
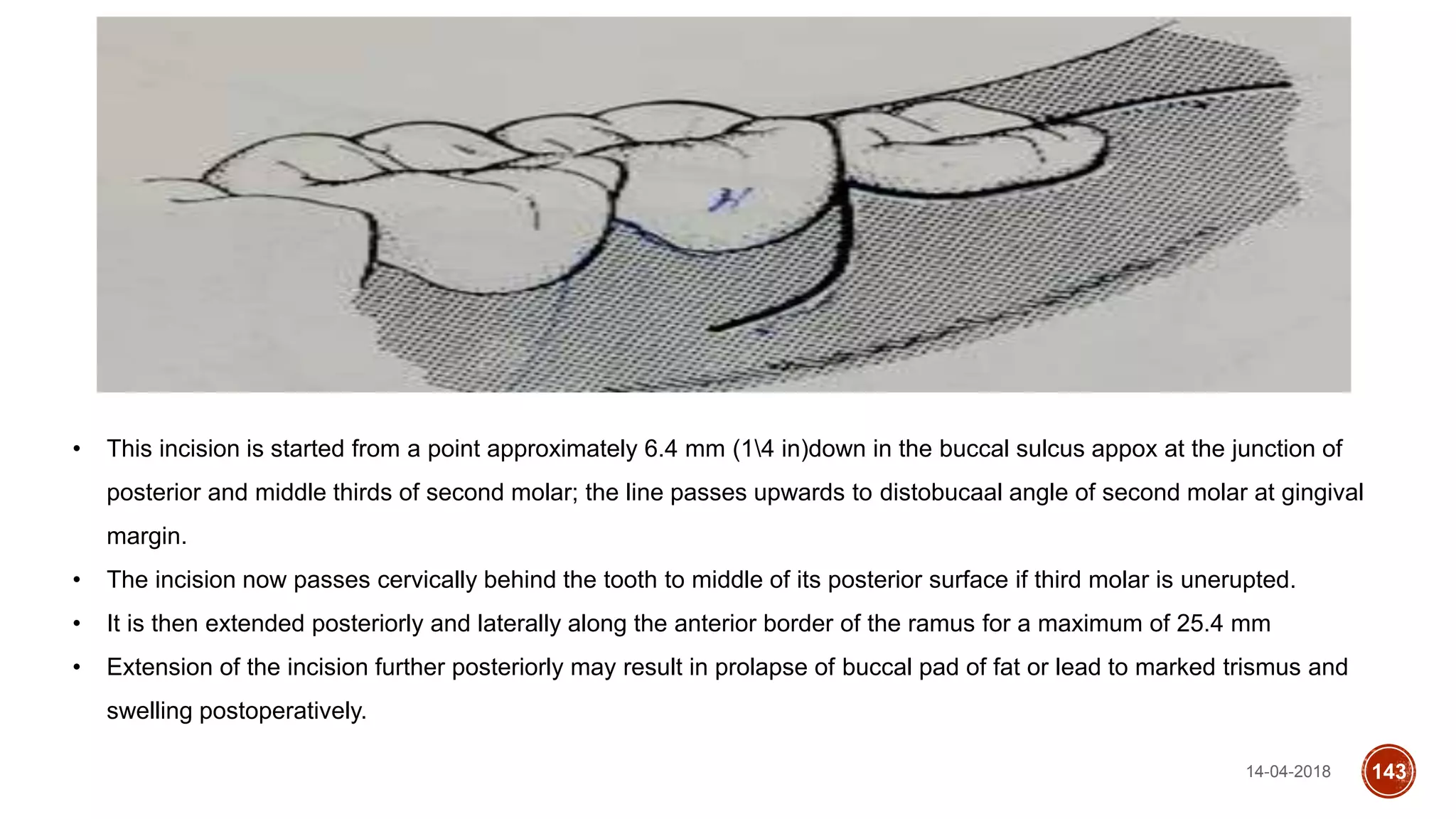
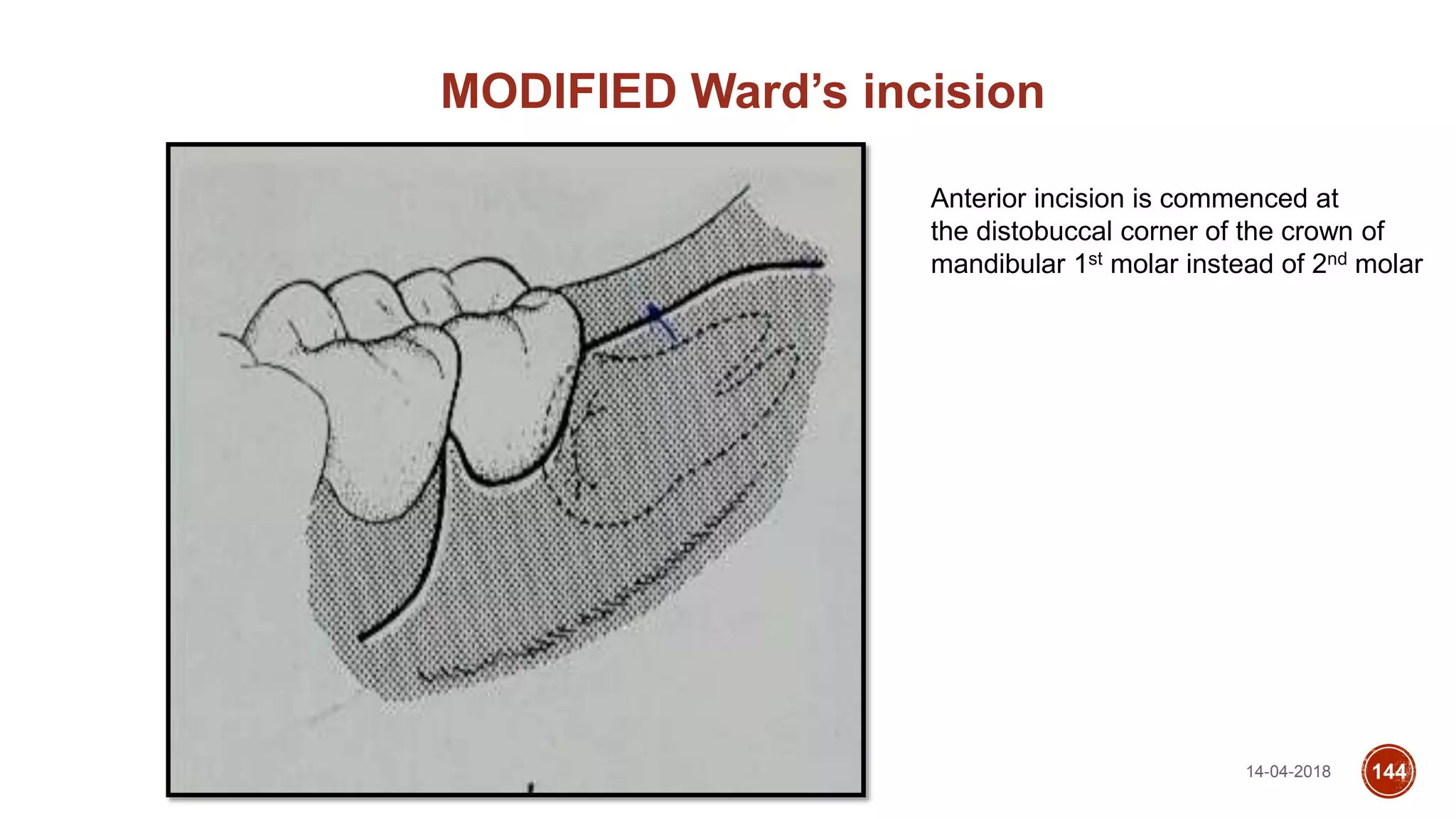
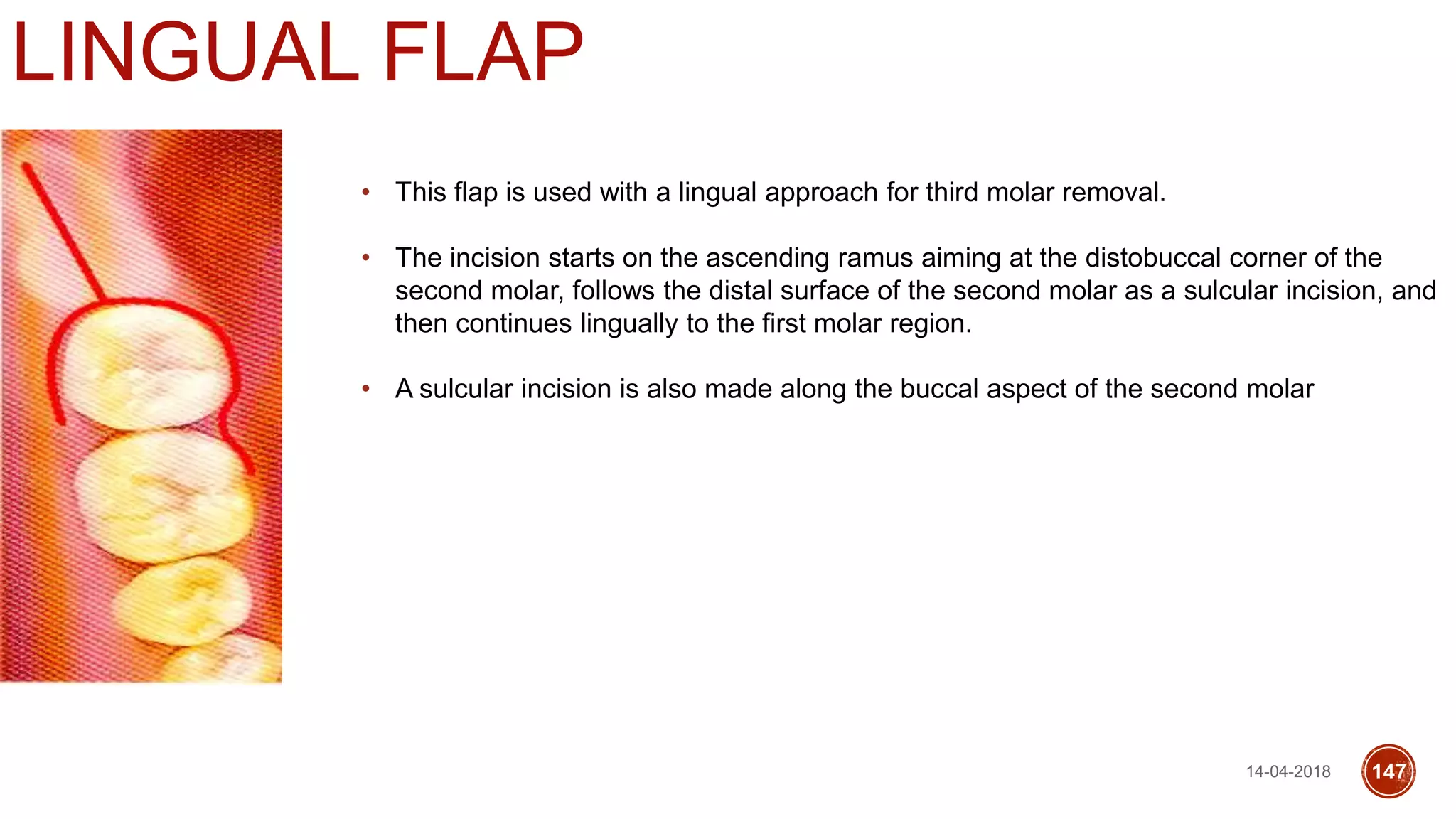
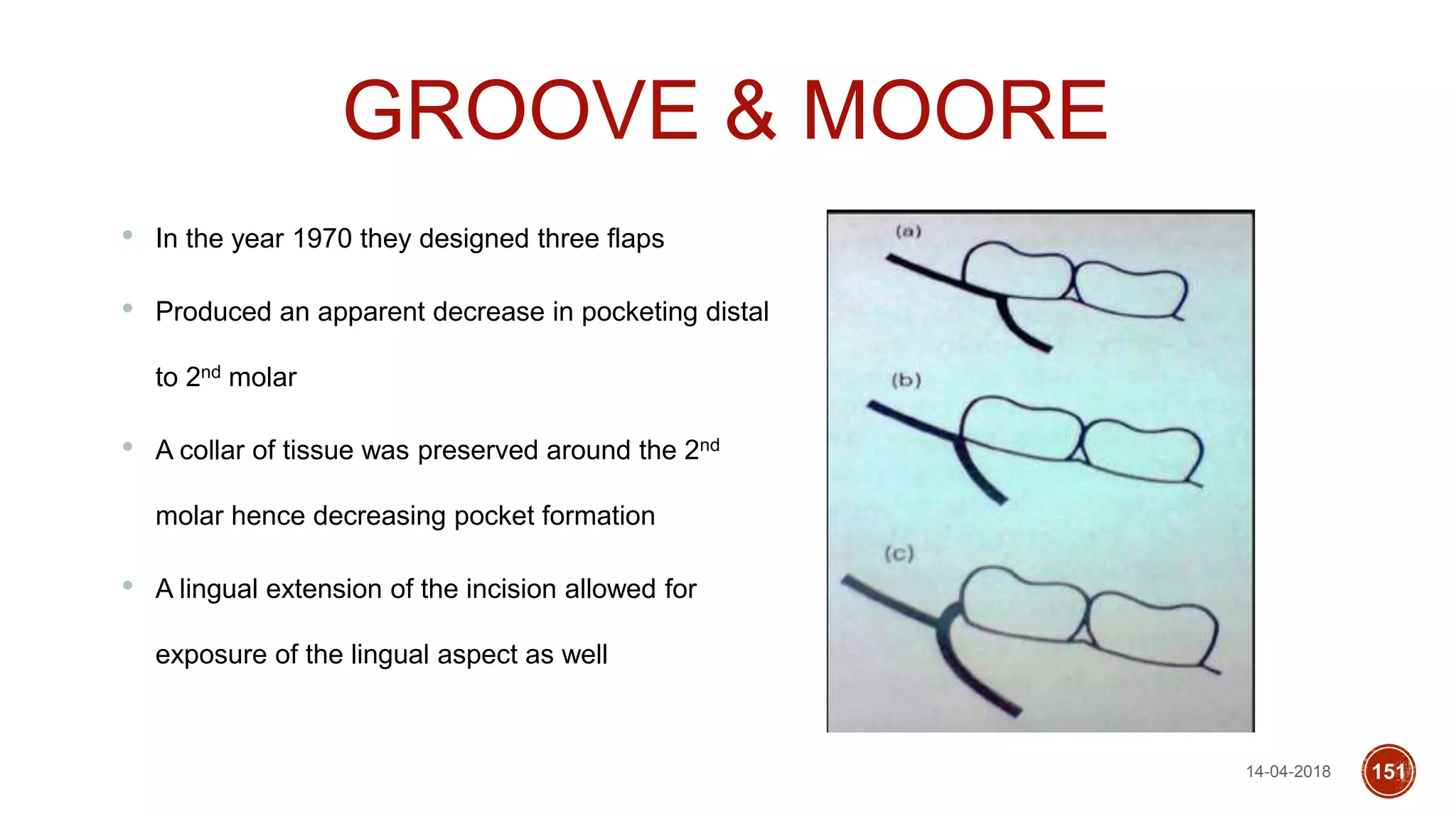
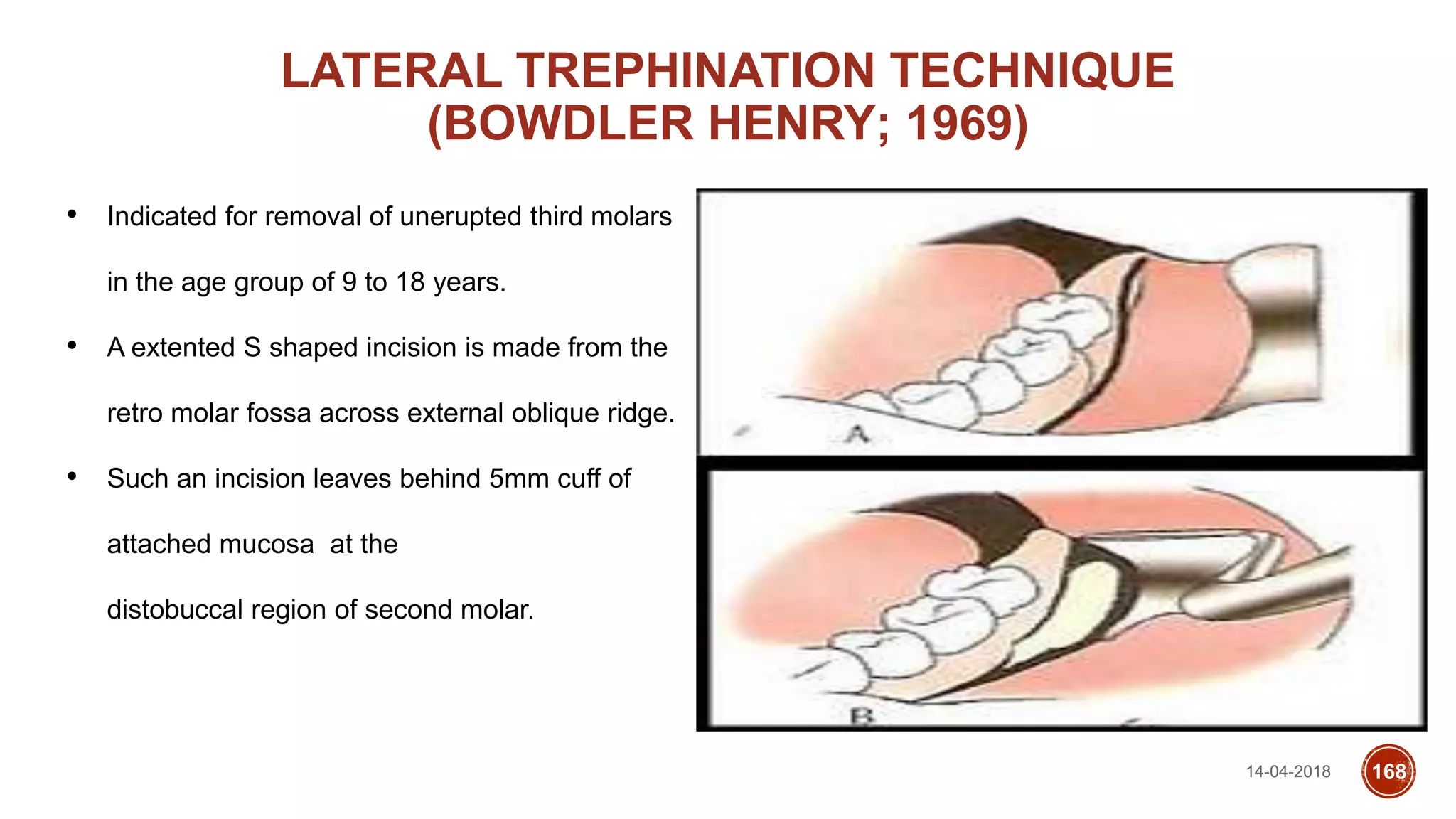
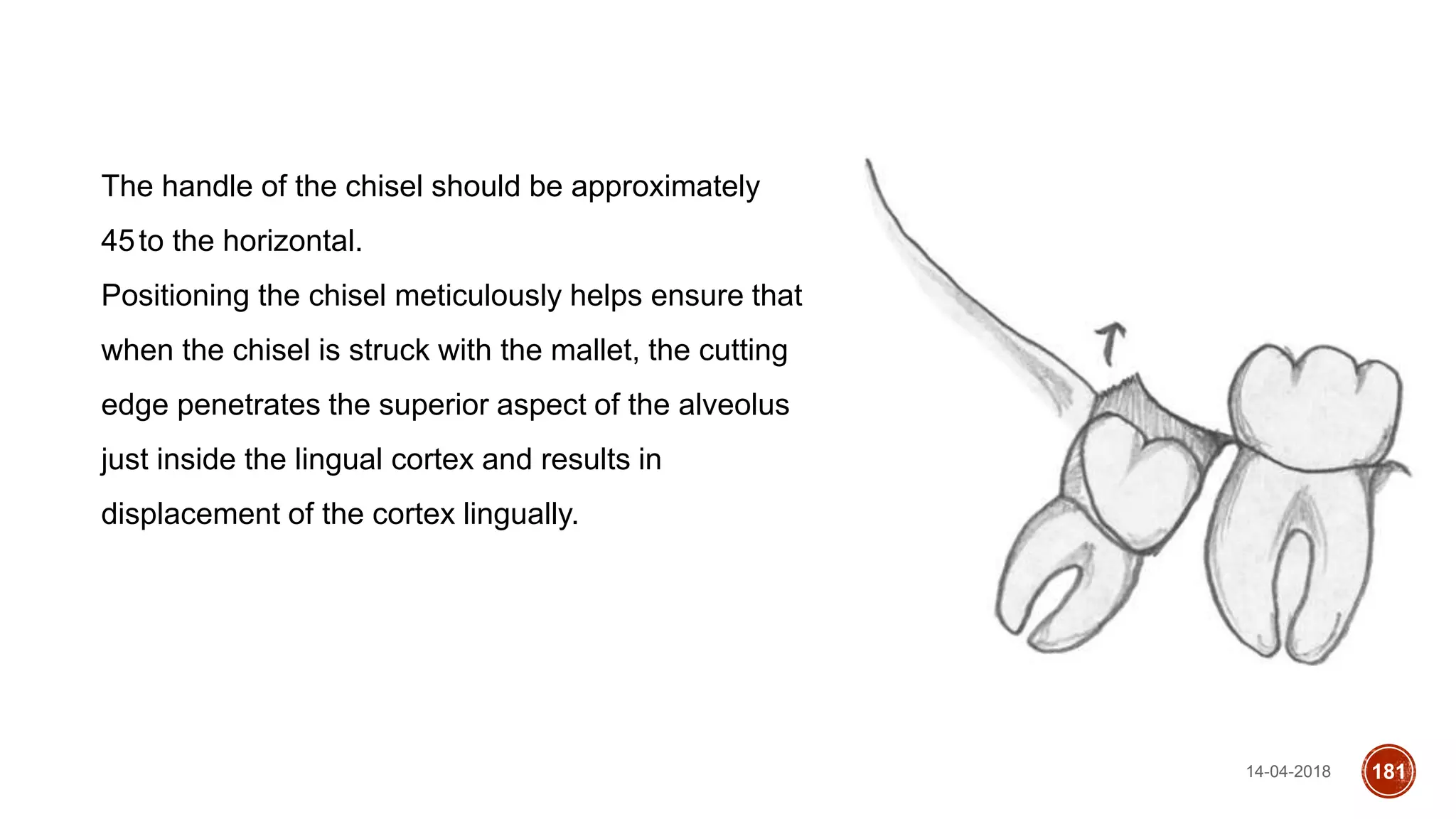
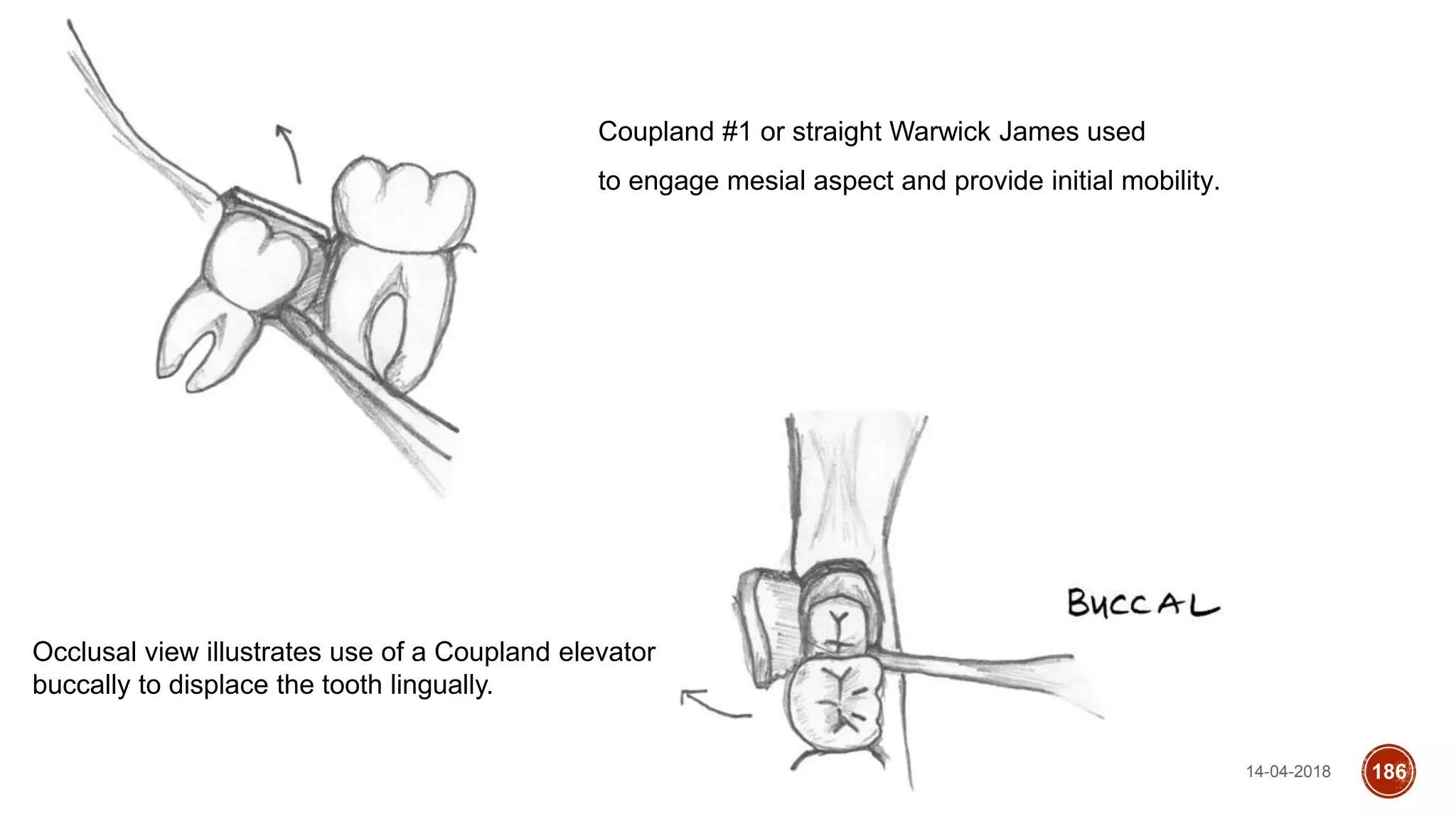
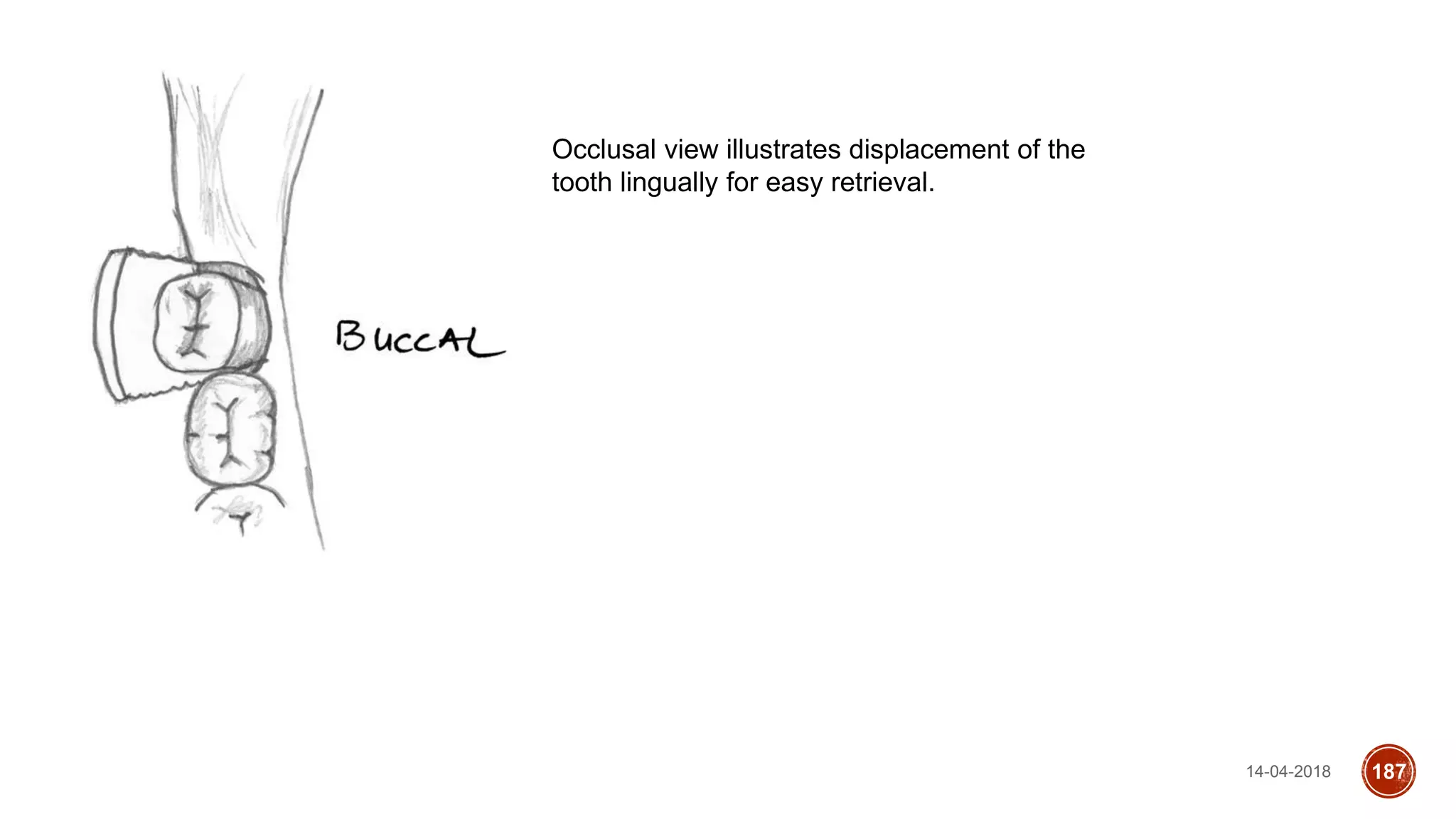
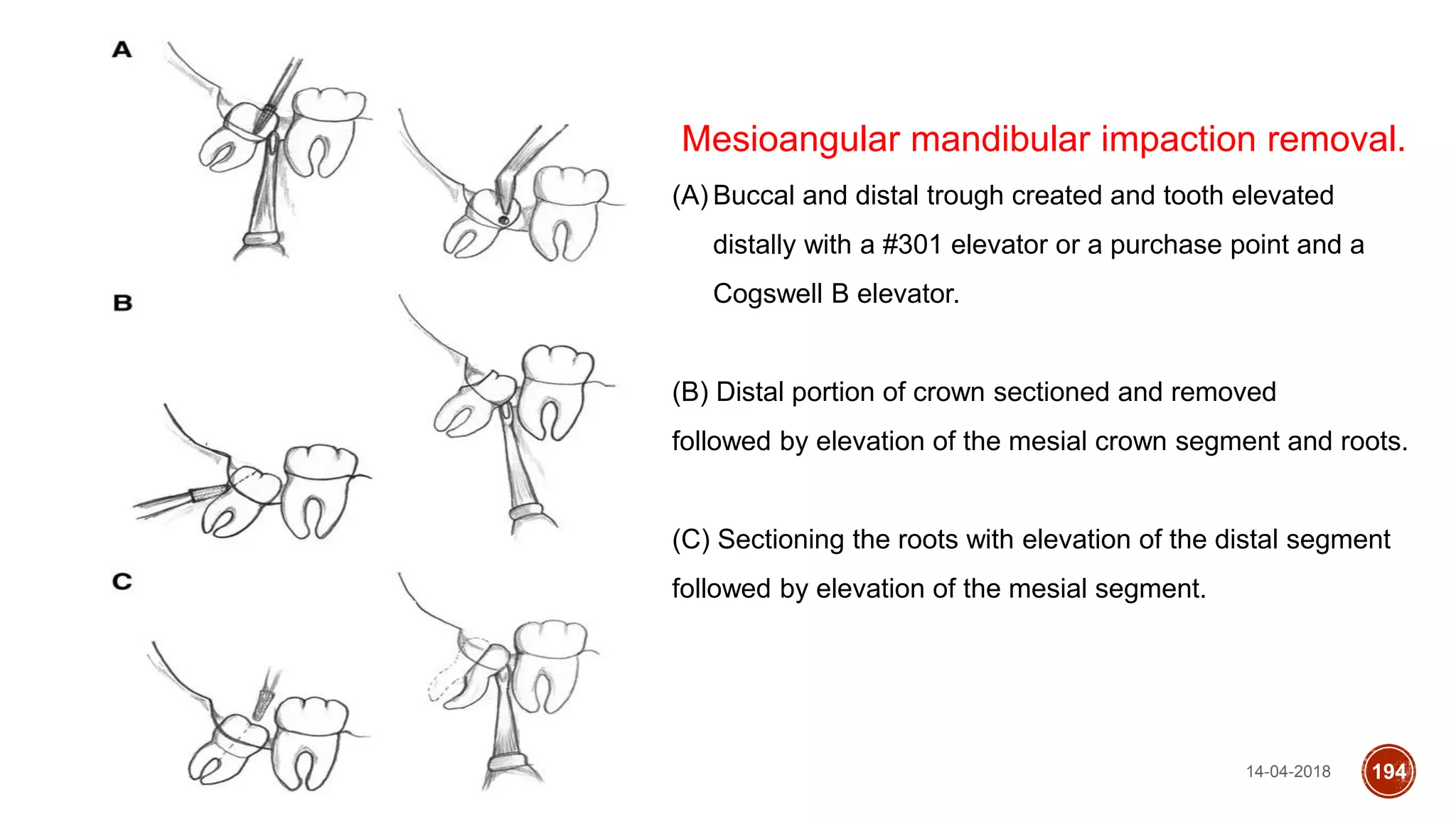
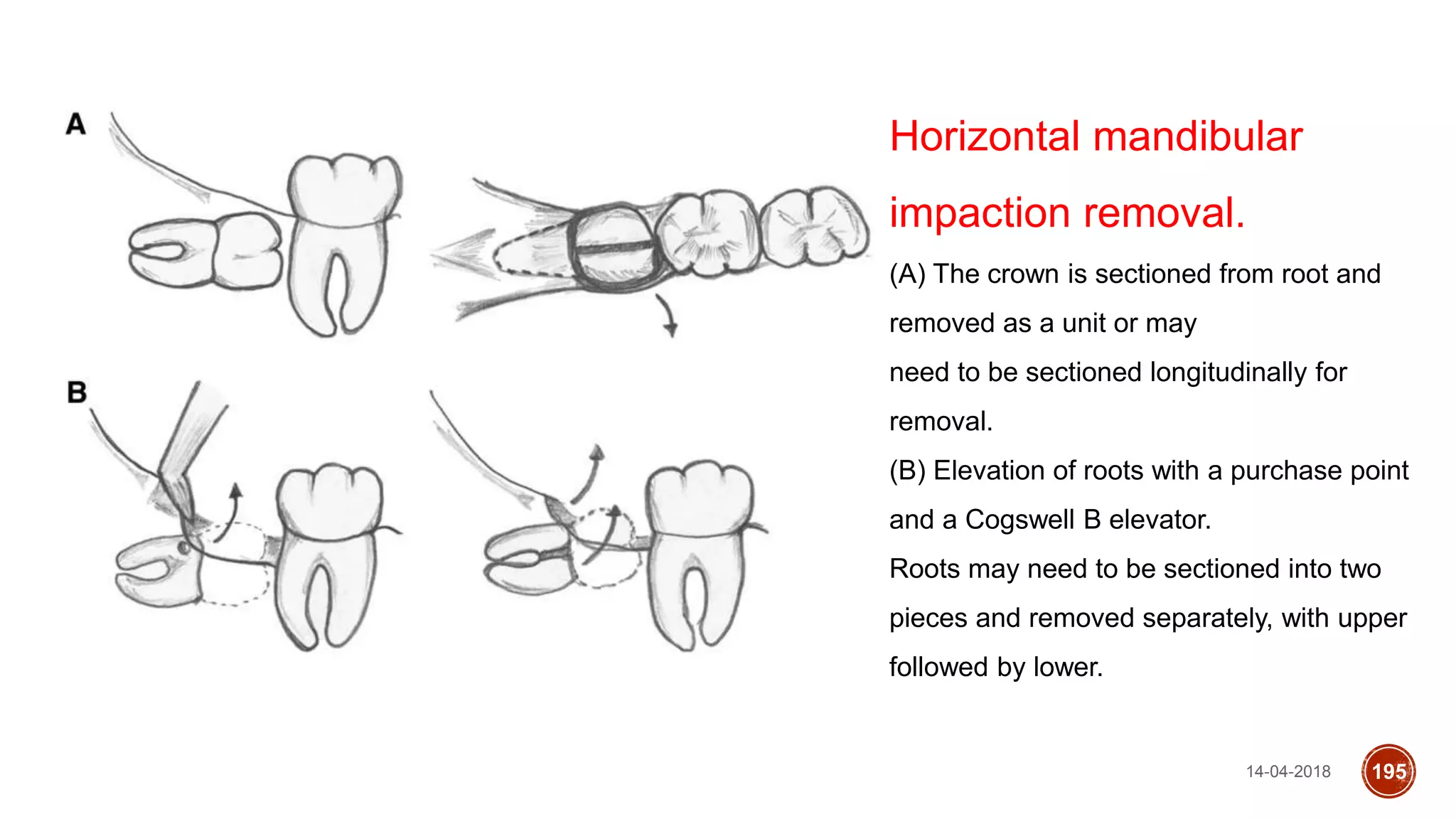
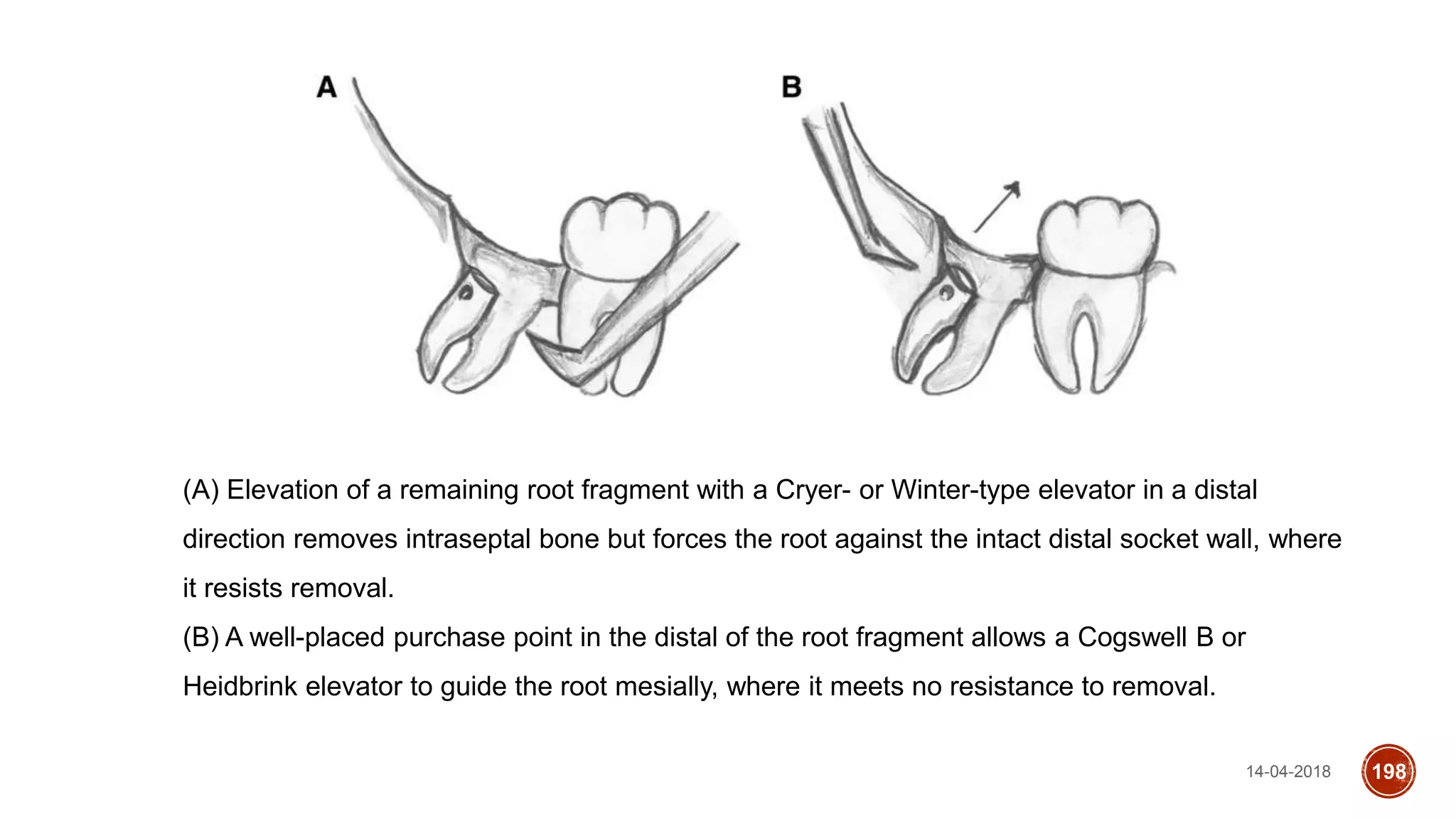
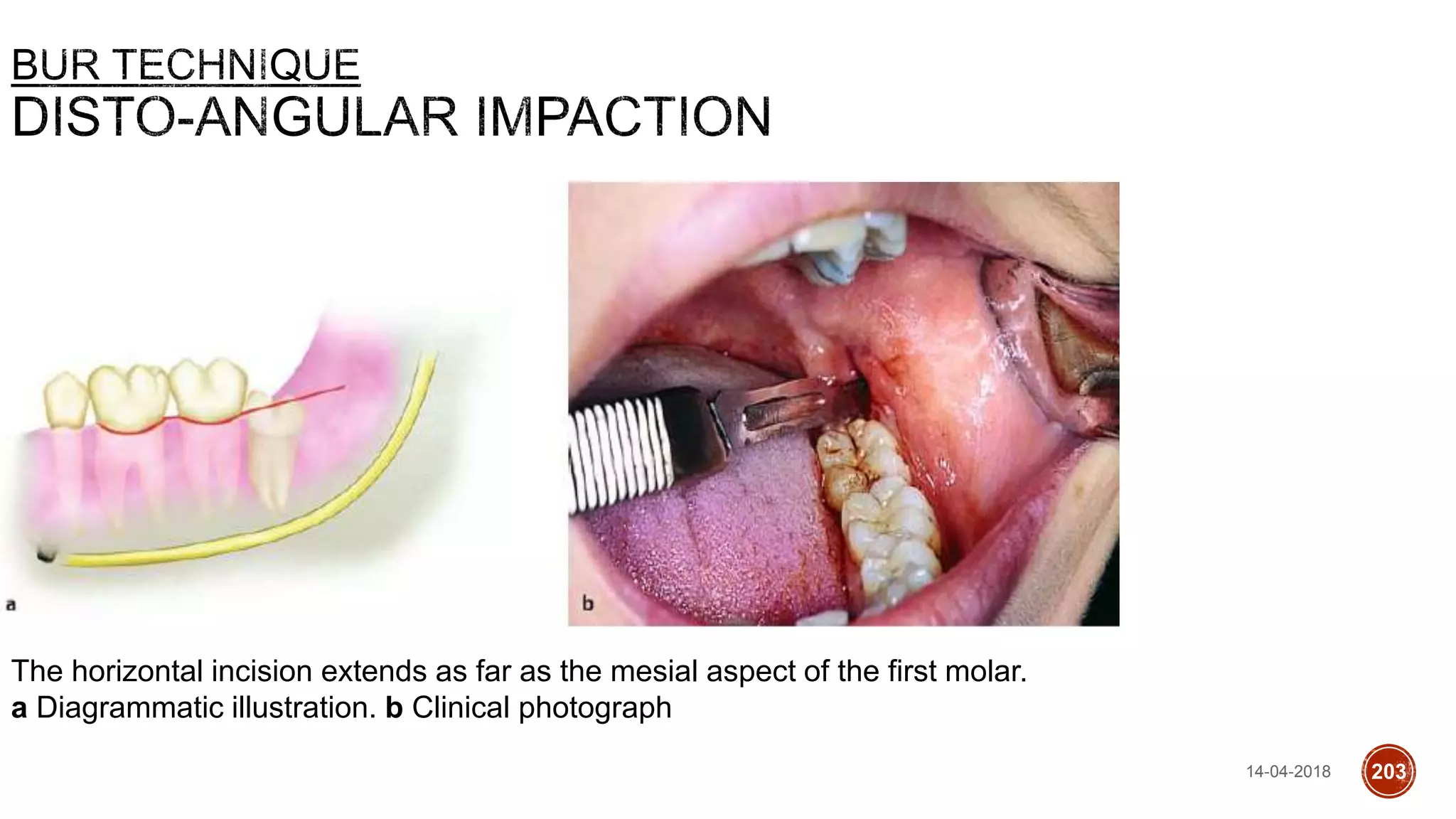
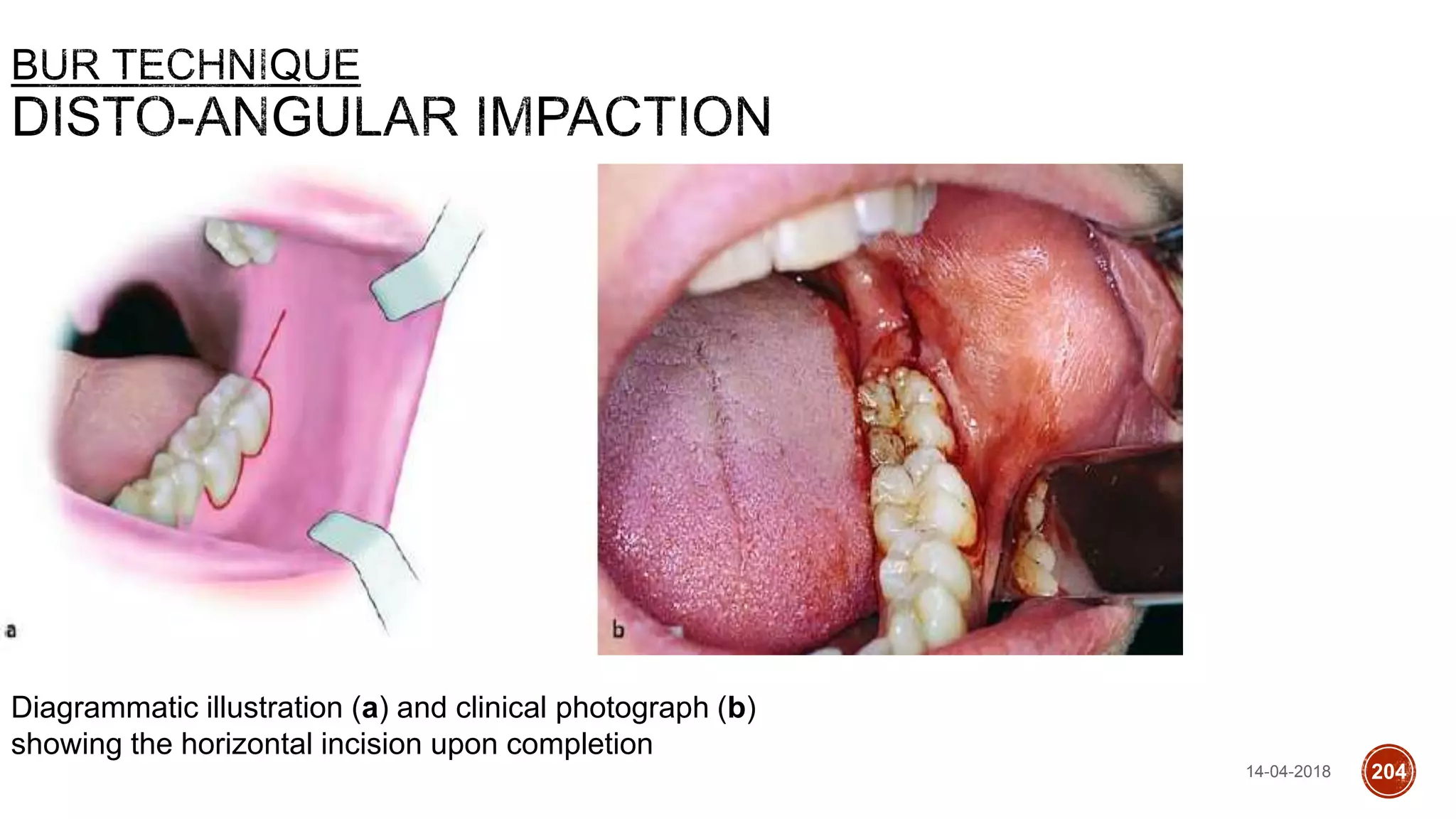
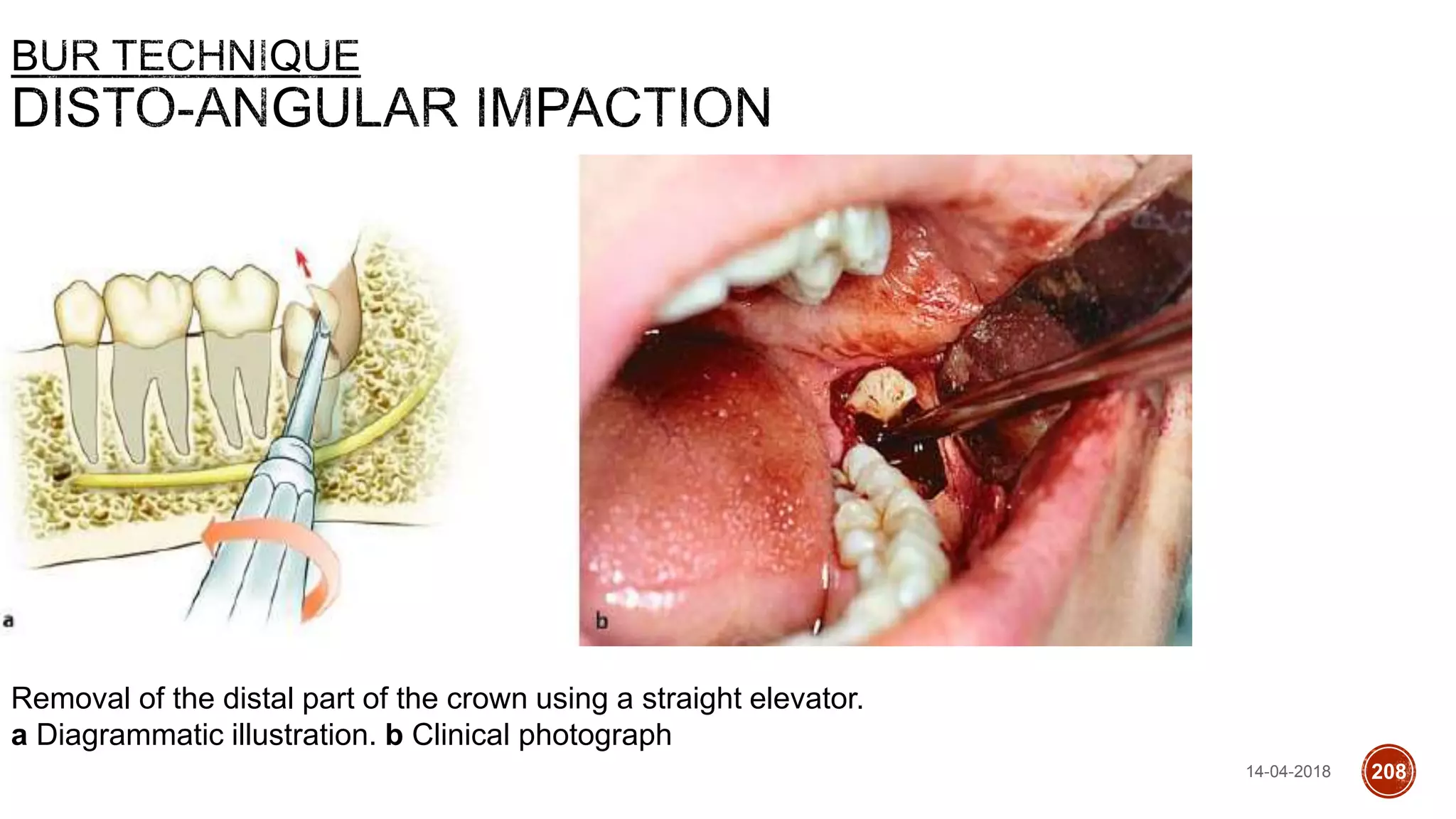
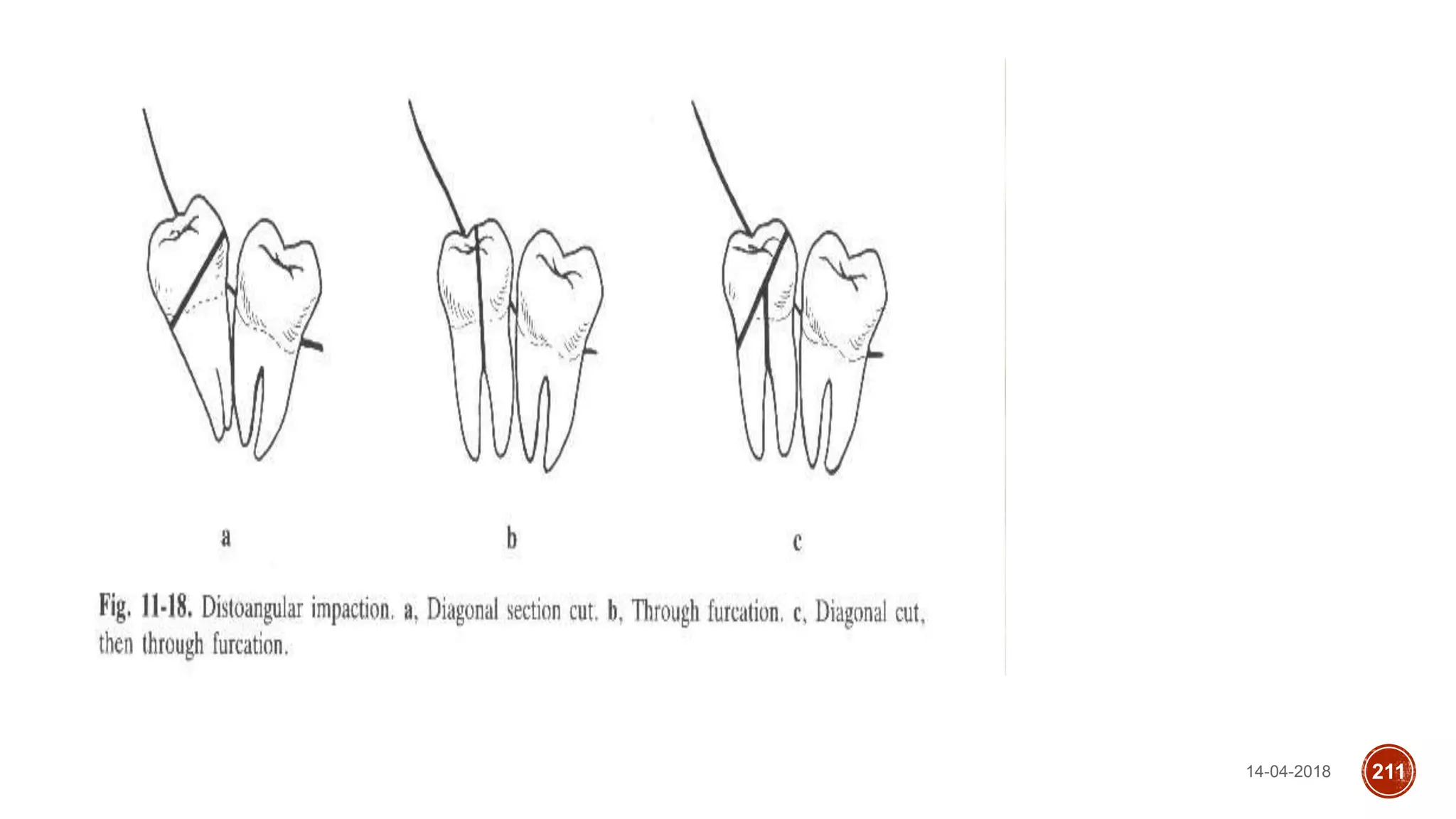
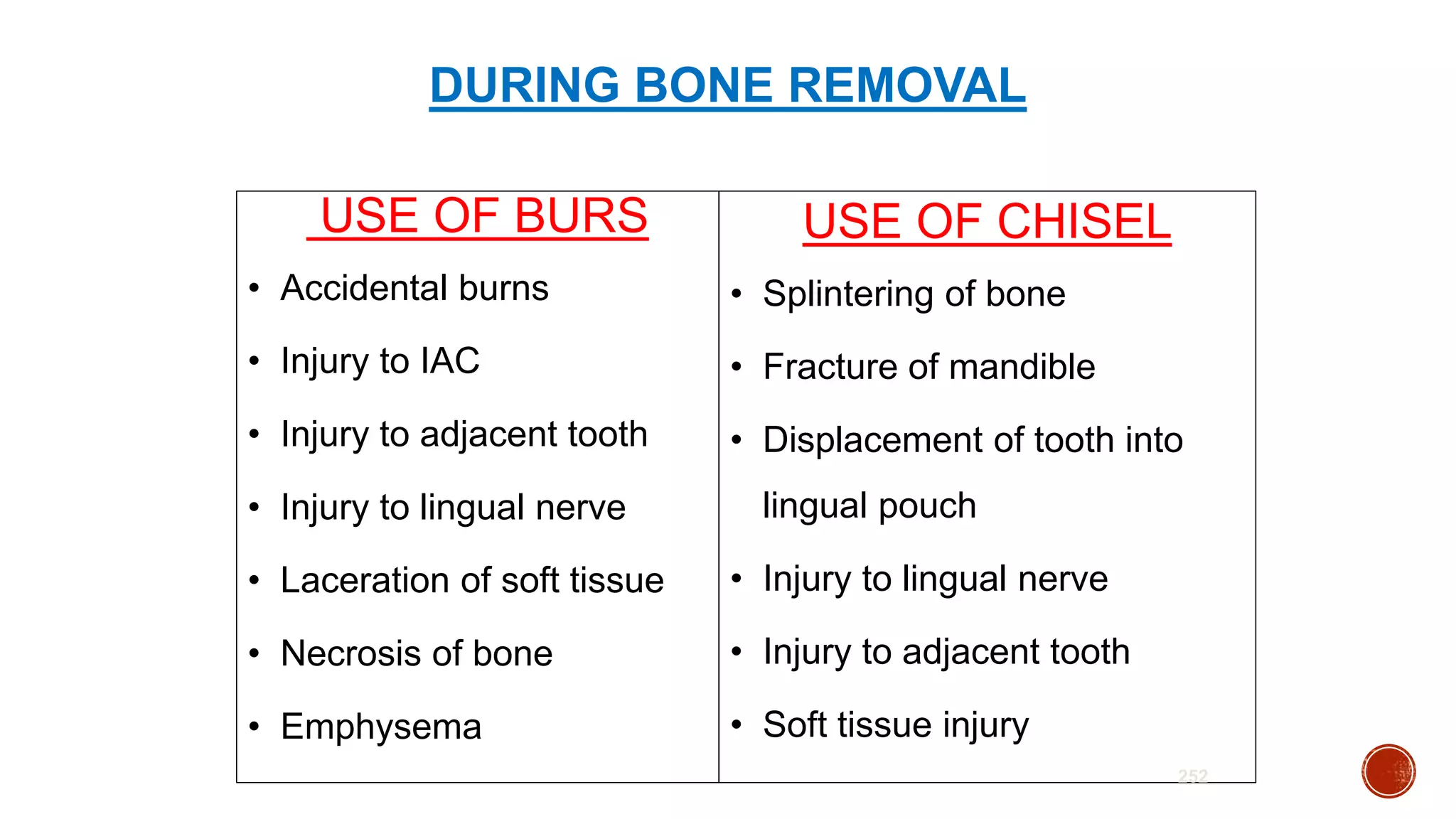
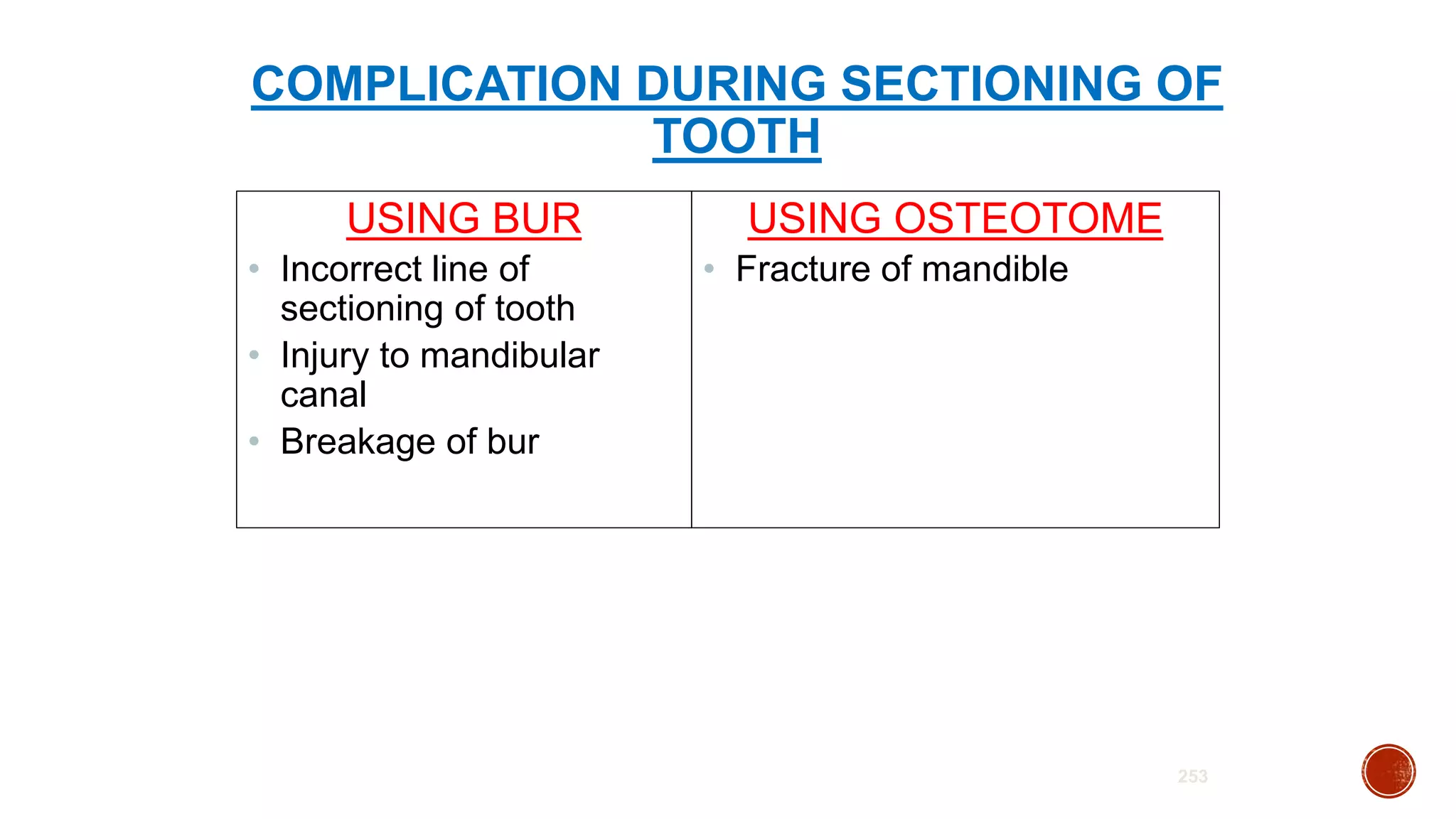
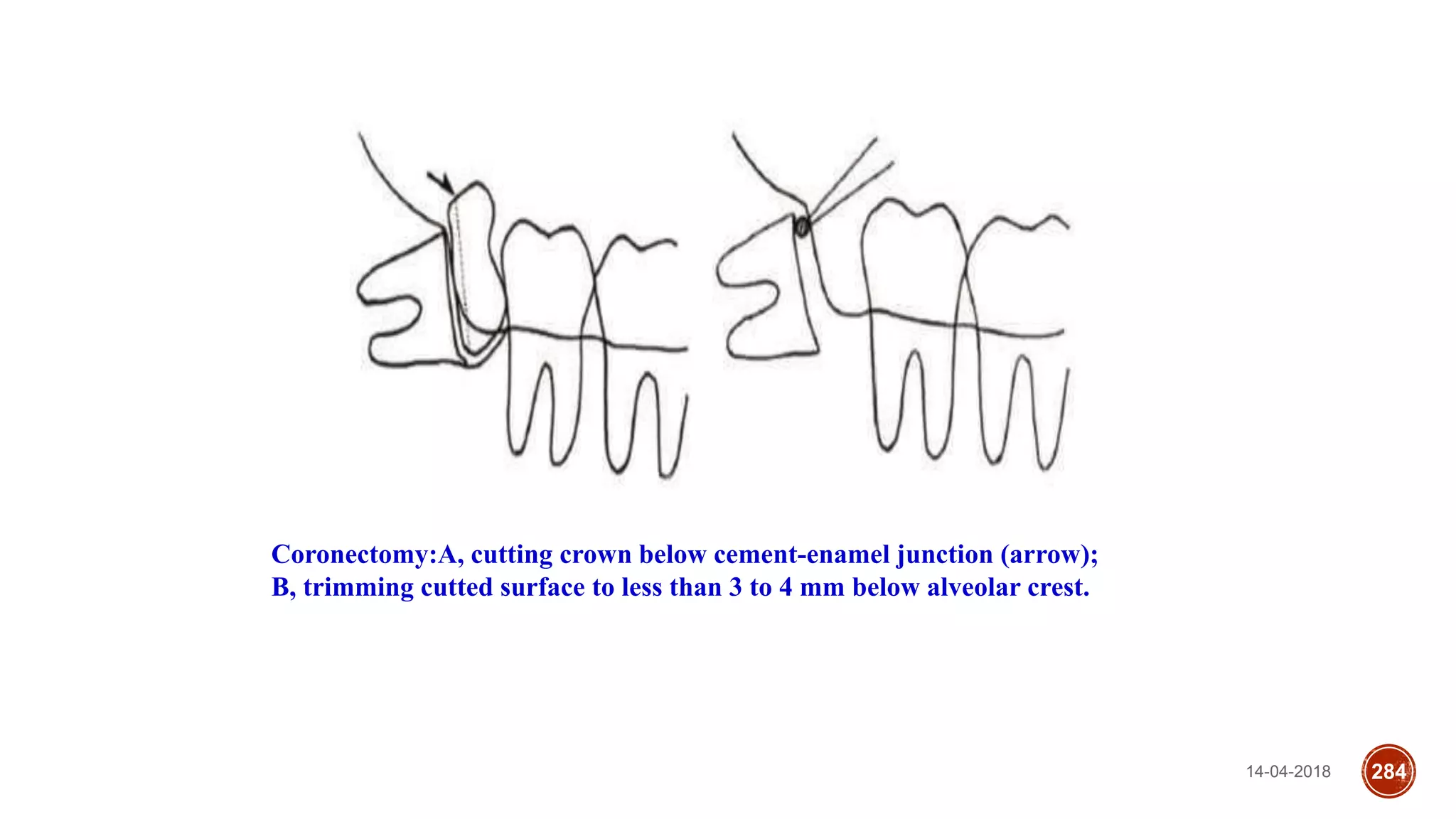
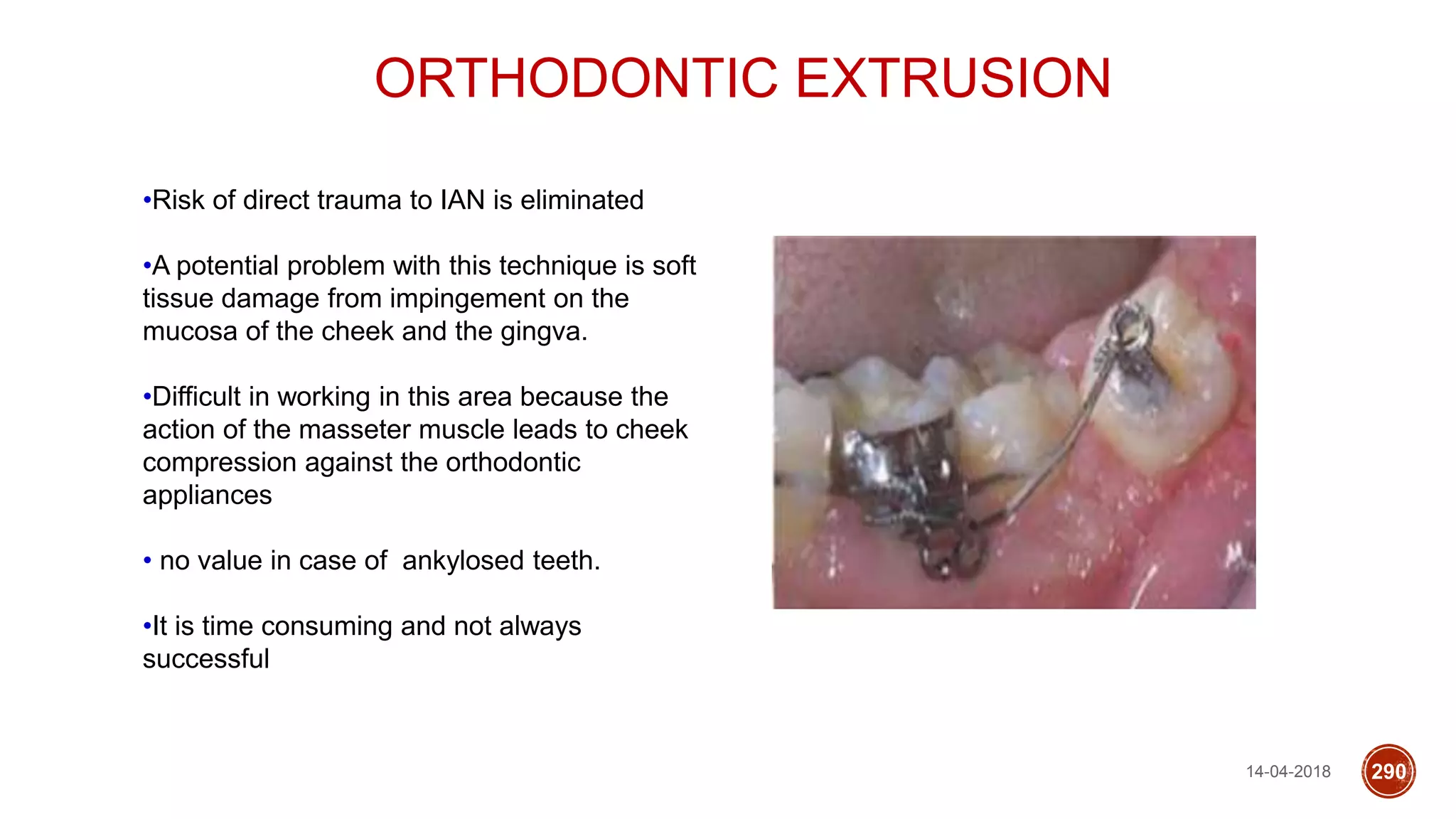
This document discusses impacted teeth, specifically focusing on impacted third molars. It begins with definitions of impacted teeth and provides the etymology and theories of tooth impaction. Local and systemic causes of impaction are described. Surgical anatomy of impacted third molars is reviewed, along with classifications of impacted mandibular third molars. Indications and contraindications for removal are outlined. Complications are briefly mentioned. The document is intended as a reference for oral and maxillofacial surgeons regarding the management of impacted third molars.