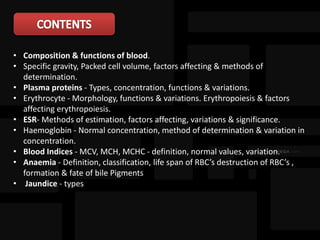
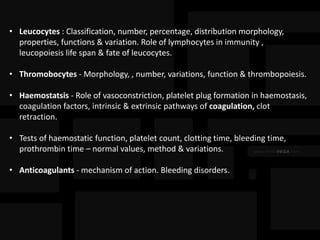
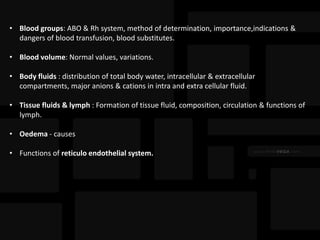
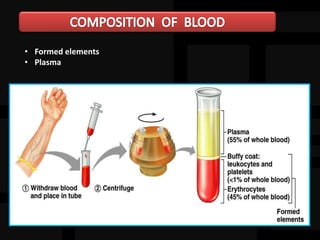
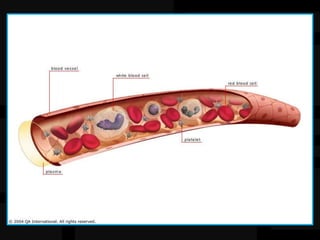
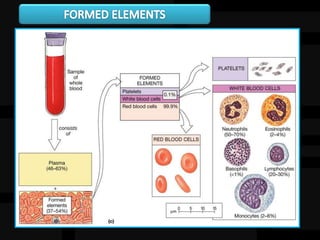
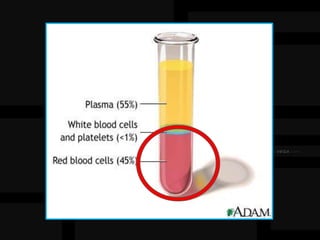
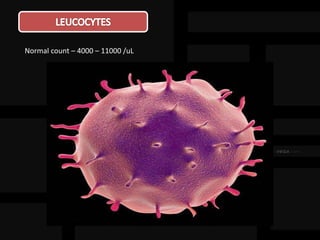
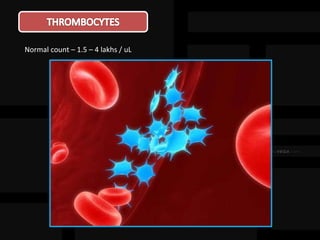
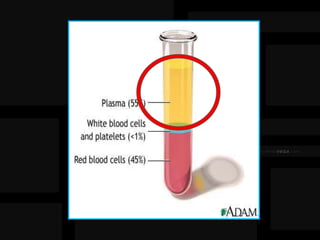
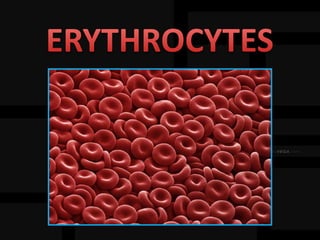
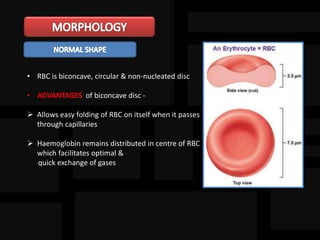
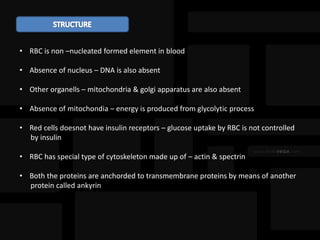
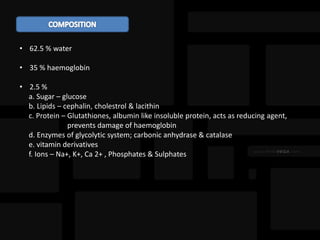
1. The document discusses the composition and functions of blood. It describes the formed elements of blood including erythrocytes, leukocytes, and thrombocytes.
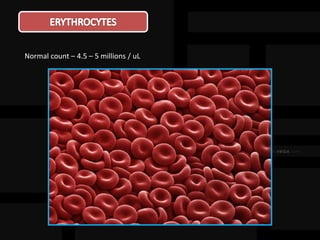
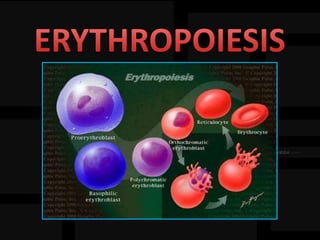
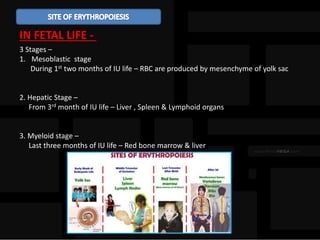
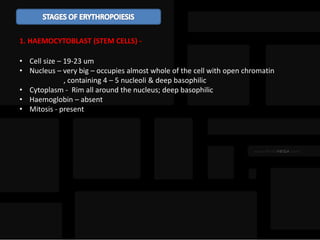
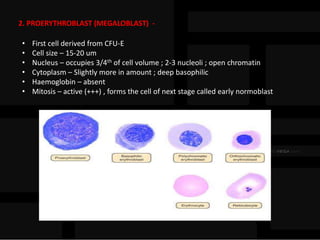
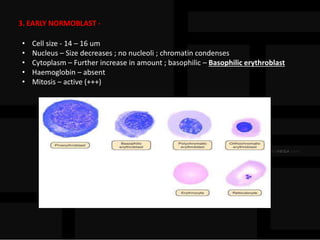
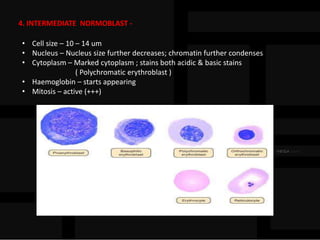
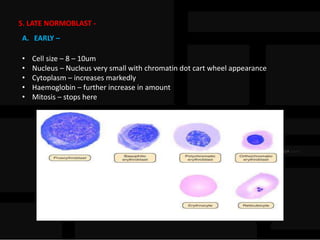
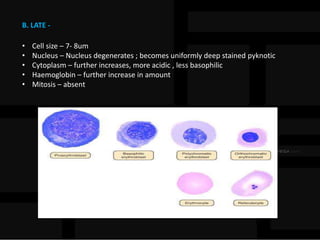
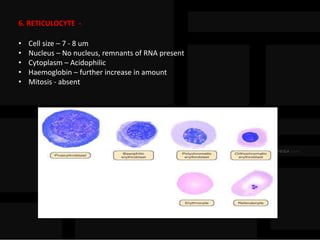
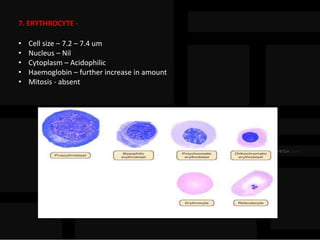
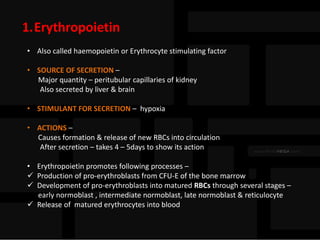
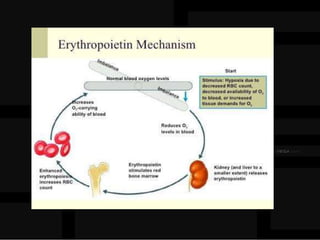
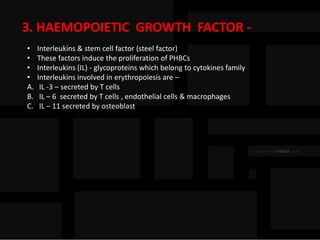
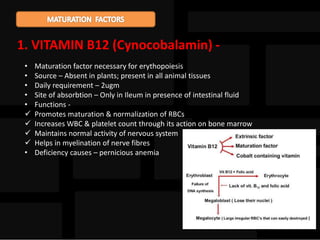
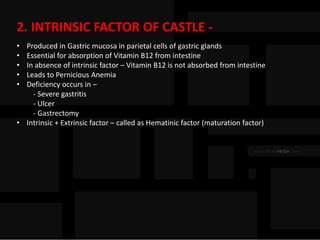
2. The stages of erythropoiesis and factors affecting erythropoiesis are explained. Erythropoiesis occurs within the red bone marrow in adults and produces red blood cells through stem cell differentiation.
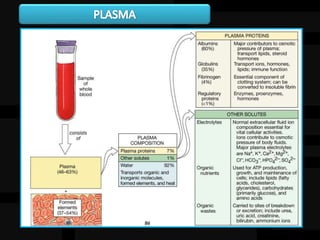
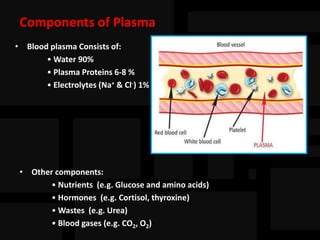
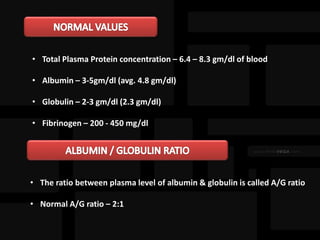
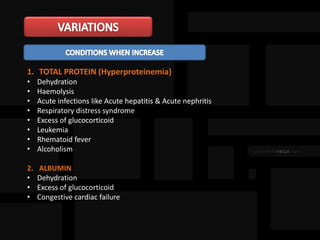
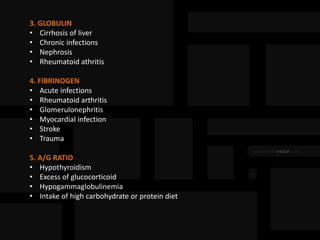
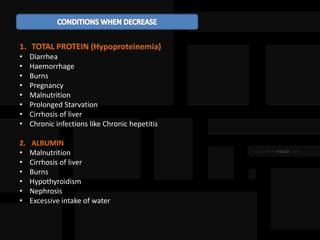
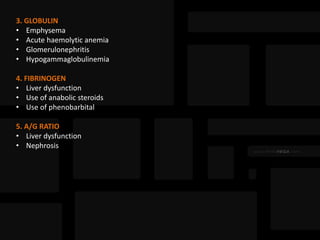
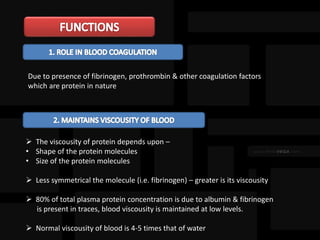
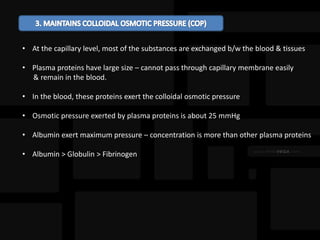
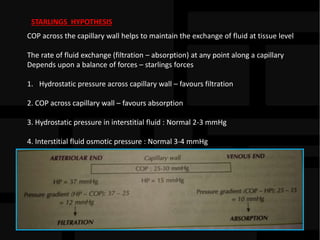
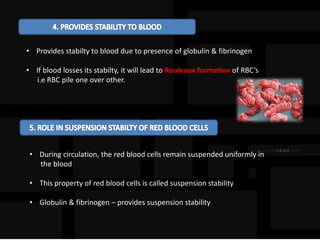
3. The functions of plasma and plasma proteins are outlined. Plasma proteins such as albumin help maintain colloid osmotic pressure and transport substances through the blood.