The document provides information on condylar fractures, including:
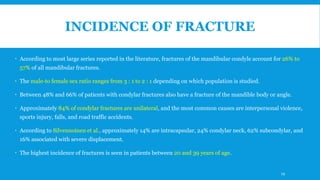
1. Condylar fractures account for 26-40% of all mandible fractures and can result in pain, dysfunction and deformity if not treated properly.
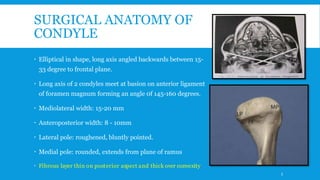
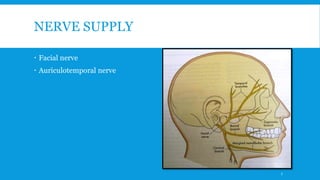
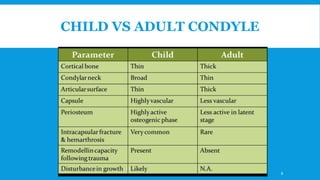
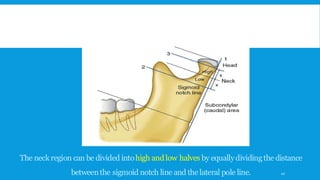
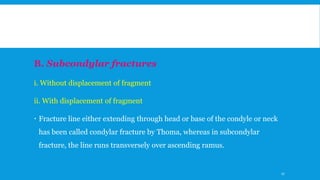
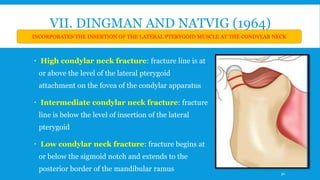
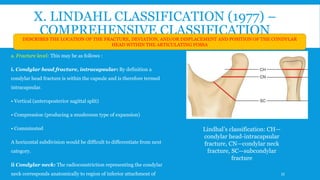
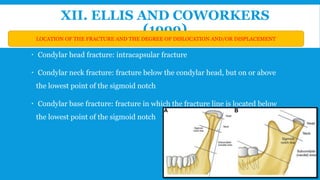
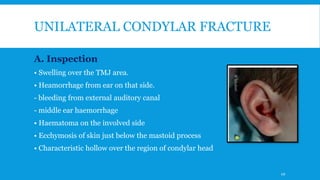
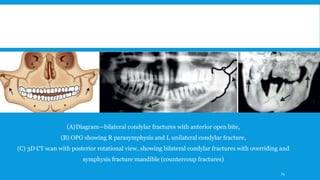
2. The condyle has a unique anatomy and is an important growth center for the mandible. Fractures can occur in the condylar head, neck or subcondylar region.
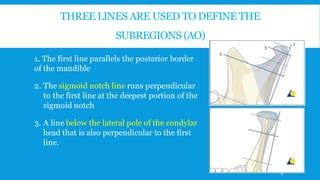
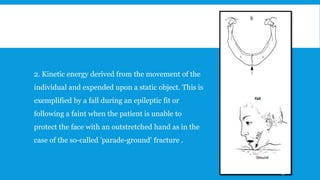
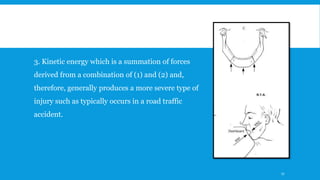
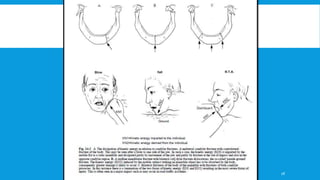
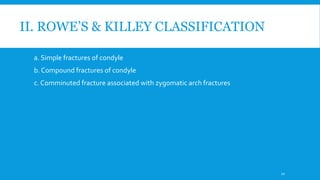
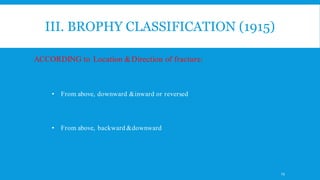
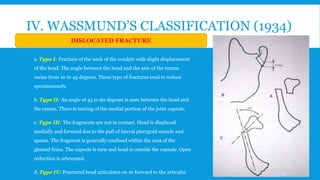
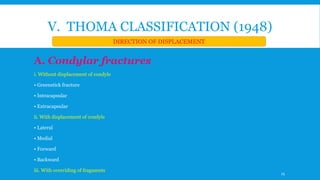
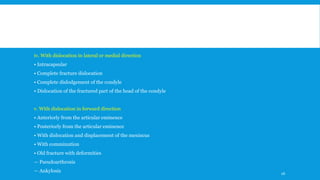
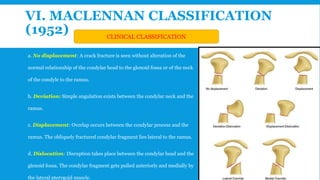
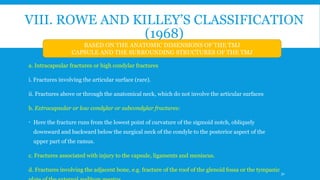
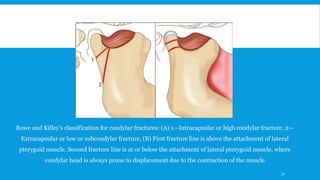
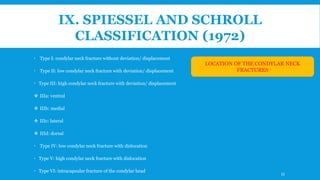
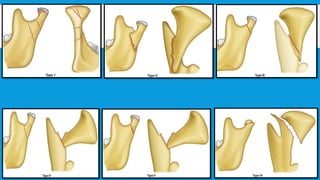
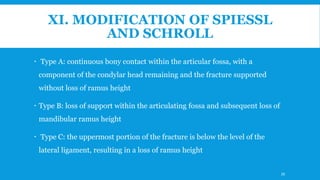
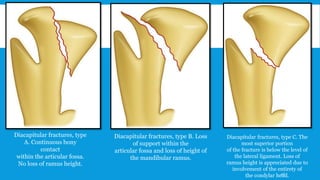
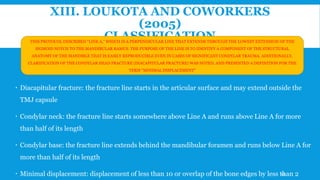
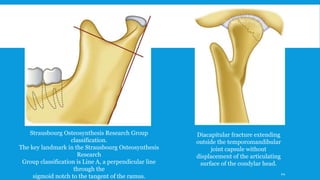
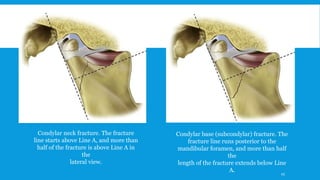
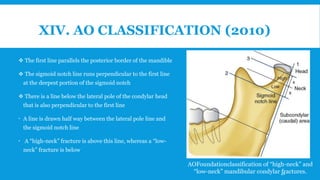
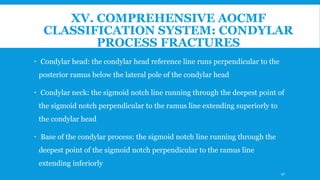
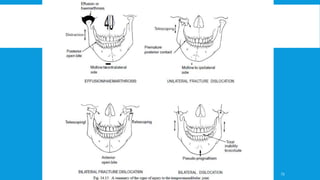
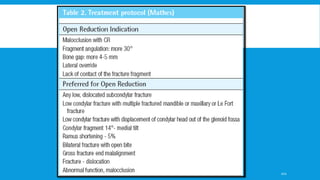
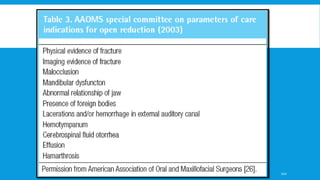
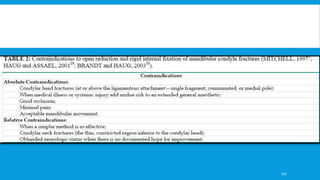
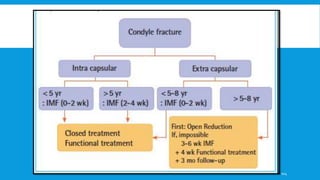
3. Various classification systems are described that categorize fractures by location, degree of displacement, and direction of forces involved. Accurate classification is important for determining appropriate treatment.