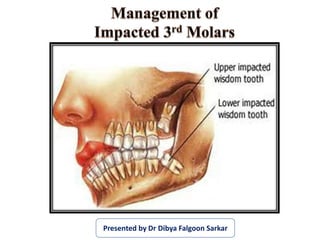
Management of Impacted Third Molars
- 1. Presented by Dr Dibya Falgoon Sarkar
- 2. Contents of Part I •Introduction •Terminology and definitions •Why teeth get impacted? •Indications and contraindications •Development of mandibular third molar •Classifications of impacted mandibular third molar teeth •Radiography and investigations •Surgical anatomy
- 3. Contents of Part II •Instrument tray setup •Operative procedure of Impacted Lower Third Molar •Surgical Removal of Impacted Maxillary Third Molar •Postoperative Care and Instructions •Drug Therapy •Complications of Impaction Surgery •Ectopic Teeth and Unusual Cases •Recent Advances and the Future of Third Molars
- 4. • Evaluation and management of impacted teeth are among the most frequent services offered by oral & maxillofacial surgeons • Reddy et al (JOMS 2012) showed that the overall prevalence of third molar impactions is about 18.6% among Indian population • Berge T.I and Gilhuus-Moe O.T (1993) showed that there is a four fold increase in the incidence of complications of impaction cases when the surgery was performed by a general practitioner as compared to that performed by an oral surgeon. • This difference in complication rates may be attributed to inadequate surgical training and lack of experience of the former.
- 5. •The term impaction is derived from Latin word 'impactus’. •Impactus means, “An organ or structure which because of an abnormal mechanical condition has been prevented from assuming its normal position.”
- 6. Mead (1954 ) An impacted tooth is a tooth that is prevented from erupting into position because of malposition, lack of space, or other impediments. Archer (1975) A tooth which is completely or partially unerupted and is positioned against another tooth, bone or soft tissue so that its further eruption is unlikely, described according to its anatomic position.
- 7. Andreasen et al (1997) A cessation of the eruption of a tooth caused by a clinically or radiographically detectable physical barrier in the eruption path or by an ectopic position of the tooth. WHO (2007) An impacted tooth is any tooth that is prevented from reaching its normal position in the mouth by tissue, bone or another tooth.
- 8. • The third molars or the wisdom teeth normally erupt last, between 18 and 25 years of age. • John hunter (1771) is one of the early authors who noted “want of room in the jaws for these late teeth” and he also suggested as a cause that “the jaws had left off growing”.
- 9. A number of theories has been put forward to explain the cause of impaction. The most commonly accepted ones are the following: •Phylogenic theory (Nodine 1943) •Mendelian theory •Orthodontic theory(Durbeck 1881) •Endocrinal theory •Anthropological theory (Mac Gregor 1985)
- 10. 1) Phylogenic theory (Nodine):- This theory motivated from Lamarck’s disuse theory. According to his theory if the particular body part is not used it will disappeared. Due to changing nutritional habits of our civilization, use of large powerful jaws have been practically eliminated. Thus, over centuries the mandible and maxilla decreased in size leaving insufficient room for third molars.
- 11. Small Jaws And Large Teeth Small Jaws And Small Teeth Large Jaws And Large Teeth Large Jaws And Small Teeth Small Jaws And Small Teeth Large Jaws And Large Teeth 2) Mendelian theory :
- 12. 3) Orthodontic theory (Durbeck 1881):- Growth of the jaw Movement of teeth Forward direction Acute infections, Fever, Severe trauma Retardation of forward growth Normally
- 13. 4) Endocrinal theory: Increase or decrease in growth hormone secretion may affect the size of the jaws. 5) Anthropological theory (Mac Gregor 1985) According to this theory human beings alone underwent a period of evolution in which the brain greatly expanded in size and the jaw had to become narrower.
- 14. Mandibular 3rd molars Maxillary 3rd molars Maxillary cuspid Mandibular bicuspids Maxillary bicuspids Mandibular canine Maxillary central and lateral incisors
- 15. In 1930 Berger lists the two main causes of impaction: 1. Local causes 2. Systemic causes
- 16. 1. Irregularity in the position and pressure of an adjacent tooth. 2. The density of the overlying or surrounding bone. 3. Long continued chronic inflammation with increase in density of the overlying mucous membrane. 4. Lack of space due to under developed jaws. 5. Unduly long retention of the primary tooth. 6. Premature loss of primary tooth. 7. Acquired diseases such as necrosis due to infection or abscess
- 17. Systemic causes Prenatal causes Hereditary Miscegenation: Interbreeding of people considered to be of different racial types Post natal causes Rickets Anemia Congenital Syphilis Tuberculosis Endocrine Dysfunction Malnutrition. Rare conditions Cleidocranial dysplasia Oxycephaly Progeria Achondroplasia Cleft palate.
- 18. •There are two types of indications for removing impacted teeth I. Therapeutic indications II. Prophylactic indication
- 20. •Prophylactic removal of a non-erupted tooth is by definition a surgical intervention to prevent future disease. •This practice is often referred to as “removal of asymptomatic third molars”. It is important to define this subject more precisely.
- 21. •Prior to radiation therapy for head and neck malignancies. •Prior to organ transplantation. •Chemotherapy •Bisphosphonate therapy
- 22. •The presence of a third molar in a fracture line. •Prior to orthognathic surgery. •When a third molar may be considered for autogenous transplantation, usually to a first molar region. •When the third molar region is involved in tumor •Resection or jaw reconstruction surgery.
- 23. (1) The routine practice of prophylactic removal of pathology-free impacted third molars should be discontinued in the National Health Service.
- 24. (2) Surgical removal of impacted third molars should be limited to those with evidence of pathology, such as the following: a. Unrestorable caries b. Fracture of tooth c. Non-treatable pulpal and/or periapical pathology d. Pathology of follicle including cyst/tumour e. Cellulitis or abscess formation f. Osteomyelitis g. Tooth/teeth impeding surgery, e.g. reconstructive jaw surgery, preprosthetic/implant surgery, orthognathic surgery.
- 25. (3) Specific attention is drawn to plaque formation and pericoronitis. Plaque formation is a risk factor but is not itself an indication for surgery. The degree to which the severity of recurrence rate of pericoronitis should influence the decision for surgical removal of a third molar remains unclear. • The evidence suggests that a first episode of pericoronitis, unless particularly severe, should not be considered an indication for surgery. • Second or subsequent episodes should be considered as an appropriate indication for surgery.
- 26. Extremes of age Surgical damage to adjacent structures Compromised medical status: Congenital coagulopathies, asthma, epilepsy, etc. Prosthetic considerations Socioeconomic reasons
- 28. Third molars are the only teeth that develop entirely after birth. The stages of the development and eruption of mandibular third molar according to the years : Tooth germ visible 9 yrs Cusp mineralization 11 yrs Crown formation 14 yrs Roots formed (apex open) 18 yrs Eruption 18-24 yrs
- 30. •George Winter’s classification (1926) •Pell & Gregory’s classification (1933) •Killey & Kay’s classification (1979) •Combined ADA & AAOMS classification of procedural terminology
- 31. George Winter’s classification (1926) Based on the relationship of the long axis of the impacted tooth in relation to the long axis of the 2nd molar i. Mesioangular ii. Vertical iii. Horizontal iv. Distoangular v. Buccoangular vi. Linguoangular vii. Transverse viii. Inverted
- 33. Winter’s sub classes • The angle between the occlusal plane or line parallel to it and the longitudinal axis of the impacted third molar. • Winter subclasses as follows: Third molars with negative angles (-0°) Inverted Third molars with an angle between 0° to 30° Horizontal Third molars with an angle between 31° to 60° Mesioangular Third molars with an angle between 61° to 90° Vertical Third molars with an angle (>90°) Distoangular
- 34. • Analysis of the potential anatomic problems involved preparatory to the removal of lower 3rd molar 1. Relation of the tooth to the ramus of the mandible 2. Relative depth of the third molar in bone
- 35. Relation of the tooth to the ramus of the mandible Class I Relative depth of the third molar in bone I. Position A II. Position B III. Position C
- 36. Relation of the tooth to the ramus of the mandible Class II Relative depth of the third molar in bone I. Position A II. Position B III. Position C
- 37. Relation of the tooth to the ramus of the mandible Class III Relative depth of the third molar in bone I. Position A II. Position B III. Position C
- 38. 3. The position of the tooth in relation to the long axis of the second molar i. Vertical ii. Horizontal iii. Inverted iv. Mesioangular v. Distoangular
- 39. a) Based on angulation and position: Same as Winter’s classification b) Based on the state of eruption: Completely eruption Partially erupted Unerupted c) Based on roots: 1) Number of roots - Fused roots ,two roots, multiple roots 2) Root pattern - Surgically favorable -Surgically unfavorable
- 40. Based on clinical and radiographic interpretation of the tissue overlying the impacted teeth. 07220-Soft tissue impaction 07230-Partial bony impaction 07240-Complete bony impaction 07241-Complete bony impaction with unusual surgical complications Combined ADA & AAOMS classification of procedural terminology
- 41. •Quek et al. (2003) classification of impaction •Operative Classification (2010) • Classification of impacted mandibular third molars on cone-beam CT images (2015)
- 42. Vertical impaction (10° to -10°) Mesioangular impaction (11° to 79°) Horizontal impaction (80° to 100°) Distoangular impaction ( -11° to -79°) Others (111° to -80°)
- 43. Quek et al. (2003) classification of impaction, a system of measurement , using protector.
- 44. Operative Classification of Impacted Molars (2010) • The mandibular third molar is classified according to its position relative to the mandibular canal using a standard panoramic x-ray. • There are 3 major types of third molar positions. TMC I Roots of the third molar above the mandibular canal TMC IIa Mandibular third molar roots are in relation to the mandibular canal TMC IIb More than a third of the molar roots are in relation to the mandibular canal TMC III All third molars roots are localized below the mandibular canal
- 45. TMC I TMC II a TMC IIb TMC III
- 46. Classification of impacted mandibular third molars on cone-beam CT images Maglione M. et al (2015) introduce a new radiological classification that could be normally used in clinical practice to assess the relationship between an impacted third molar and mandibular canal on cone beam CT (CBCT) images.
- 47. Class O: The mandibular canal is not visible on the images (plexiform canal). Class 1: The mandibular canal runs apically or buccally with respect to the tooth but without touching it (the cortical limitations of the canal are not interrupted). 1A: The distance IAN and tooth is greater than 2 mm. 1B: The distance IAN and tooth is less than 2 mm
- 48. Class 2: The mandibular canal runs lingually with respect to the tooth but without touching it (the cortical limitations of the canal are not interrupted). 2B: The distance IAN and tooth is less than 2 mm. 2A: The distance IAN and tooth is greater than 2 mm.
- 49. Class 3: The mandibular canal runs apical or buccal touching the tooth. 3A: In the point of contact the mandibular canal shows a preserved diameter. 3B: In the point of contact the mandibular canal shows an interruption of the corticalization.
- 50. Class 4: The mandibular canal runs lingually touching the tooth. 4A: In the point of contact the mandibular canal shows a preserved diameter. 4B: In the point of contact the mandibular canal shows an interruption of the corticalization.
- 51. Class 5: The mandibular canal runs between the roots but without touching them 5A: The distance IAN and tooth is greater than 2 mm. 5B:The distance IAN and tooth is less than 2 mm.
- 52. • Class 6: The mandibular canal runs between the roots touching them. 6A: In the point of contact the mandibular canal shows a preserved diameter. 6B: In the point of contact the mandibular canal shows an interruption of the corticalization. • Class 7: The mandibular canal runs between fused roots
- 53. •WHARFE assessment - Macgregor 1985 •Pederson’s scale (1988) •Parant scale
- 54. Criteria Category Score Winters Classifications Horizontal 2 Distoangular 3 Mesioangular 1 Vertical 0 Height of mandible (mm) 1-30 0 31-34 1 35-39 2 Angulation of 2nd molar (degrees) 1-59 0 60-69 1 70-79 2 80-89 3 90+ 4 WHARFE’S ASSESSMENT by McGregor 1985
- 55. Root shape & development Complex 3 (more than 2/3 complete) Unfavorable curvature 2 (less than1/3 complete) Favorable curvature 1 Follicles Normal 0 Possibly enlarged -1 Enlarged -2 Impaction relieved -3 Path of exit Space available 0 Distal cusps covered 1 Mesial cusps also covered 2 Both covered 3 TOTAL 33
- 56. Difficulty index for removal of third molar (PEDERSON’S SCALE, 1988) ANGULATION/SPATIAL RELATIONSHIP Mesioangular 1 Horizontal/Transverse 2 Vertical 3 Distoangular 4 DEPTH Level A 1 Level B 2 Level C 3 Difficulty index for removal of third molar (PEDERSON’S SCALE, 1988) RAMUS RELATIONSHIP Class I 1 Class II 2 Class III 3
- 57. Modified Pederson’s Difficulty index Pederson’s Difficulty index Very difficult : 7 to 10 Moderately difficult : 5 to 7 Minimally difficult : 3 to 4 • Very difficult = 7–10 • Moderately difficult = 5–6 • Slightly difficult = 3-4
- 58. Easy I Extraction requiring forceps only Easy II Extraction requiring osteotomy Difficult III Extraction requiring osteotomy and coronal section Difficult IV Complex extraction ( root resection)
- 59. Difficulty index for removal of third molar (Kharma scale ,2014) ANGULATION/SPATIAL RELATIONSHIP Mesioangular 0 Horizontal/Transverse 1 Vertical 2 Distoangular 3 DEPTH Level A: high occlusal 1 Level B: medium occlusal 2 Level C: deep occlusal 3
- 60. ROOTS FORM Convergent 0 Divergent 1 Bulbous 2 RAMUS RELATIONSHIP Class I: Sufficient Space 0 Class II: Reduced Space 1 Class III: No Space 2
- 61. Modified Difficulty index (According to the Kharma’s scale) Very difficult 7–10 Moderately difficult 5–6 Slightly difficult 3-4 Easy 1-2
- 62. Occlusal view Coronal section
- 63. i. Lingual plate ii. Musculature iii. Neurovascular Bundle iv. Bone trajectories of mandible v. Retromolar triangle vi. Facial artery and vein vii. Lingual nerve viii.Mylohyoid nerve ix. Long buccal nerve
- 64. • A line of stress extends from one condyle to the other passing along the symphysis. • A number of trajectories radiate down below the roots of teeth
- 65. Surgical implication of trajectories • Importance lies in use of chisel for bone removal. • Buccal horizontal cut may extend from 1st molar till distal to 3rd molar till ramus and cause fracture. • To prevent from such incident vertical stop cut need to be placed mesial and distal to the 3rd molar
- 66. • The lingual plate is the side of the lower jaw tooth socket nearest the tongue. • In the region of the lower 3rd molar. • The lingual plate can often be very thin. Surgical implications • Because of the extreme thinness of the lingual plate the apices of lower third molar frequently perforates it. • Attempted elevation of fractured roots may lead to their displacement through the thin lingual cortex into the 'lingual pouch'.
- 67. Fracture of lingual plate: • Difficulty will be experienced in retrieving such dislodged root fragments. • Rarely the whole tooth may be pushed into the lingual pouch. Whole tooth may be displaced into the lingual pouch under the mylohyoid muscle
- 68. Musculature The various muscles surrounding the third molar region are: • Buccinator - Anteriorly • Temporalis - Distally • Masseter - Laterally • Medial Pterygoid And Mylohyoid - Medially
- 69. ―This horseshoe-shaped muscle forms the musculature of the cheek. ―Inserted along the external oblique ridge and continues along the pterygomand raphe. Surgical implication ―During surgical removal deeply seated impacted tooth require detachment of this muscle – Lead to postoperative swelling, trismus & pain.
- 70. • This fan-shaped muscle is inserted on the coronoid process and anterior border of mandible. • Two tendons can be noticed where the muscle attaches to the anterior border of mandible: outer and inner tendon • Surgical implication ―During buccal approach for the removal of third molars, the outer tendon has to be sectioned to enable reflection of the flap. ― This in turn will help to remove adequate bone from the buccal and distal side.
- 71. ―This muscle is inserted into the lateral side of the ramus from the coronoid process up to the angle. ―Rarely involved in third molar surgery. ―Postoperative edema may involve posteriorly to the muscle leading to trismus and pain.
- 72. ―Its inserted on the medial aspect of mandible in the angle region. ―Not directly involved in third molar surgery. ―But during lingual approach postoperative edema involve this muscle which can lead to trismus due to secondary involvement of the muscle
- 73. ―This muscle is inserted on the mylohyoid line from canine to the third molar region. ―During lingual approach this muscle can partly sever may lead to transient swallowing difficulty. ―Postoperative infection can spread to sublingual / submandibular space through this muscle breakage.
- 74. The neurovascular bundle contains the inferior alveolar artery, vein and nerve enclosed in a fascial sheath. The radiographic evaluation of the relationship of the mandibular canal and roots of the third molar forms an important part of the preoperative assessment.
- 75. The inferior alveolar canal deroofed as part of a marginal mandibular resection showing neurovascular vessels in third molar region. The vein (V) lies superiorly, and the artery (A) lies lingually and superiorly. The inferior alveolar nerve (N) lies below. Castellon et al performed a prospective study in 1117 patients and concluded that patient age, ostectomy of the bone distal to the third molar, the radiologic relationship between the roots of the third molar and the mandibular canal, and deflection of the mandibular canal increased the risk of IAN damage. ( Incidence 5%)
- 76. • Kilic et al performed a study to identify the position of the mandibular canal through direct measurement and to determine the branches of the inferior alveolar nerve through histologic examination on 26 human cadavers They concluded that the mandibular canal was located at a mean distance of 10.52 mm above the inferior margin of the mandible. (Clinical Anatomy 23:34–42 (2010)) • Miloro et al conducted a radiographic study to determine the distance between mandibular third molars and the mandibular canal using OPGs They concluded that unerupted molars and mesioangular impacted molars were most closely positioned and were risk factors for post op paresthesia (OOOO journal 2005; 100: 545-9) • Levine et al conclude that the IAN canal was 4.9 mm and 17.4 mm from the buccal and superior cortical surfaces of the mandible, respectively. Older patients and white patients, on average, have lesser distance. ( JOMS 65: 470-474;2007)
- 77. • Depressed roughened area – bounded by buccal & lingual crest. • Lateral to this – retromolar fossa. Through this branches of retromolar nutrient vessels emerges and supply temporalis tendon, buccinator muscle and adjacent alveolus • Surgical implication • If the distal incision is extended on ramus instead of extending over cheek – cause injury to retromolar nutrient vessels – lead to rapid bleeding. • Excessive distal extension of incision may cause incision of temporalis attachments and may lead to post operative trismus
- 78. • Cross the inferior border of mandible anterior to masseter muscle near to 2nd molar • Surgical implication Injury may occur due to slippage of the BP blade while making vertical realising incision. It is better to start incision from buccal sulcus then extend upward to the tooth.
- 79. •The lingual nerve lies on the medial aspect of the third molar. •Frequently lingual nerve courses submucosally in contact with the periosteum covering the lingual wall of the third molar socket or it may run below and behind the tooth.
- 80. • The average diameter of the nerve was 1.86 mm. • In the lower third molar region 61.7% of the lingual nerves were round. • Out of 256 cases, 4.5% cases showed that the nerve lied above the alveolar crest
- 81. Four anatomical risks of lingual nerve: ( Len Tolstunov 2007) • Lingual version of distoangular impacted lower 3rd molar • Root of few distoangular 3rd molar directed lingually – lingual version – increase the vulnerability with lingual nerve •Lingual plate deficiency • Root Apices of third molar penetrate the lingual plate – deflected into lingual pouch – injure the lingual nerve • High lateral position of lingual nerve • Lingual nerve can be in full contact with lingual plate / above the lingual plate – increase vulnerability of lingual nerve • Local chronic inflammatory condition • Long standing pericoronal infection lead to scaring of lingual nerve with lingual plate • If lingual plate is deficient then its tend to attached with the 3rd molar tooth
- 82. Mylohyoid nerve • This nerve leaves IAN before it enters into mandibular canal • Then penetrate the sphenomandibular ligament.
- 83. Long buccal nerve •Emerges through the buccinator and passes anteriorly on its outer surface
- 84. • The operation of removing a lower third molar can have serious complications if it is not planned with some care. • All features like size, shape, position of the tooth and consistency of bone can all be demonstrated on a radiograph.
- 86. Radiographs Linear cross sectional tomography Lateral oblique view
- 87. •Position & depth of impacted tooth •Root pattern of impacted teeth •Shape of crown •Texture of investing bone •Relation to inferior alveolar canal •Position & root pattern of second molar
- 88. • hite Line • Provide information regarding the depth & inclination • Amber Line • Indicate the margin of the alveolar bone enclosing the teeth. • One must differentiate between external oblique ridge and bone lying distal to impacted tooth. • Red Line • Provides information about depth at which elevator should be applied • Longer the line difficult to remove/access the tooth • Length : difficulty :: 1 : 3
- 89. •In 1990, Rood and Shehab , in a literature review, collected seven radiographic indicators of a close relationship between the lower 3rd molar and the inferior alveolar canal.
- 90. Narrowing of root Bifid root apex Darkening of root Deflection of root Related to inferior alveolar canal
- 91. Diversion of canal Interruption in white line of canal. Narrowing of canal Related to inferior alveolar canal
- 92. • Helps to show relationship of root apices with inferior dental canal or the maxillary sinus floor • Useful to predict the bone density of mandible • Useful for obtaining a 3D spatial orientation of the third molar inside the mandible/ maxilla
- 93. Use of CBCT
- 94. • Indications: 1. When OPG suggest close relationship between root apex and madibular canal 2. Information about distance between IAN & lower tooth root 3. Prediction for risk of damage of IAN. • Advantages : 1. Radiation exposure 10 times less than regular CT scan 2. Required less time(10-40 sec) than conventional CT 3. Price is comparatively less than CT scan (<50%) CBCT Scan
Editor's Notes
- Lytle (1979) Impacted tooth is one that has failed to erupt into normal functional position beyond the time usually expected for such appearance. Eruption is prevented by adjacent hard or soft tissue including tooth, bone or dense soft tissue.
- Heredity is most common cause. The hereditary transmission of small jaws and large teeth from parents to siblings.
- Impaction may also be found where no local predisposing conditions are present.
- Impaction may also be found where no local predisposing conditions are present.
- The National Institute of Clinical Excellence (NICE) of England in March 2000
- Healing Longer recovery periods Difficult - more densely calcified bone Bone removal is more due to reduced PDL space If benefits healing than complication, don’t extract – Can be used as abutment
- Mesioangular – Most common type(43%) because mandibular third molars follow an mesial inclination while eruption, least difficult to remove but most damaging Vertical - 2nd most common type(38%) Horizontal - 3% Distoangular - Most difficult to remove (6%) Buccoangular Linguoangular Transverse Inverted
- Sufficient space available b/w anterior border of ascending ramus and distal side of 2nd molar for the eruption of 3rd molar
- Space available is less than mesiodistal width of crown of third molar
- Absolute lack of space, 3rd molar completely within ramus
- They may also occur in a) buccal deflection b) Lingual deflection c) torsion
- Quek’s study: Angle formed between long axis of 2nd & 3rd molars using orthodontic protractor
- The present classification is a simple and easy-to-apply method for the surgical management of third mandibular molars and can be extended for any ectopic or impacted mandibular tooth.
- TMC I Roots of the third molar above the mandibular canal TMC IIa Mandibular third molar roots are in relation to the mandibular canal
- The height of the mandible is measured from the distal profile of the amelocemental junction to the nearest point on the lower border of the jaw. The angle of the second molar is that made by the long axis of that tooth to a fiducial horizontal line
- Exit path. The tooth is rotated about the midpoint of the amelocemental junction and the point at which the shadow of the coronoid process crosses the crown is noted. In the example shown a mesioangular tooth when rotated is seen to have only the distal cusp completely covered.
- The lower third molar tooth is situated at the distal end of the body of the mandible where it meets a relatively thin ramus. The tooth is embedded between the thick buccal alveolar bone and a thin lingual cortical plate
- It is attached to the maxilla at the level of the apices of molar roots.
- The outer tendon is inserted to the anterior border of coronoid process. The inner tendon is attached to the temporal crest of mandible. The retromolar fossa is found in between these tendons.
- Most prevalent types of retromolar triangles, according to Suazo et al.,2007 Tapering form 9.16%; Drop form 10.83%; Triangular form 80%.
- Because of lingual retromolar anatomy, the surgeon must take into consideration the proximity of the lingual nerve to the third molar region. Damage to this nerve with its intimate relationship with the chorda tympani may result in loss of taste and lingual salivary gland secretion, in addition to loss of sensation in the anterior two-thirds of the tongue on the affected side. By averaging data from several recent studies, the mean vertical distance of the nerve from the distolingual alveolar crest in the region of the mandibular third molar was found to be about 4.45 mm, and the average horizontal distance of the nerve to the lingual cortex was 2.18 mm.
- Surgical implication In 16% of cases this nerve present in too close proximity of canal Damage may take place during lingual approach for removing 3rd molar tooth.
- Surgical implication During wide opening of mouth it lies above the retro molar fossa region. Injury is rare but can occur if incision is placed too laterally into the buccal mucosa
- A diagnostic technique for determining the buccolingual relationship of impacted mandibular third molar and inferior alveolar neurovascular bundle Mandibular occlusal views are useful for determination of bucco-lingual placement of the tooth within the mandible
- A diagnostic technique for determining the buccolingual relationship of impacted mandibular third molar and inferior alveolar neurovascular bundle
- Assessment of position and depth of the impacted tooth in alveolar bone Using roots of 2nd molar, occlusal plane and alveolar crest between second & third molar as a guide
