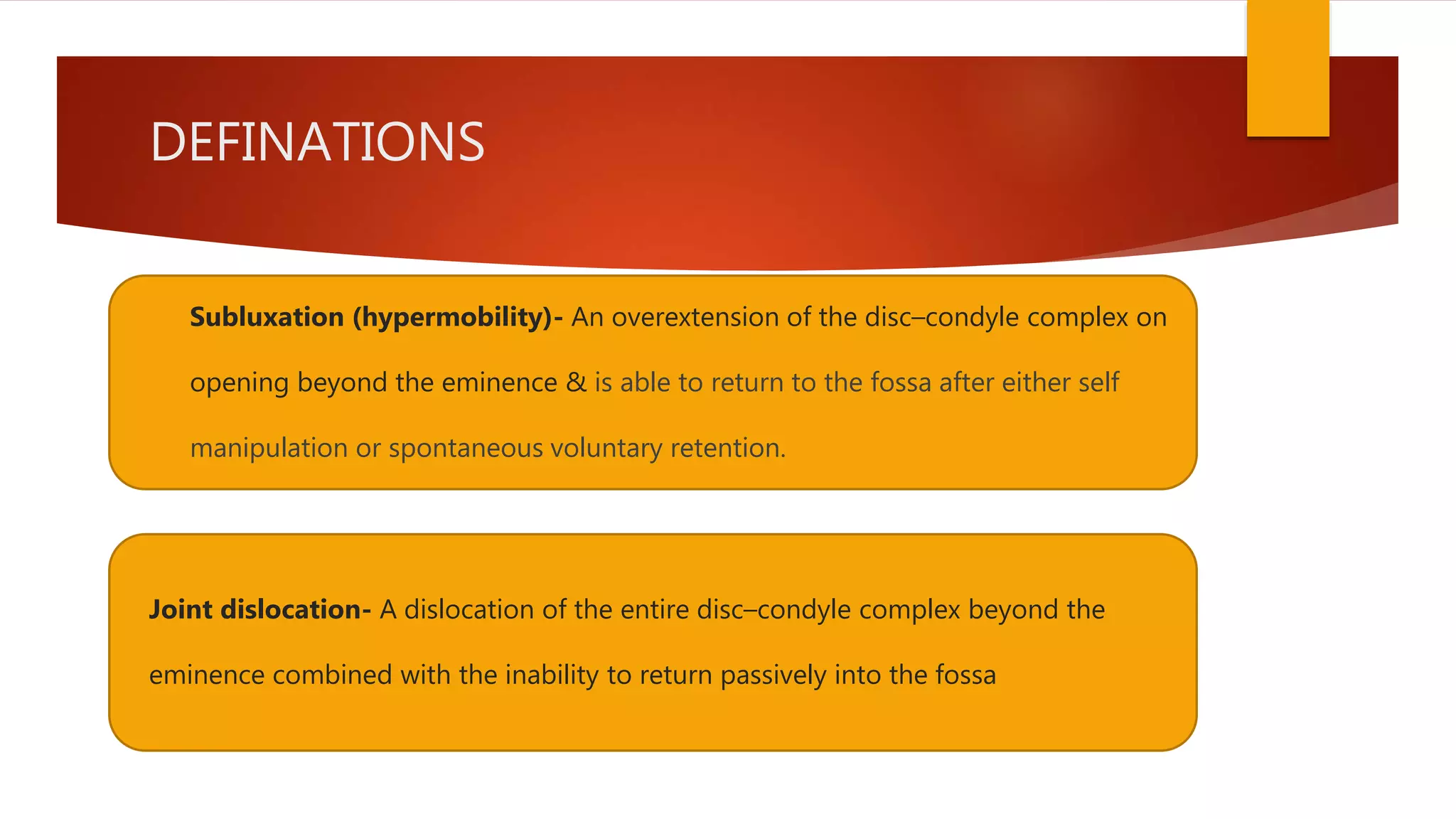
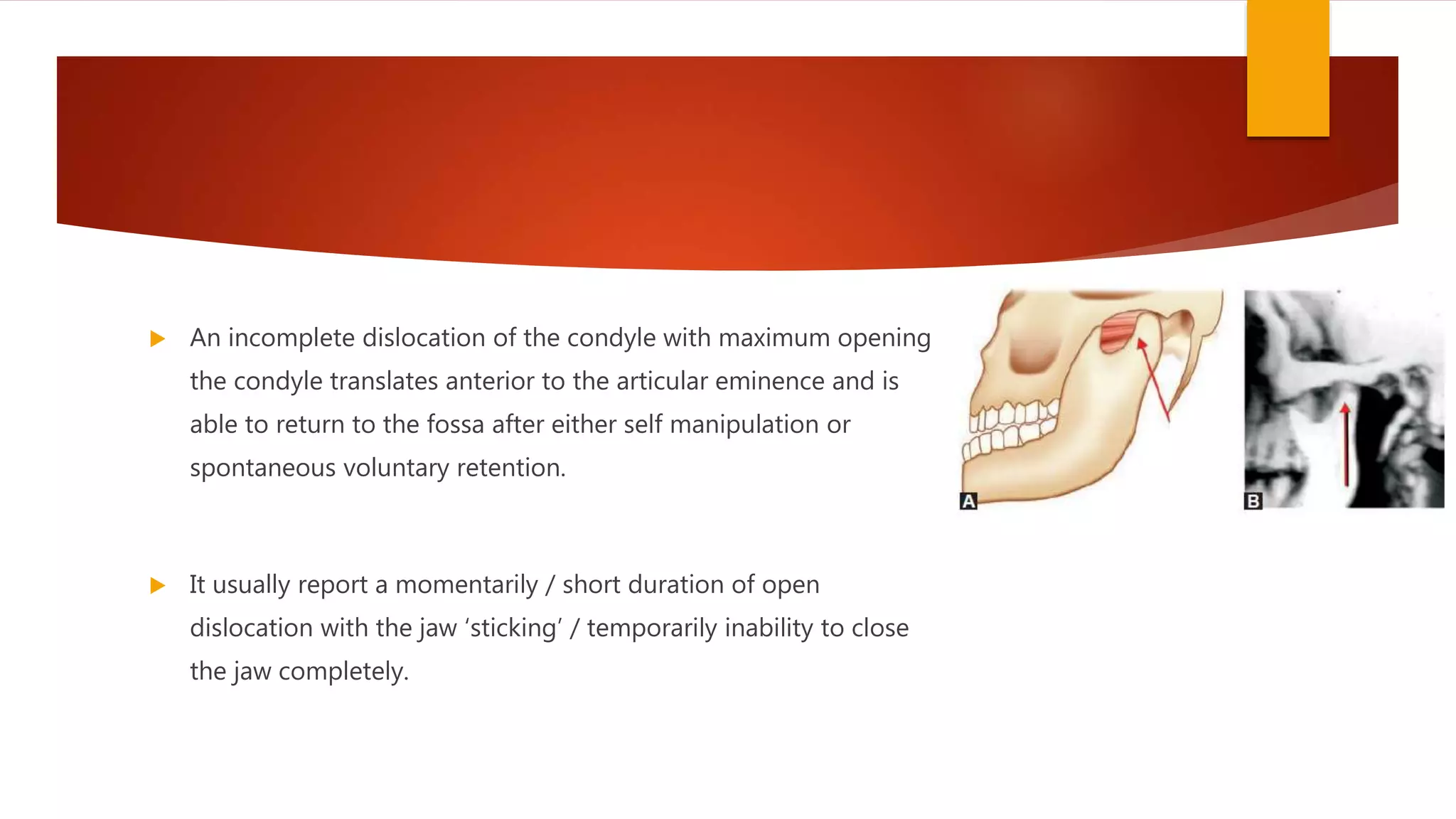
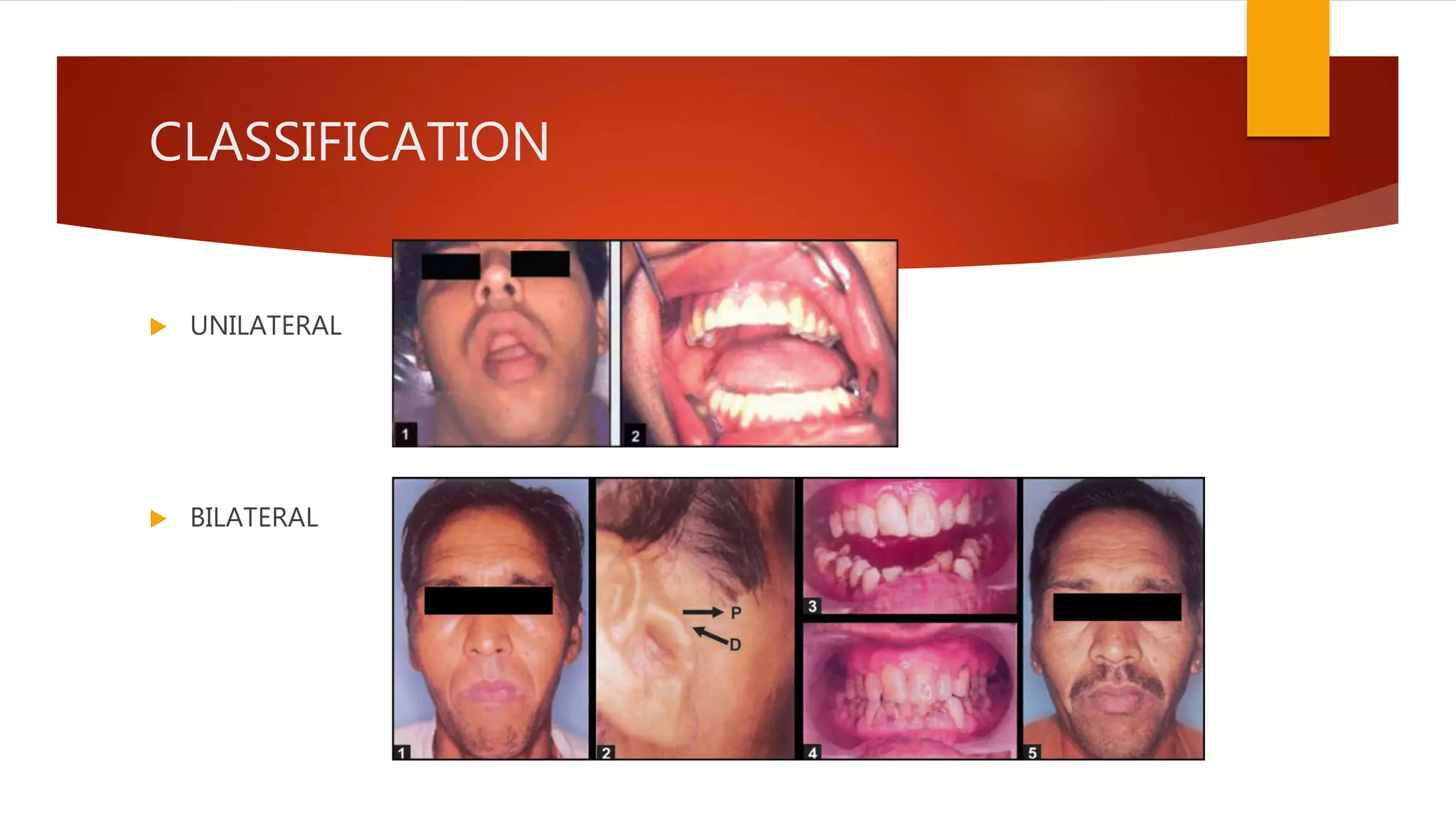
1) Hypermobility of the temporomandibular joint (TMJ) refers to excessive translation of the condyle beyond the articular eminence on opening. Subluxation involves reduction of the condyle whereas dislocation prevents reduction.
2) Causes of hypermobility include trauma, connective tissue disorders, internal derangements and occlusal discrepancies. Chronic dislocation can be long-standing, recurrent or habitual.
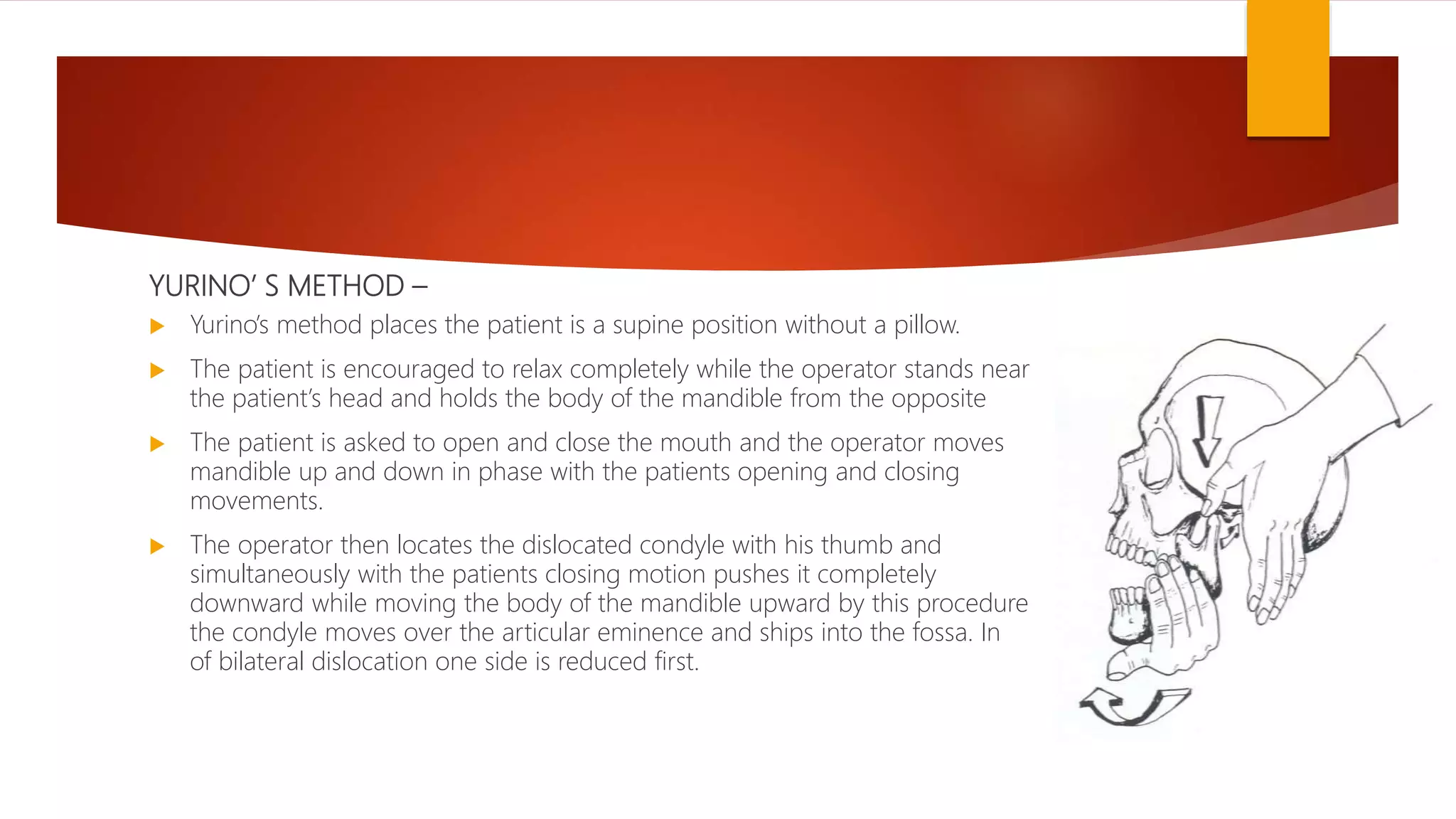
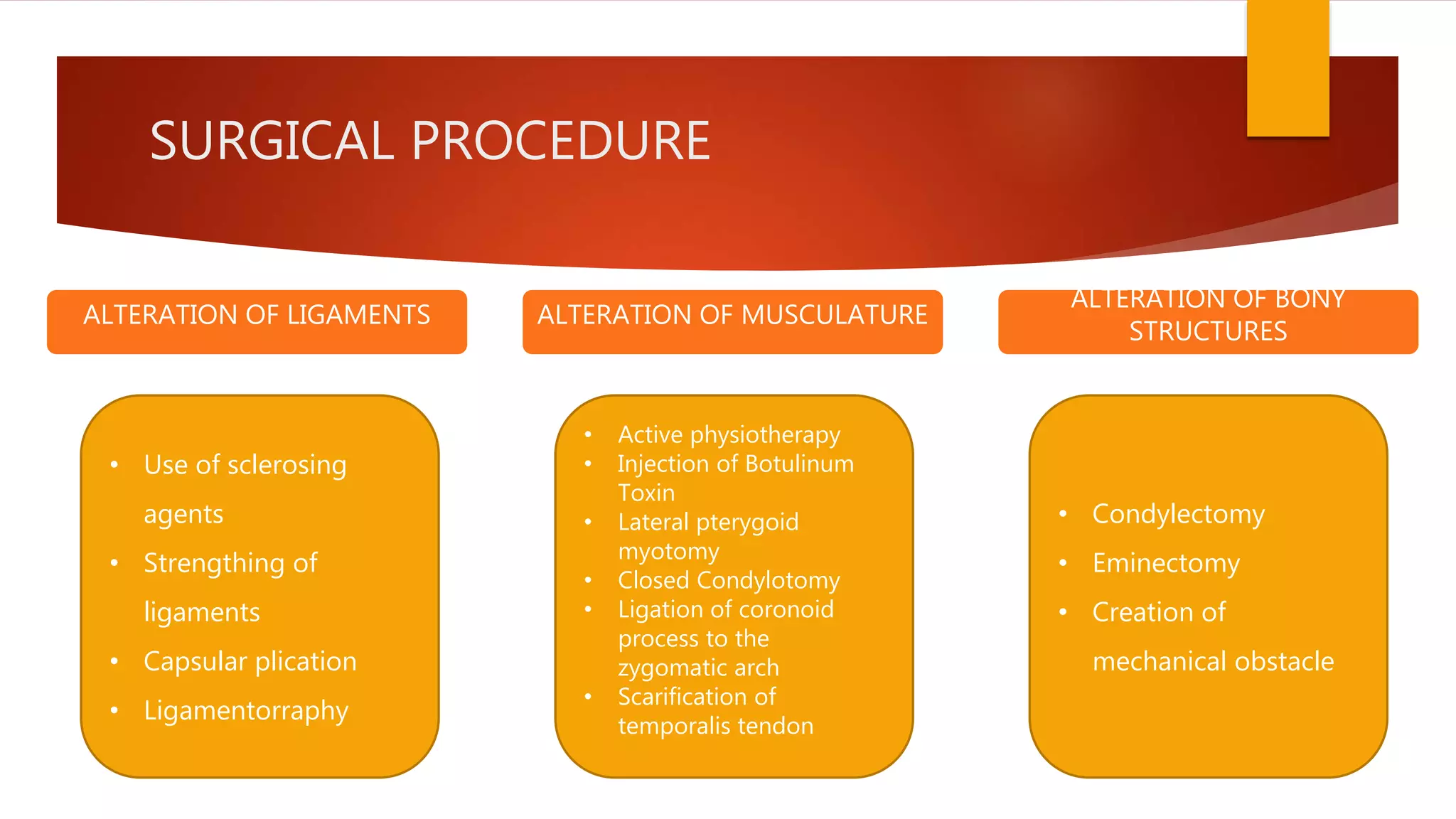
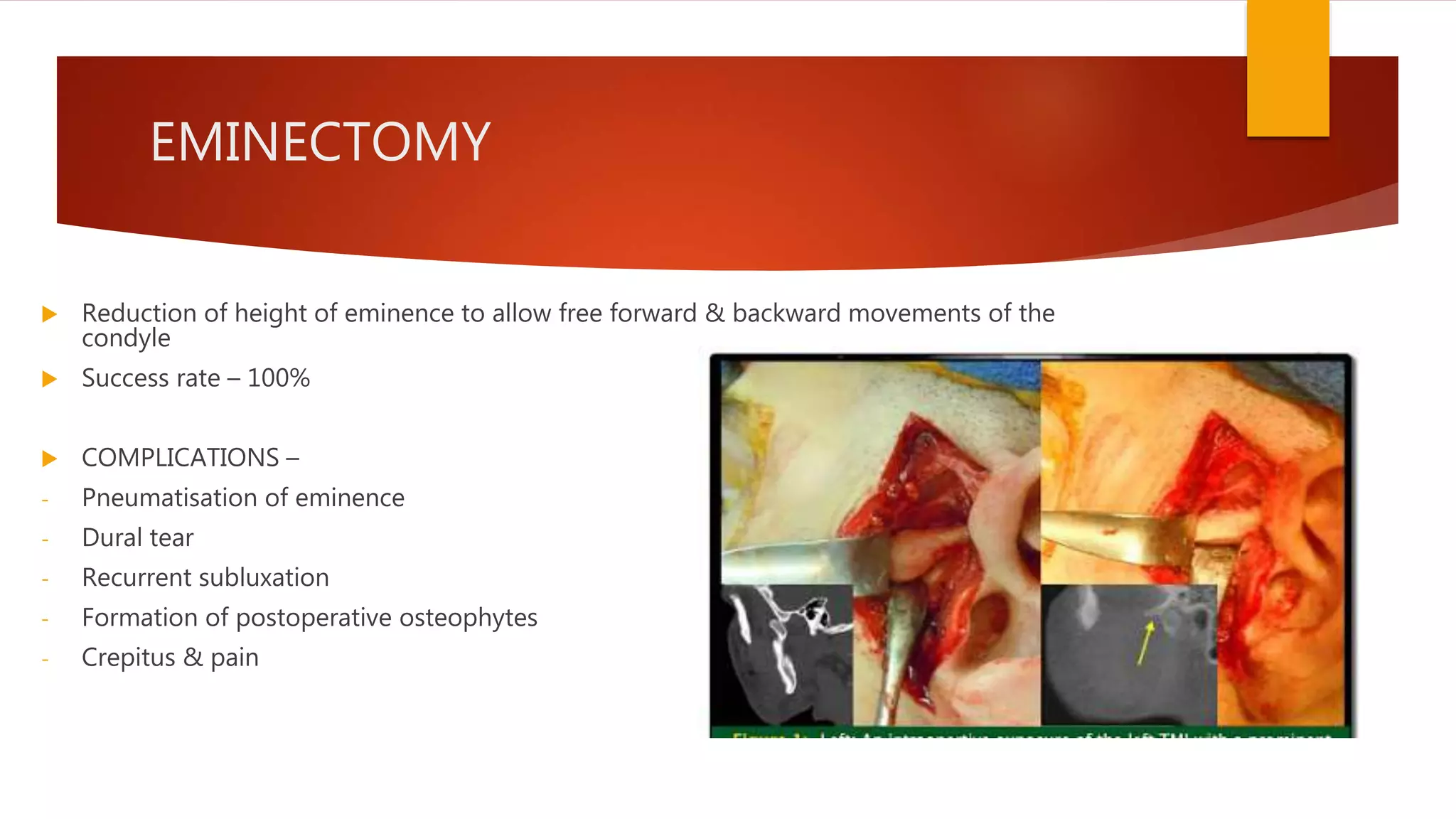
3) Treatment depends on the severity and chronicity of the condition. More severe or chronic cases may require surgery like eminectomy while milder cases can be managed with exercises, injections or occlusal splints.