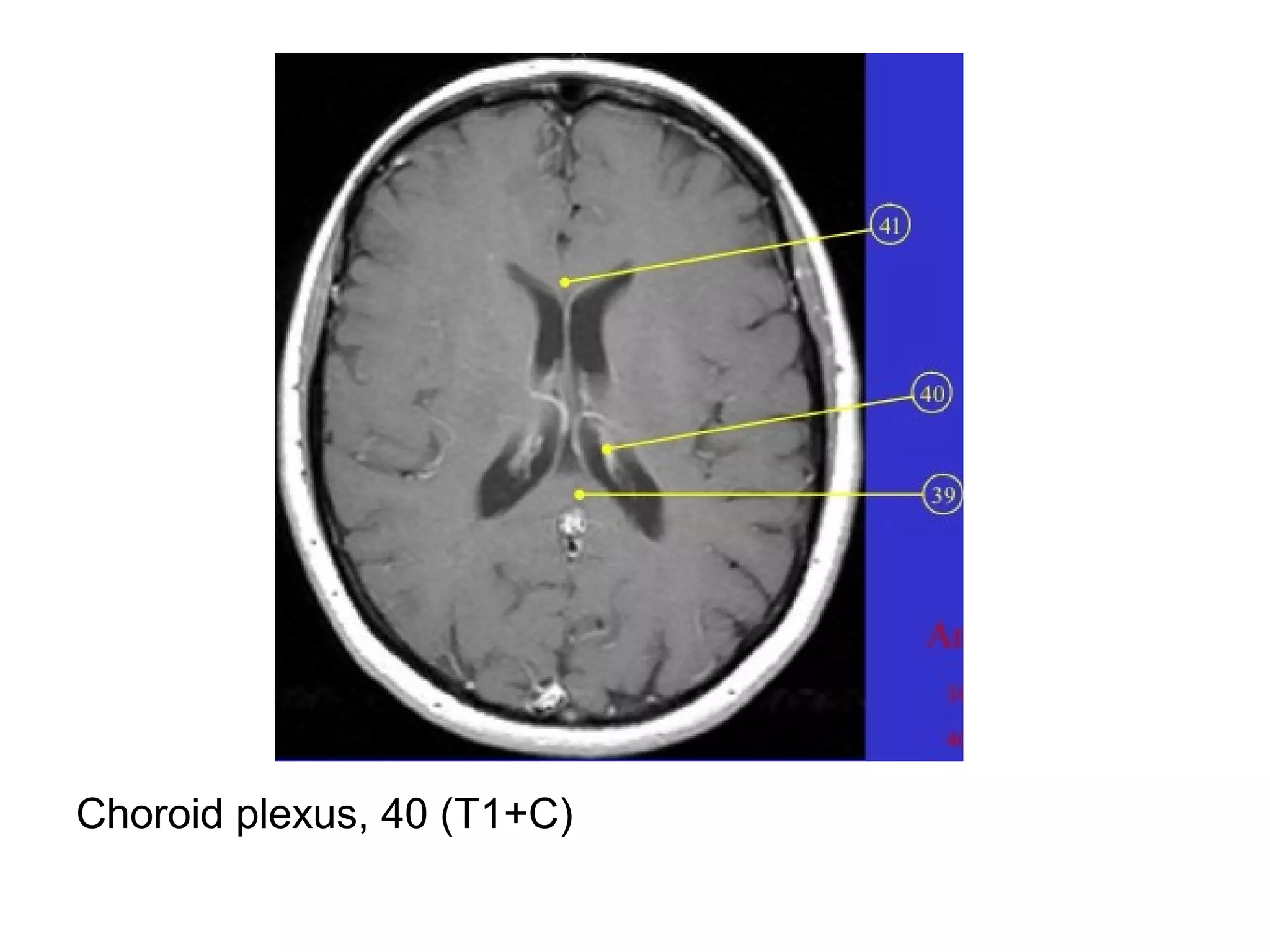
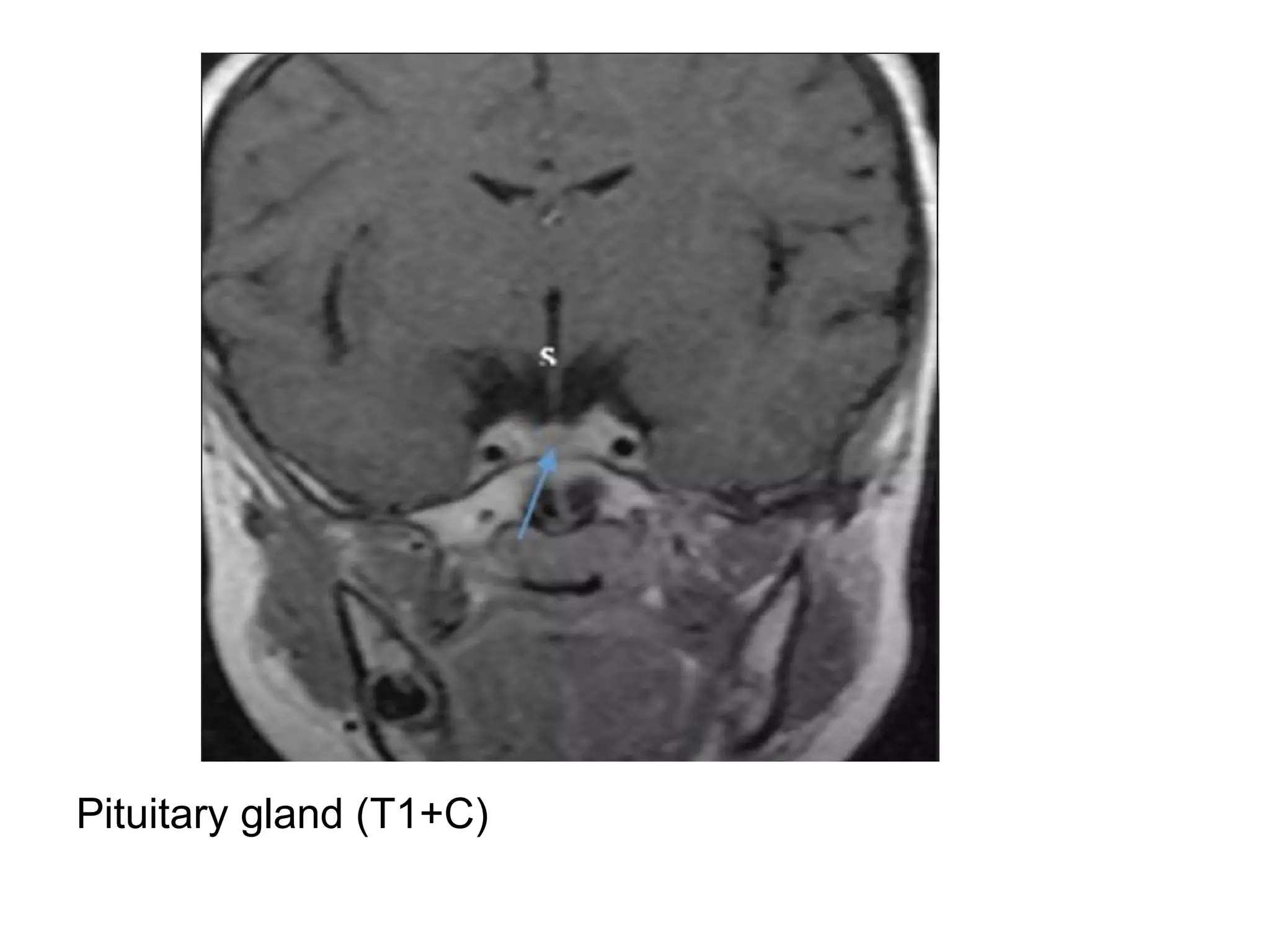
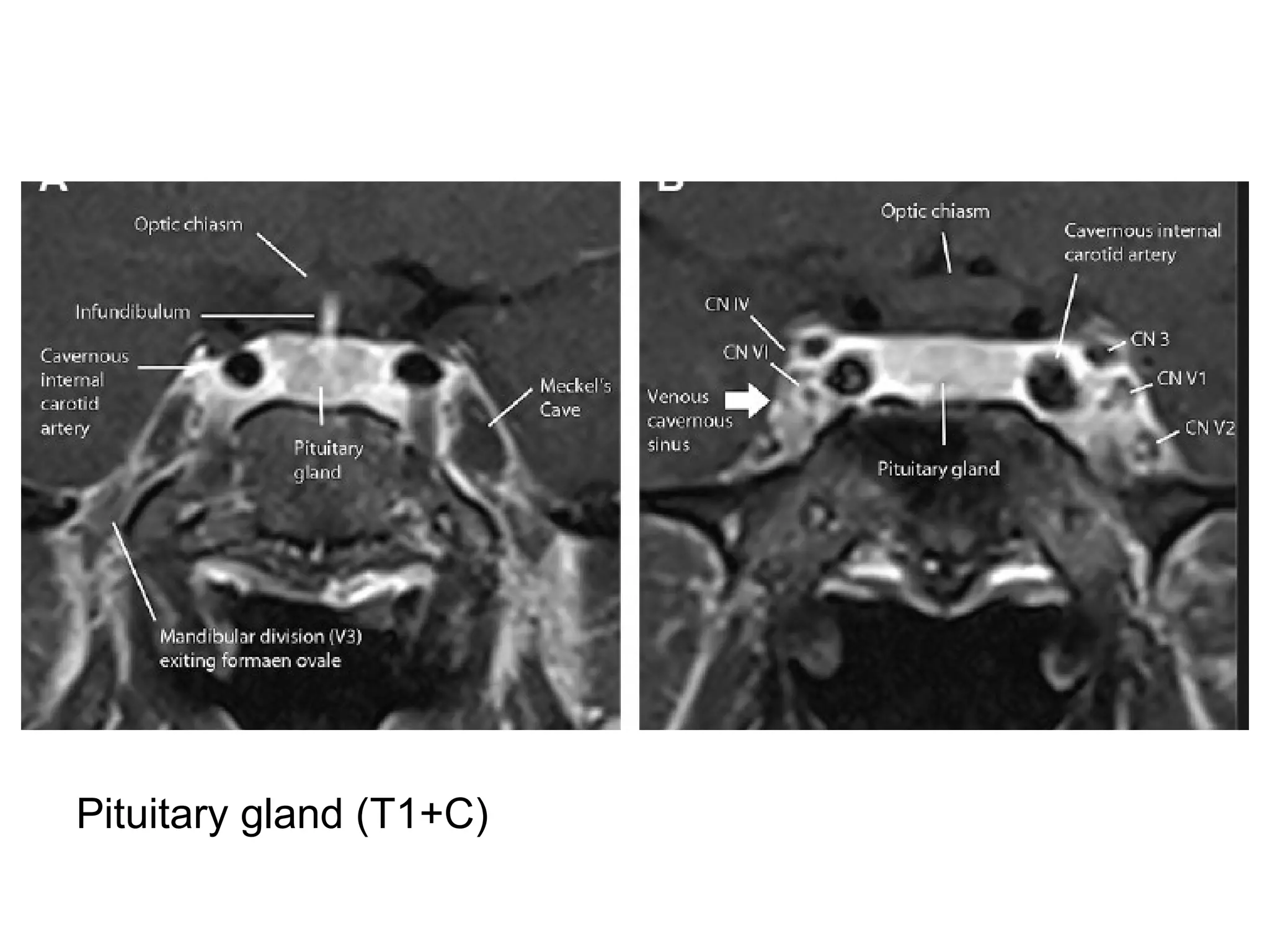
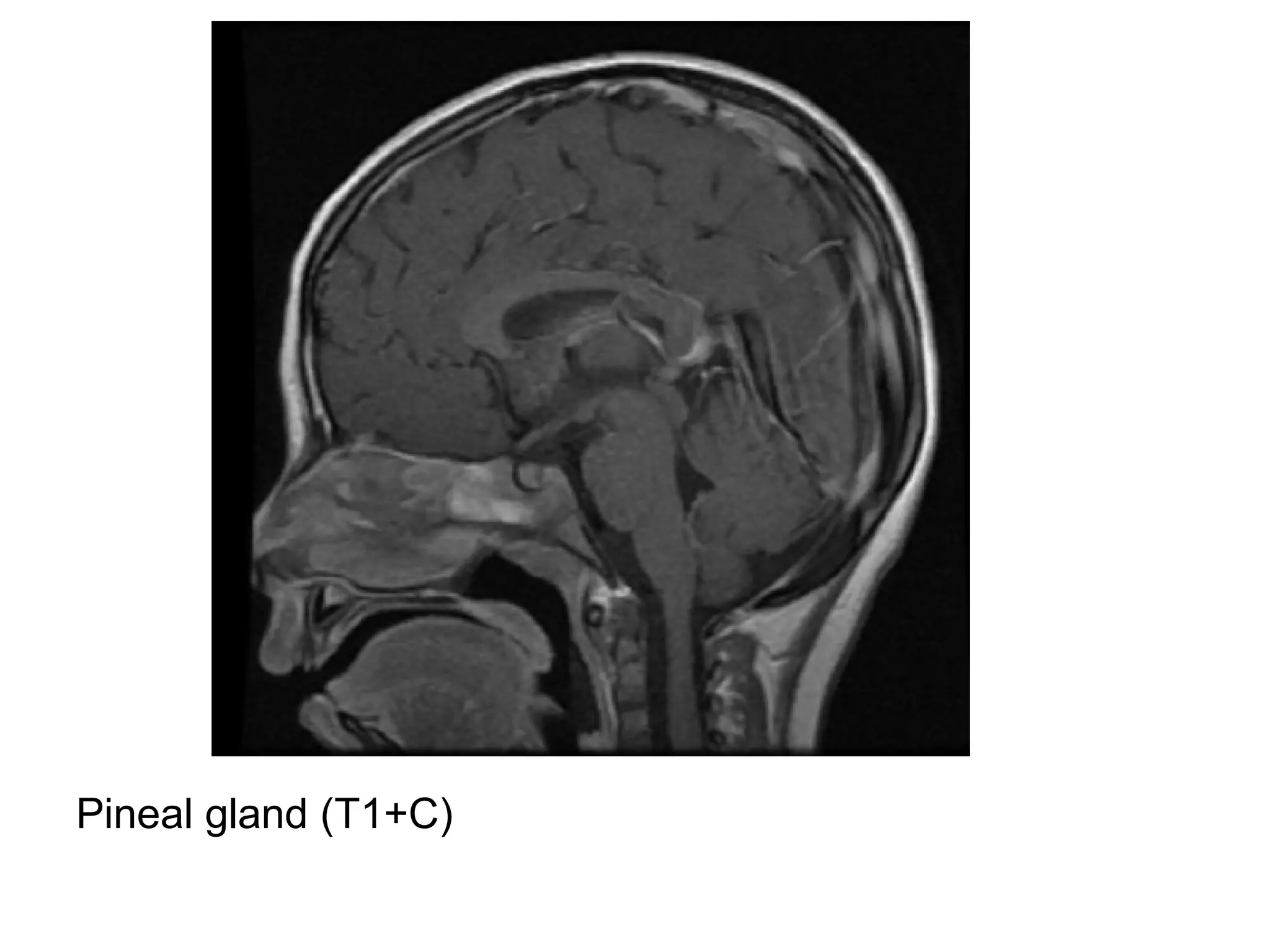
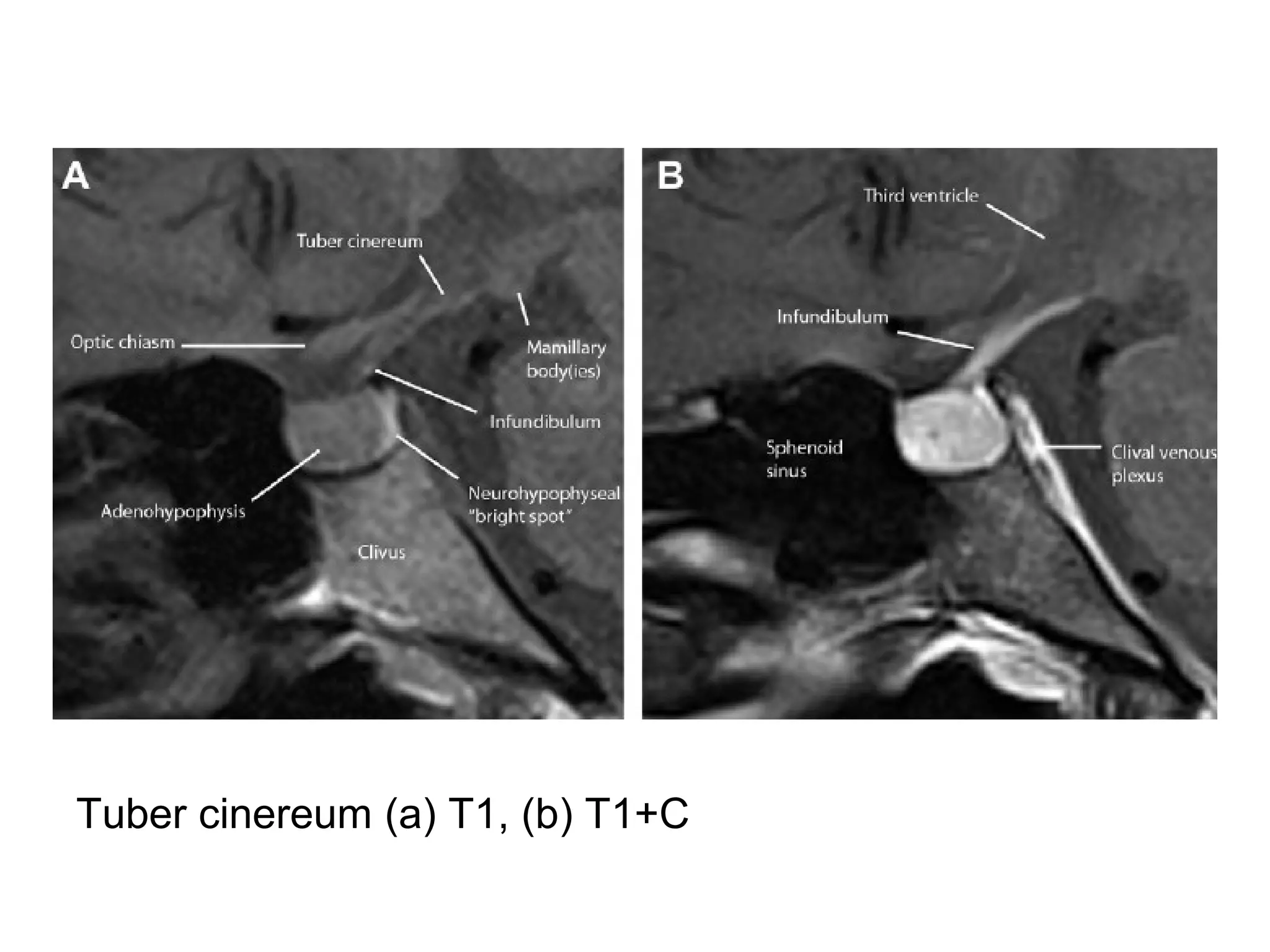
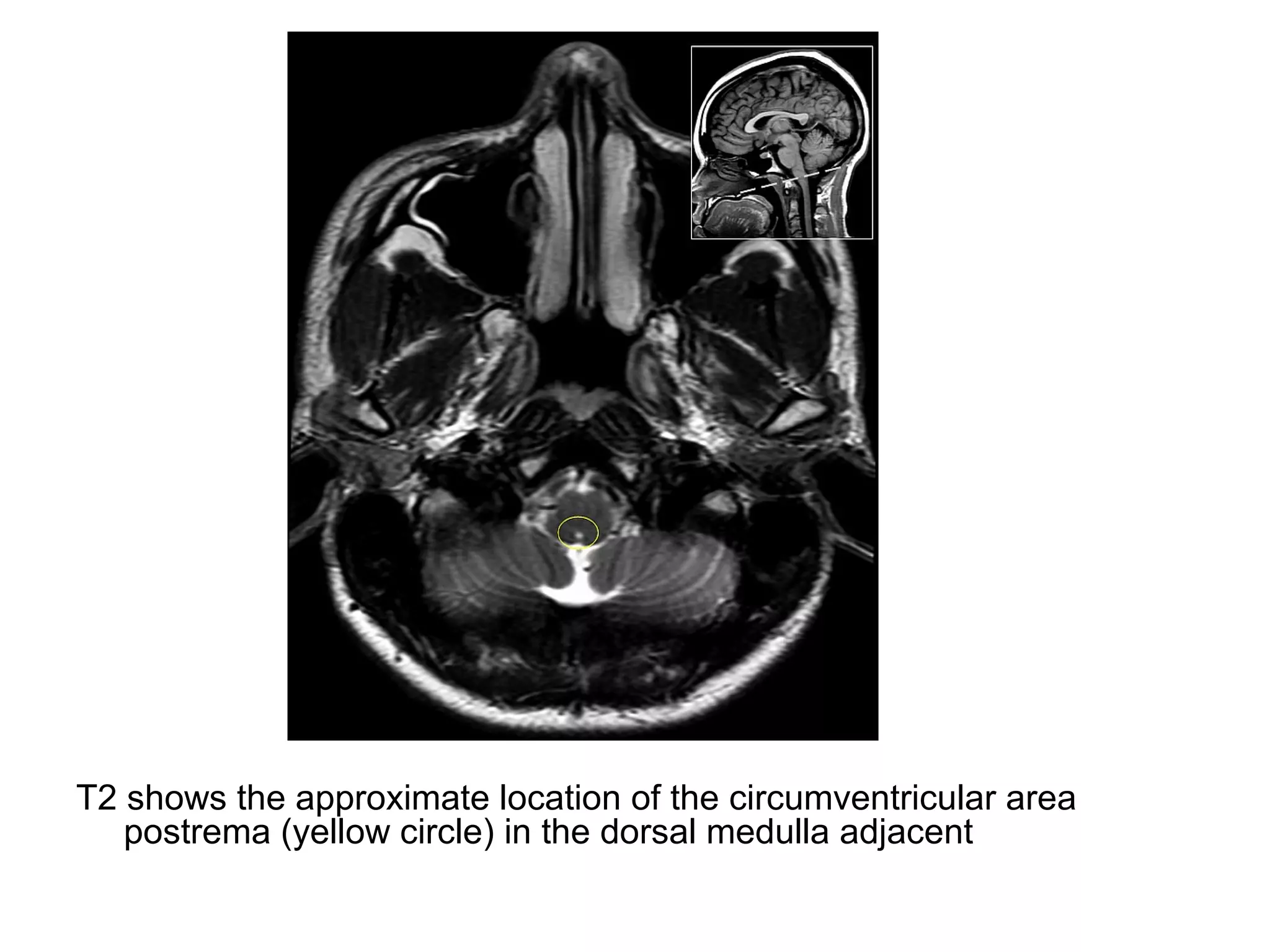
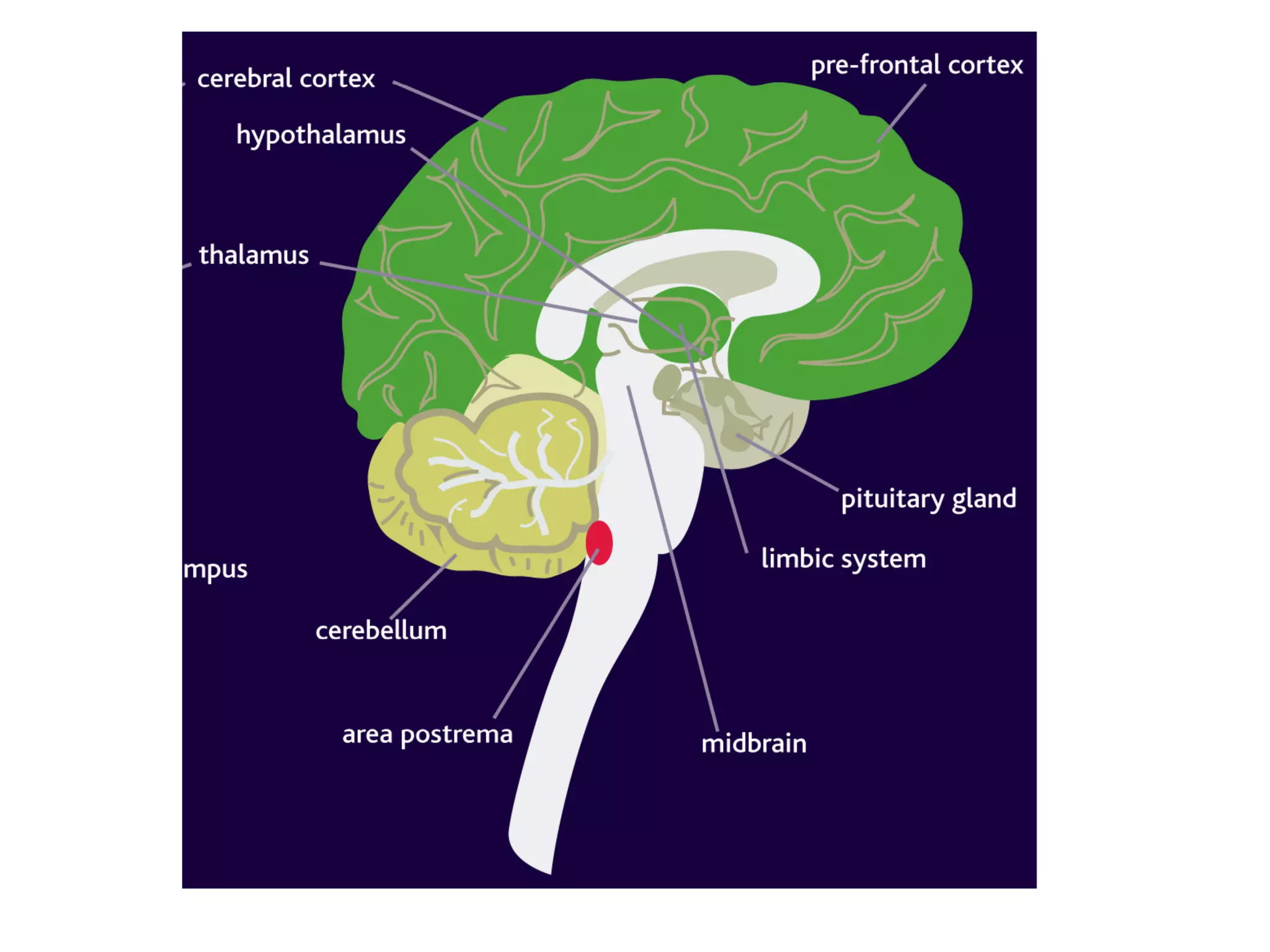
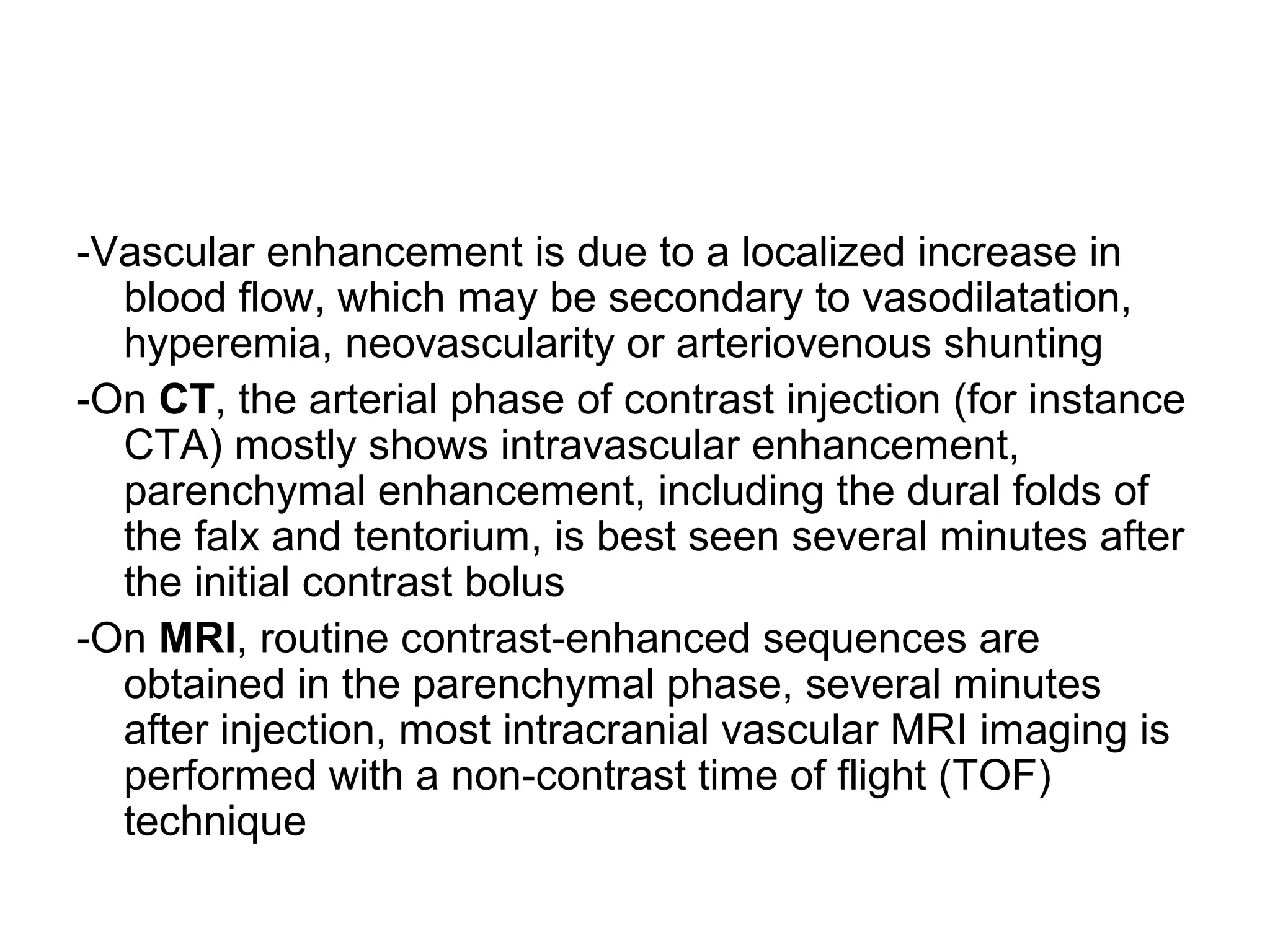
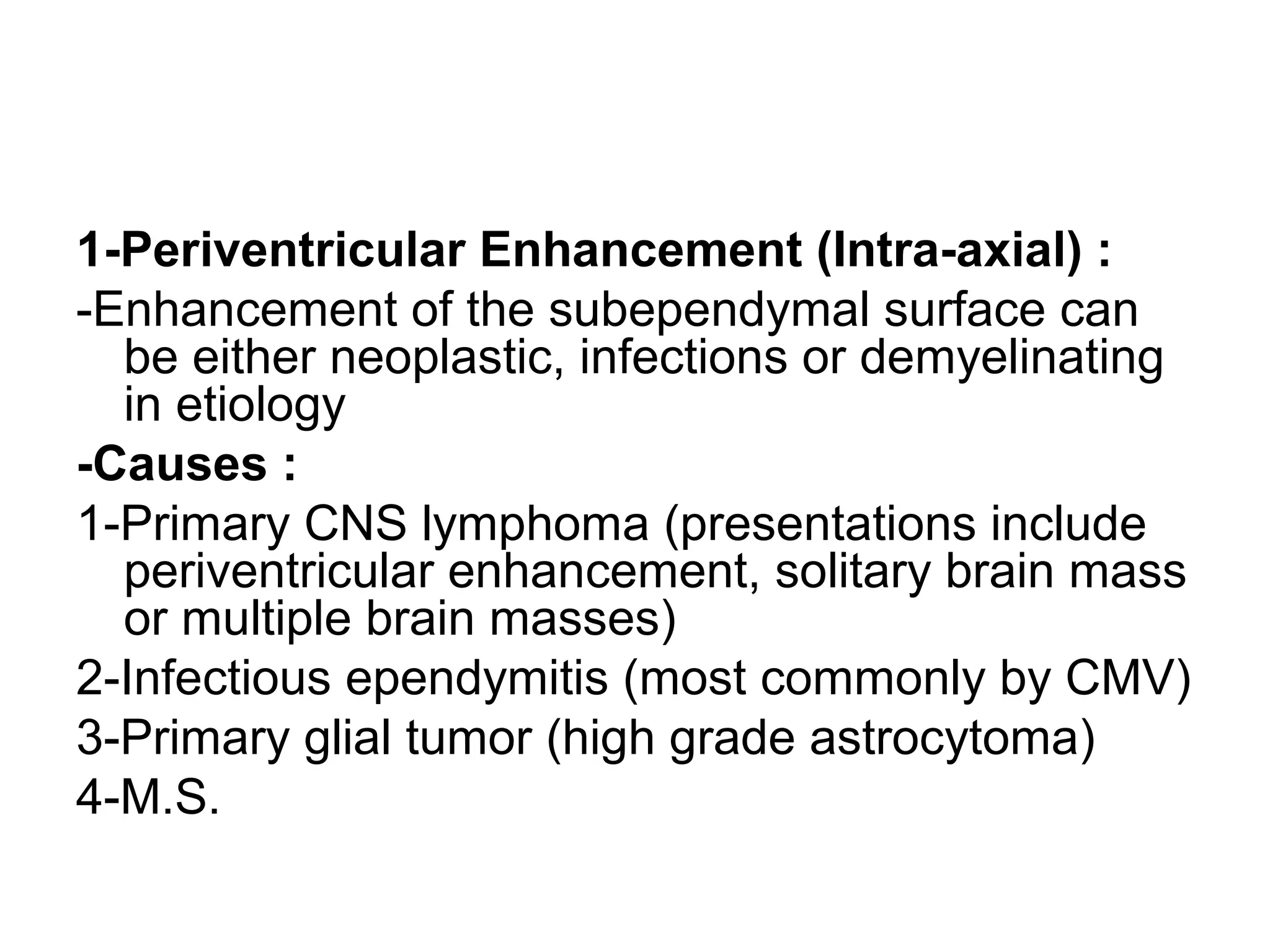
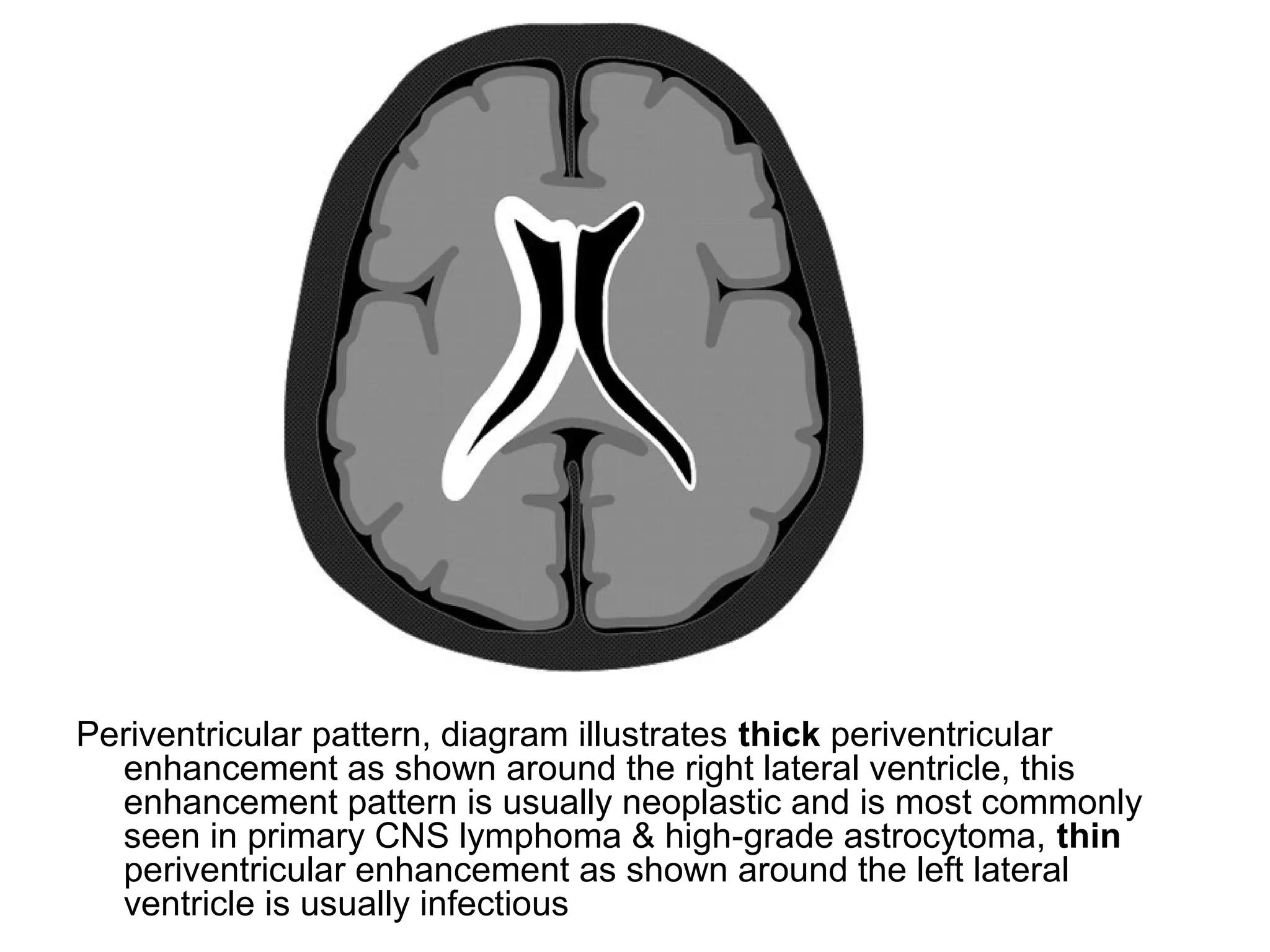
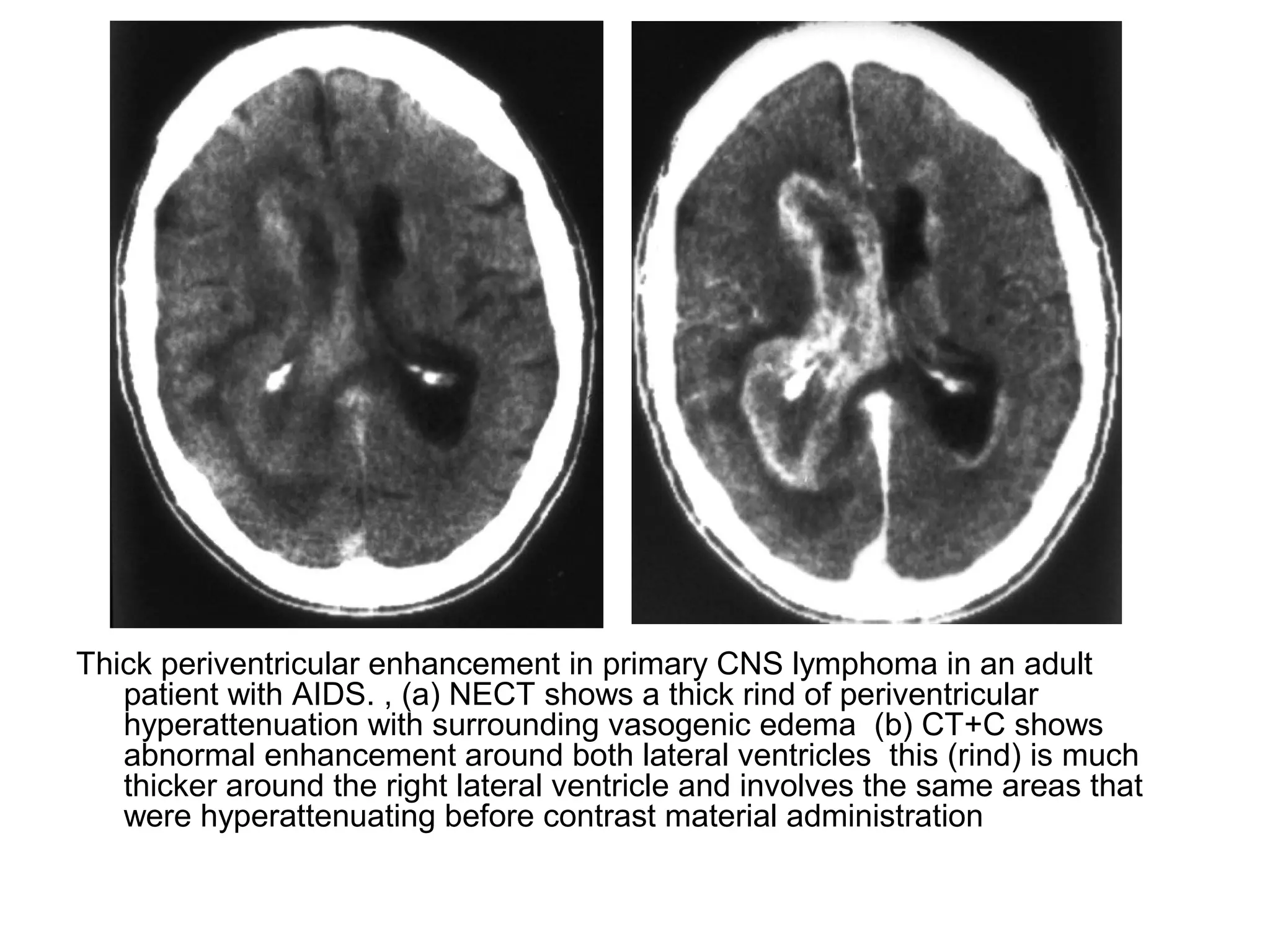
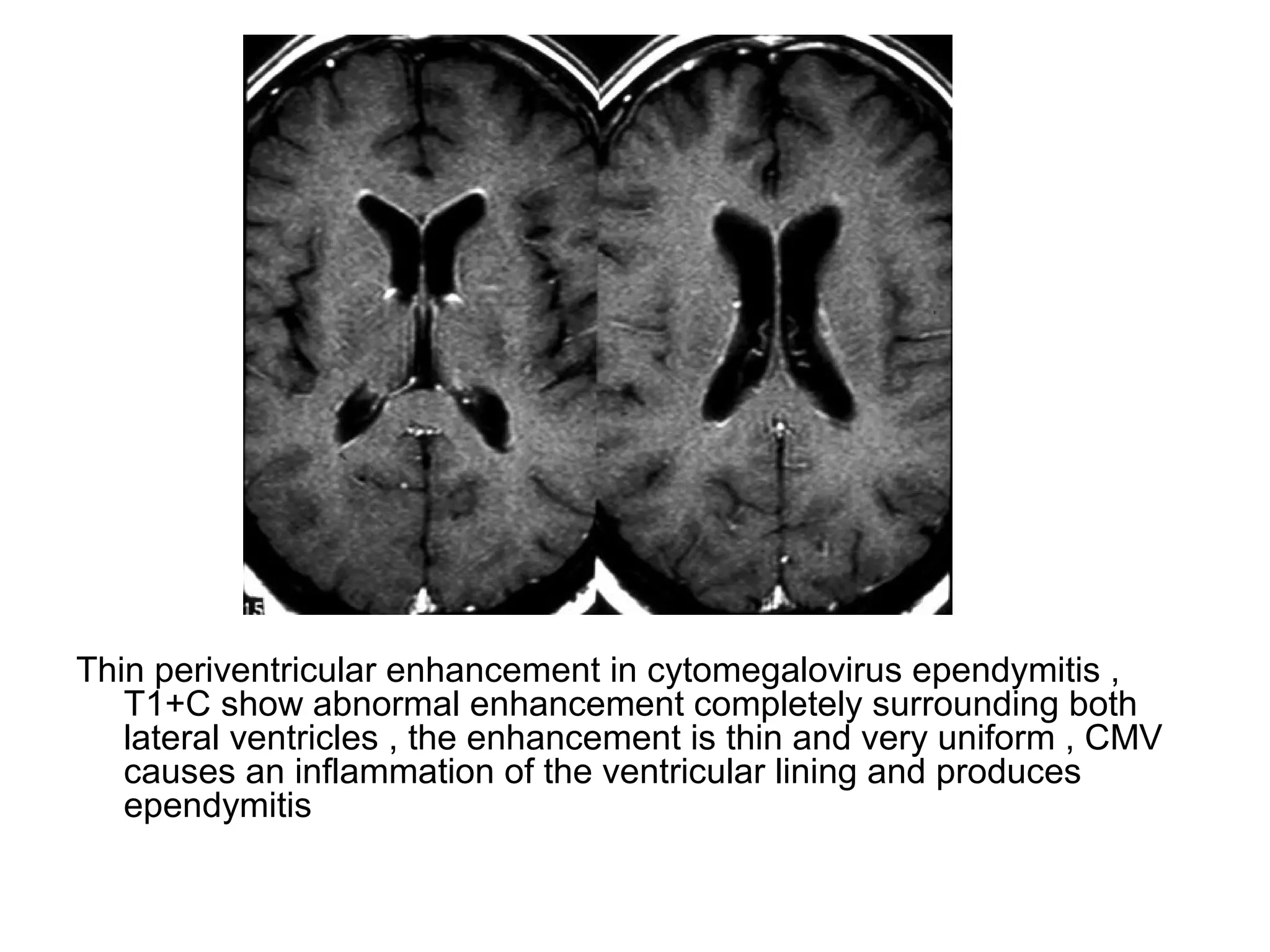
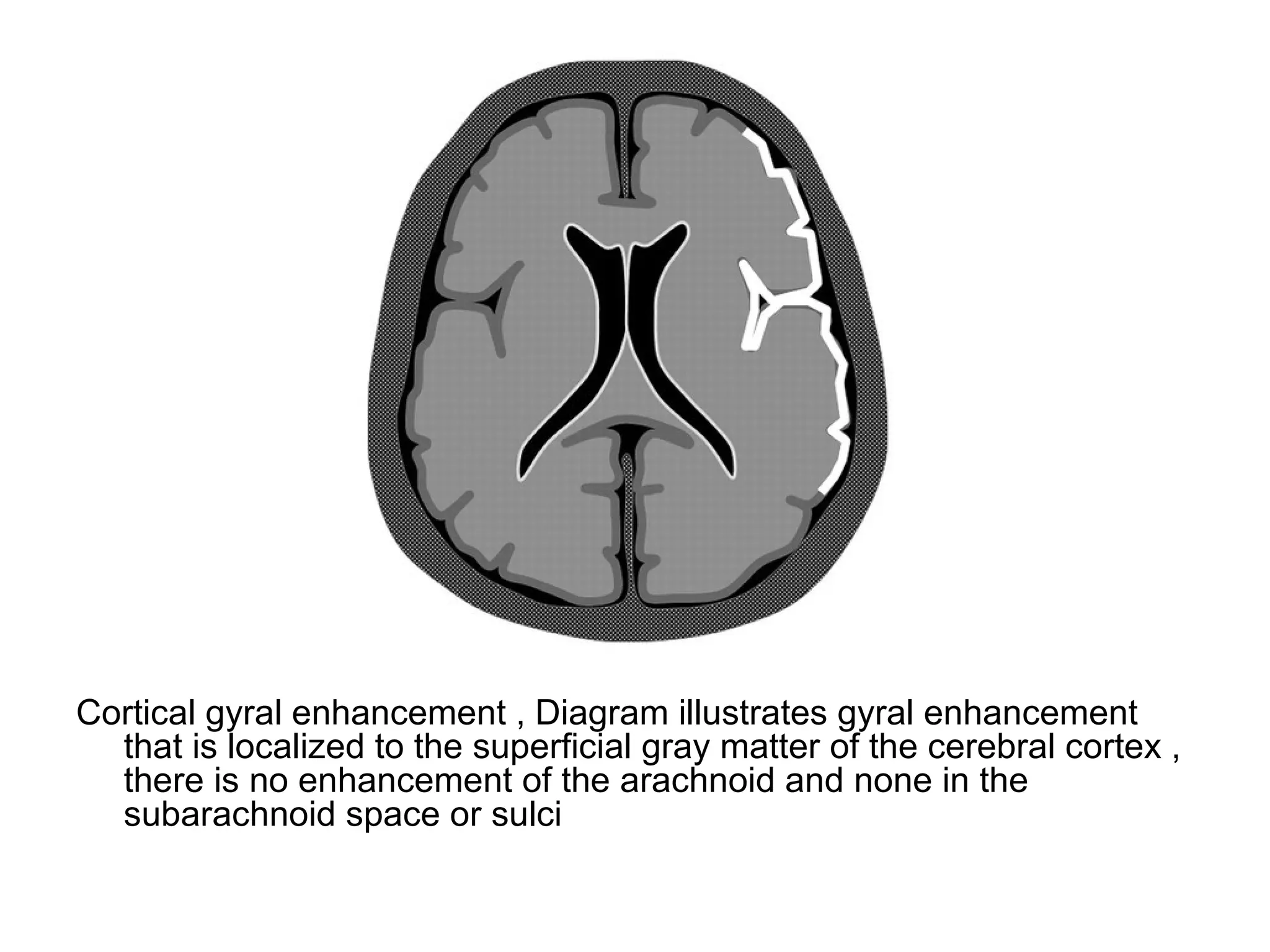
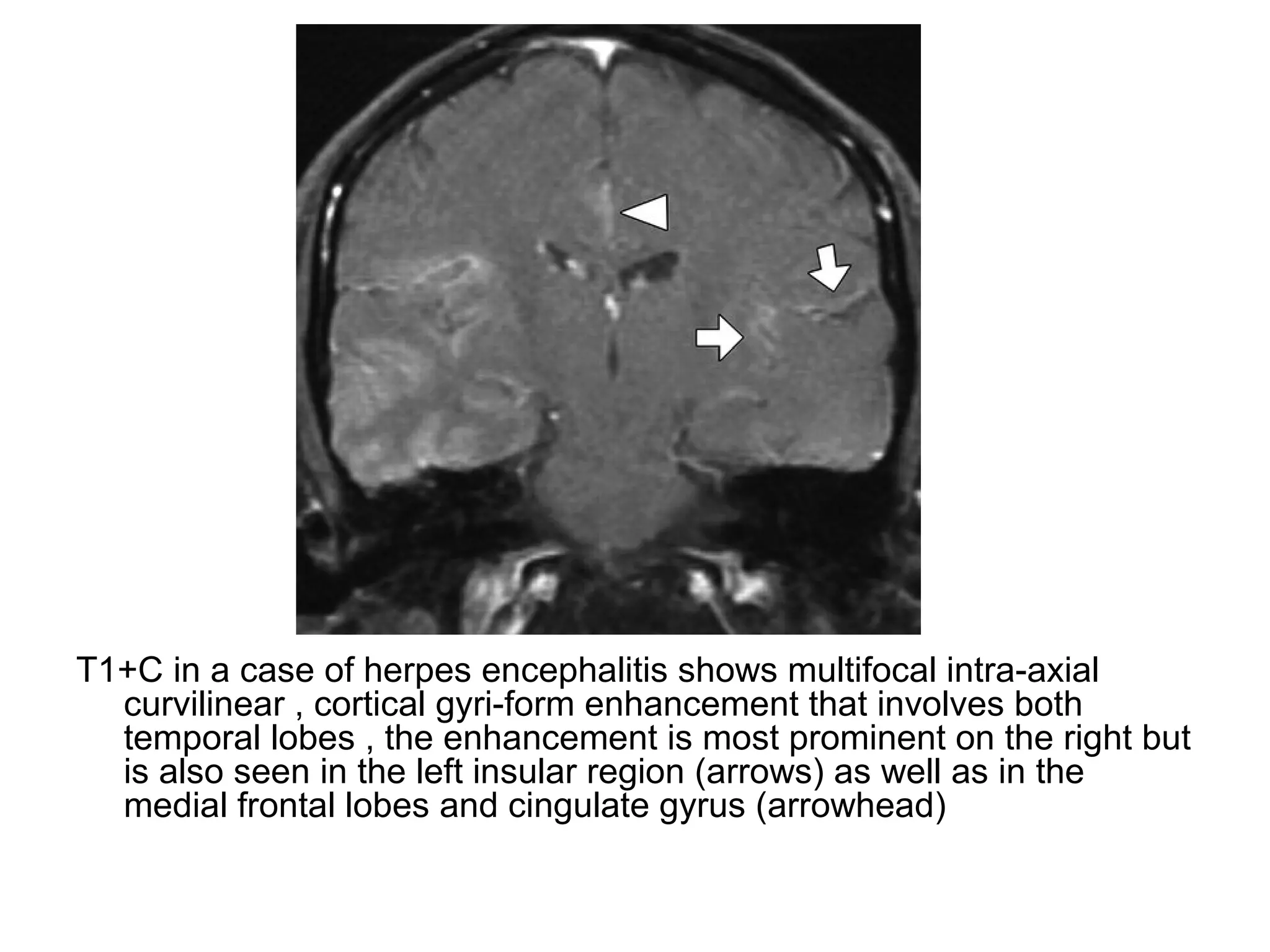
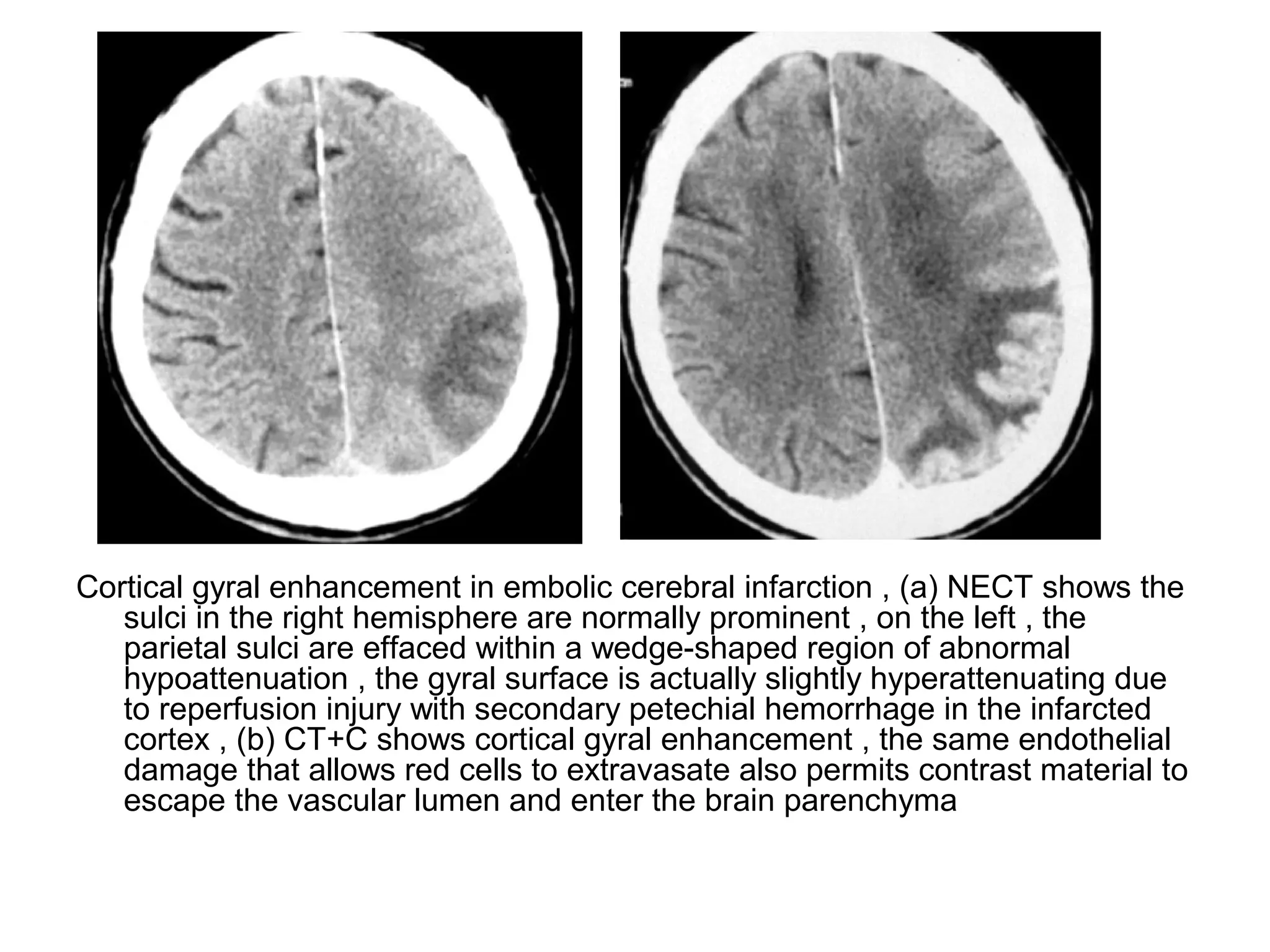
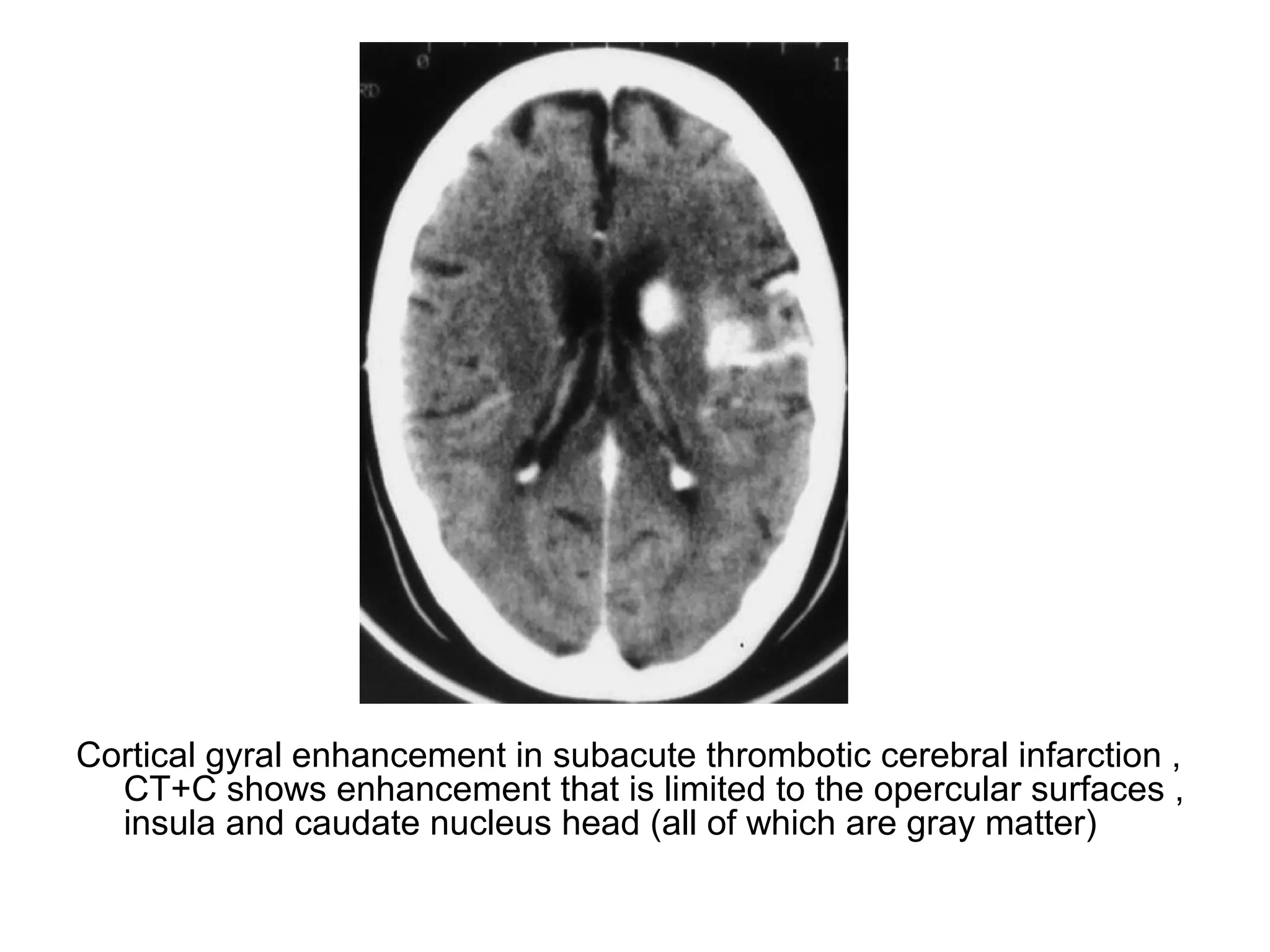
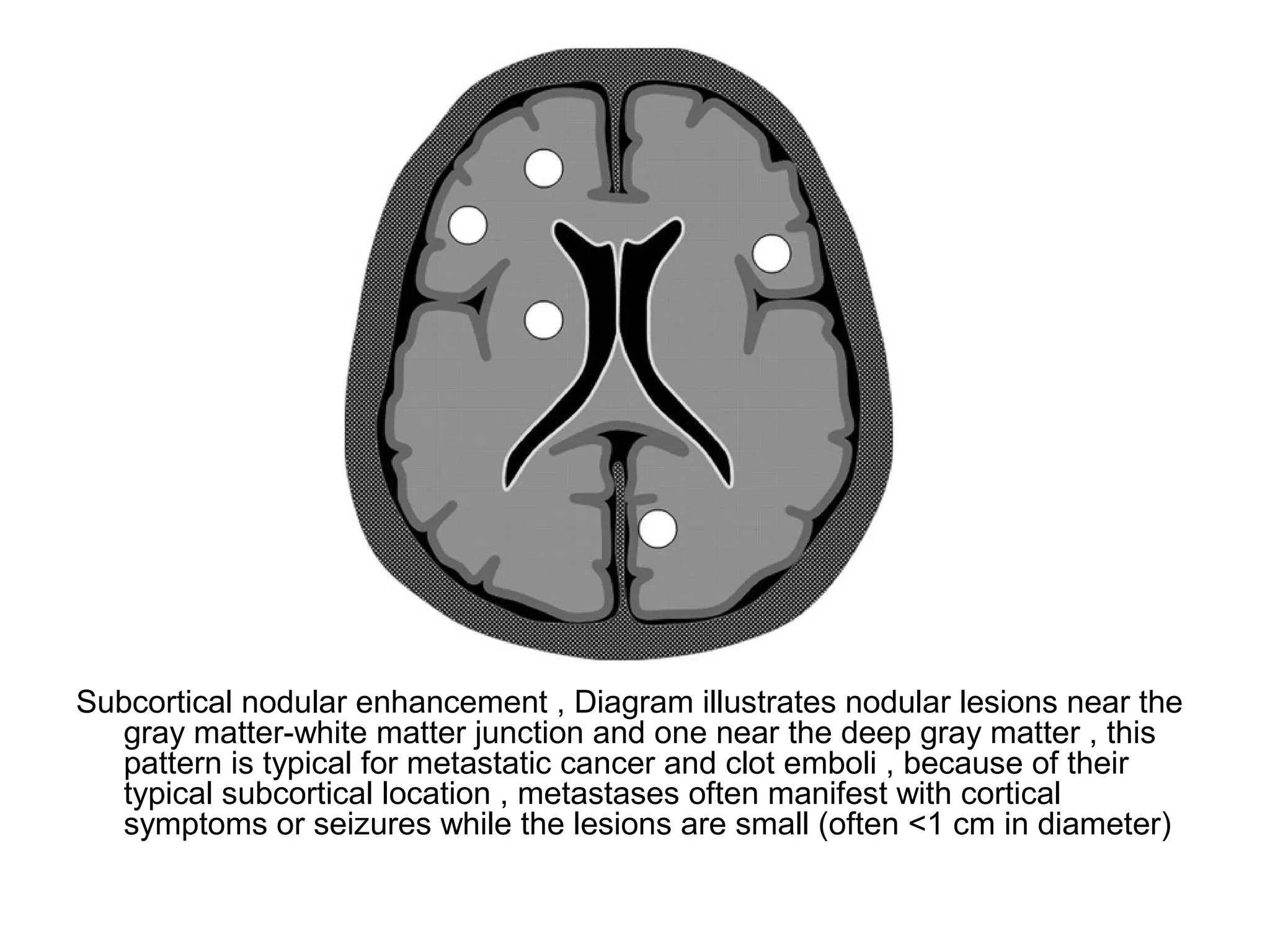
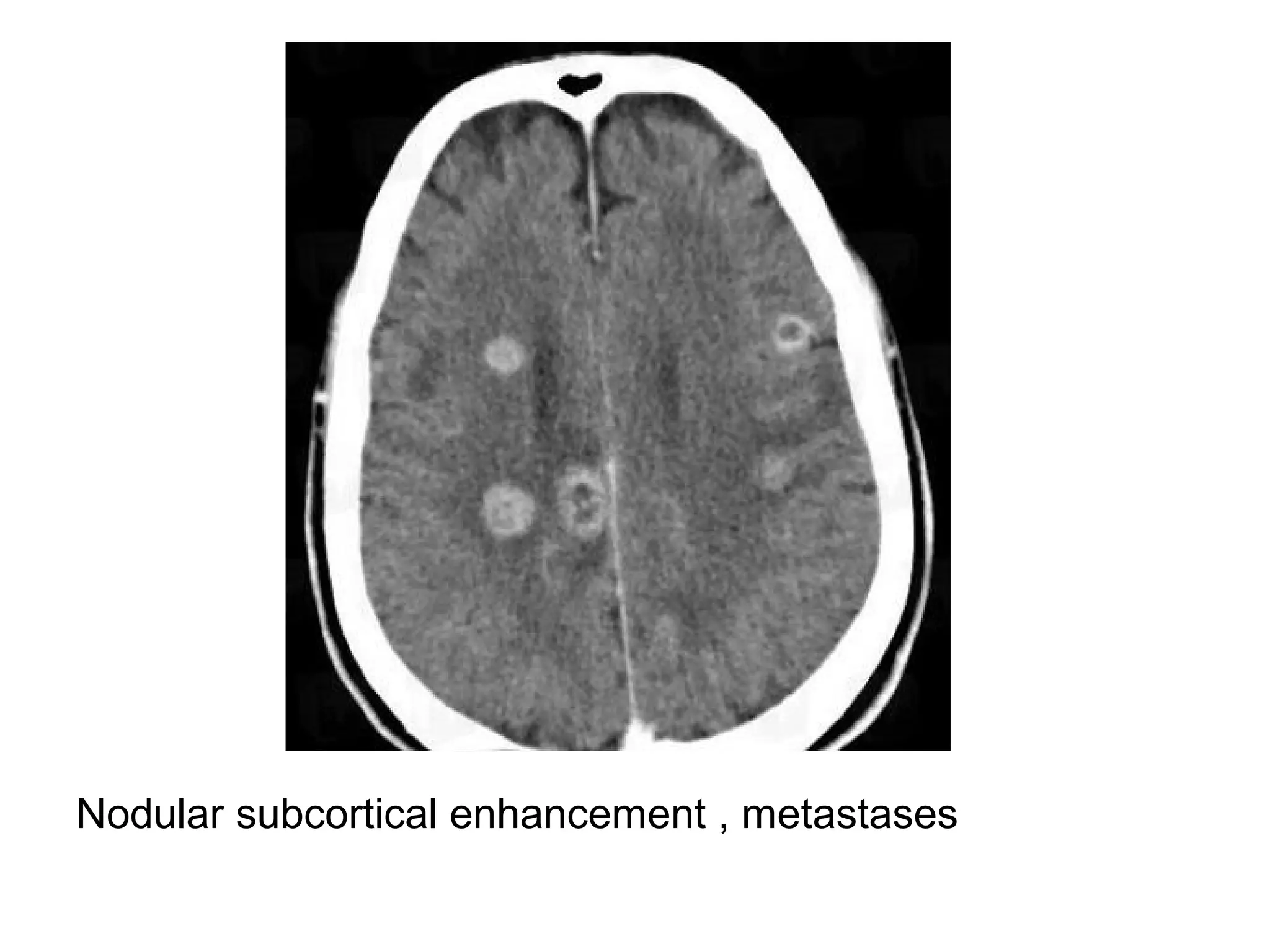
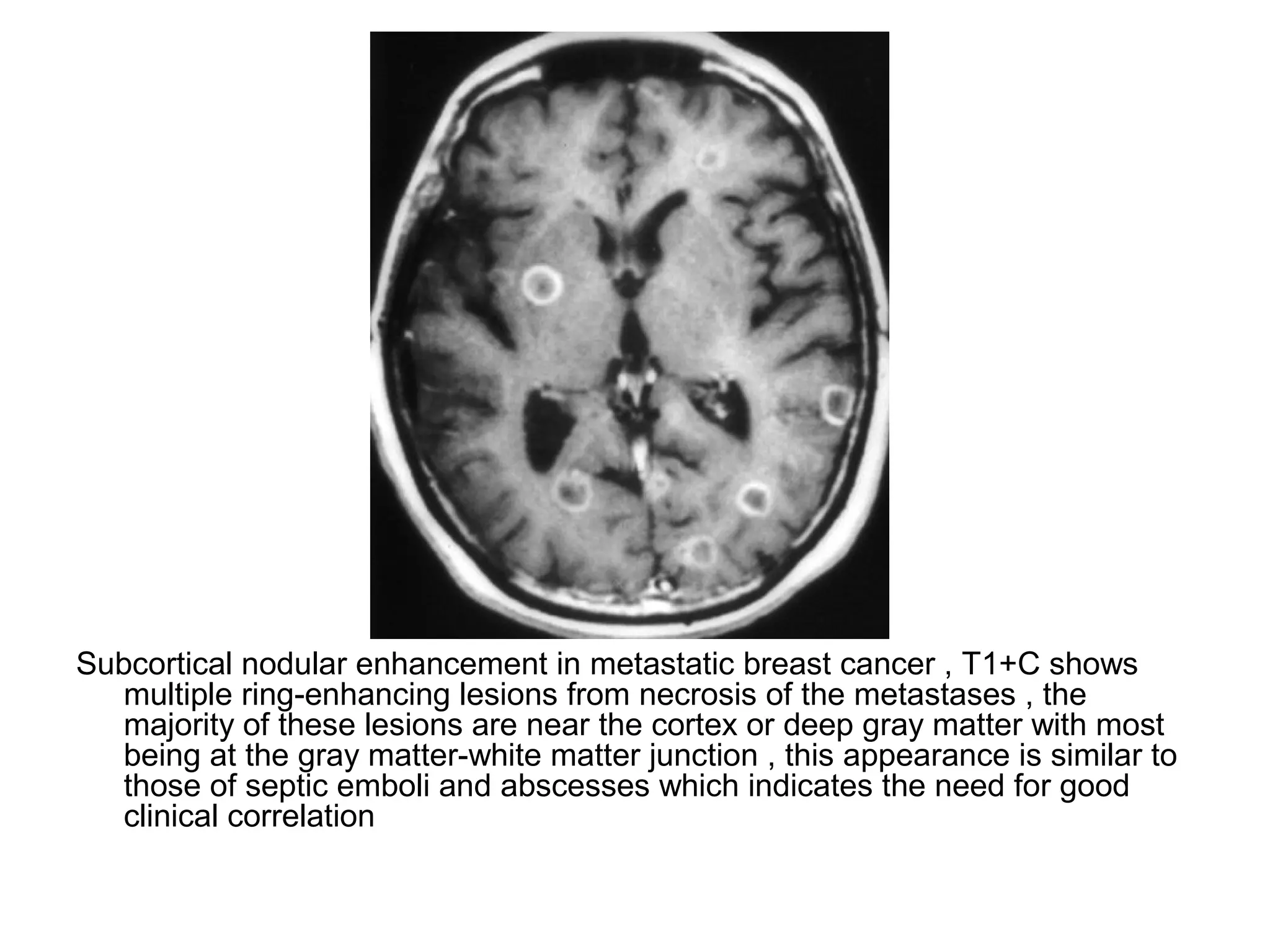
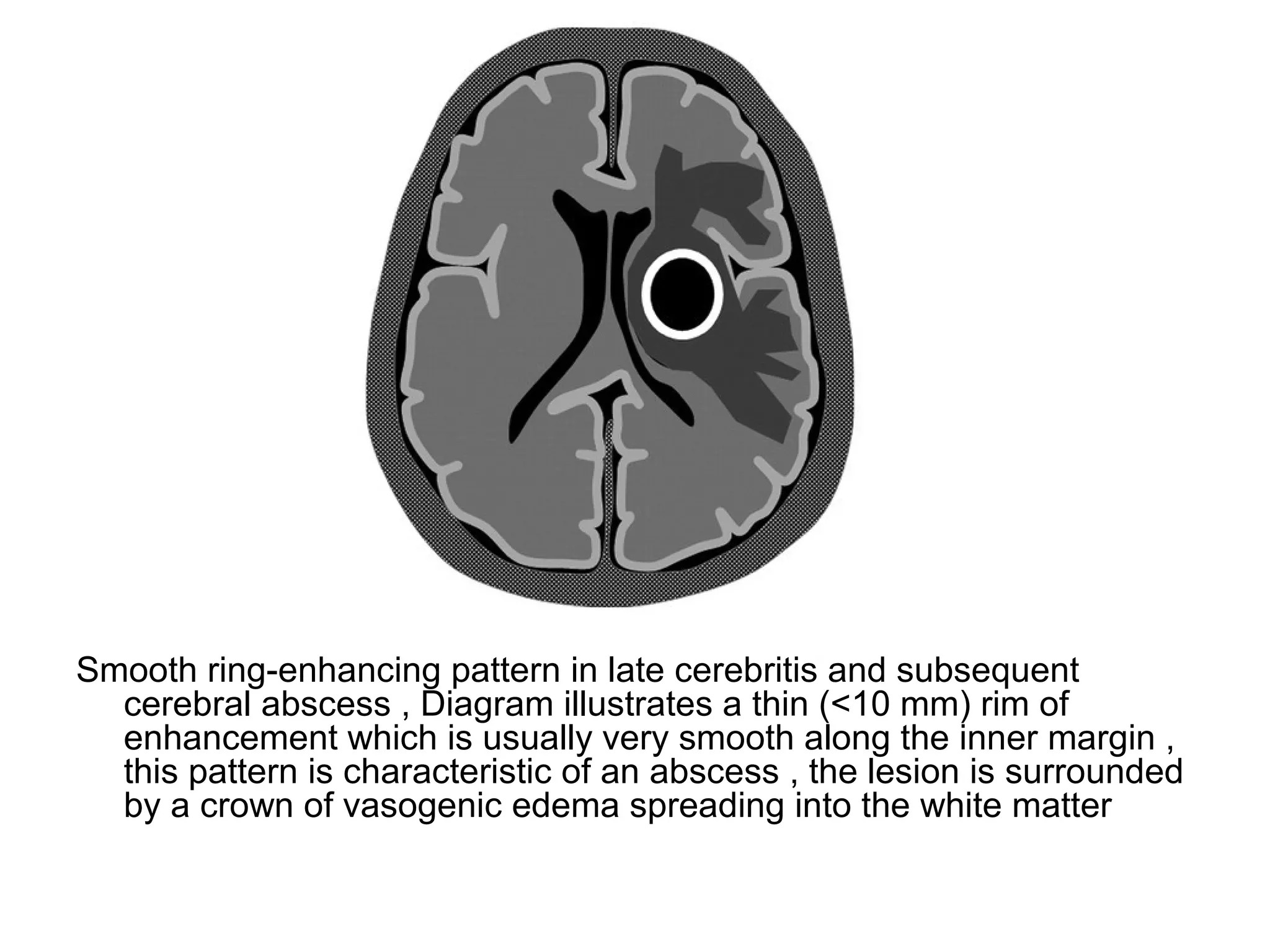
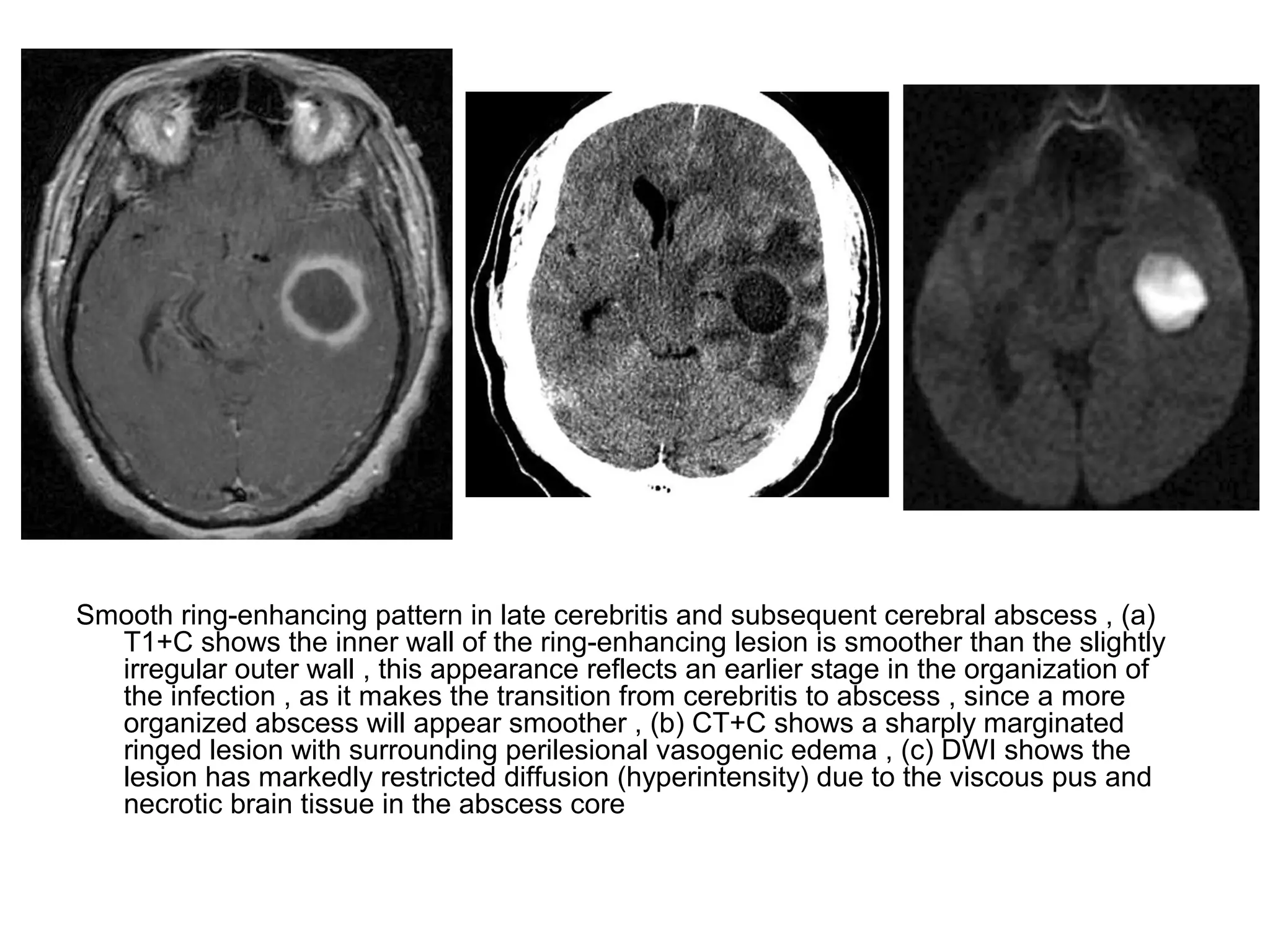
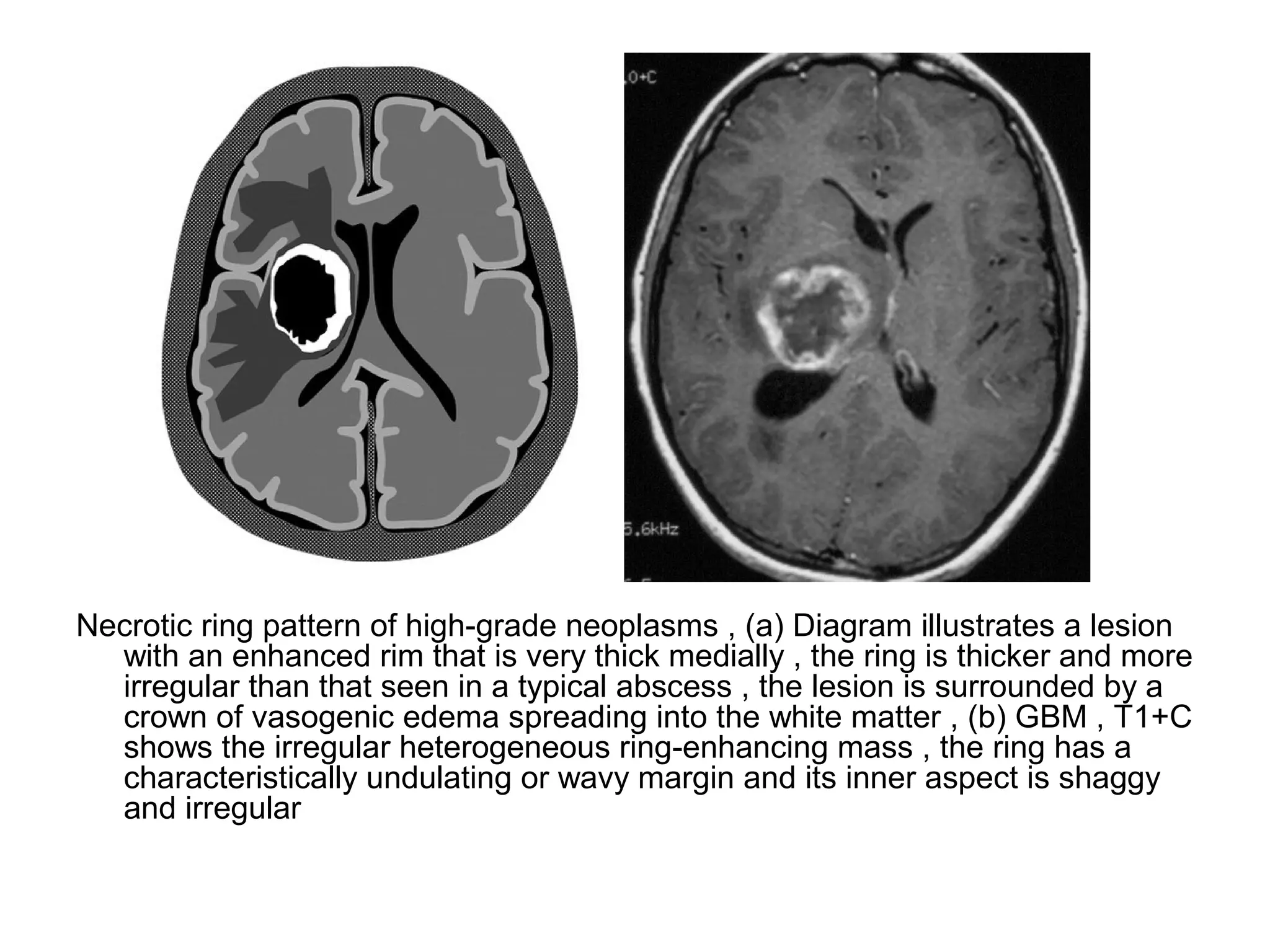
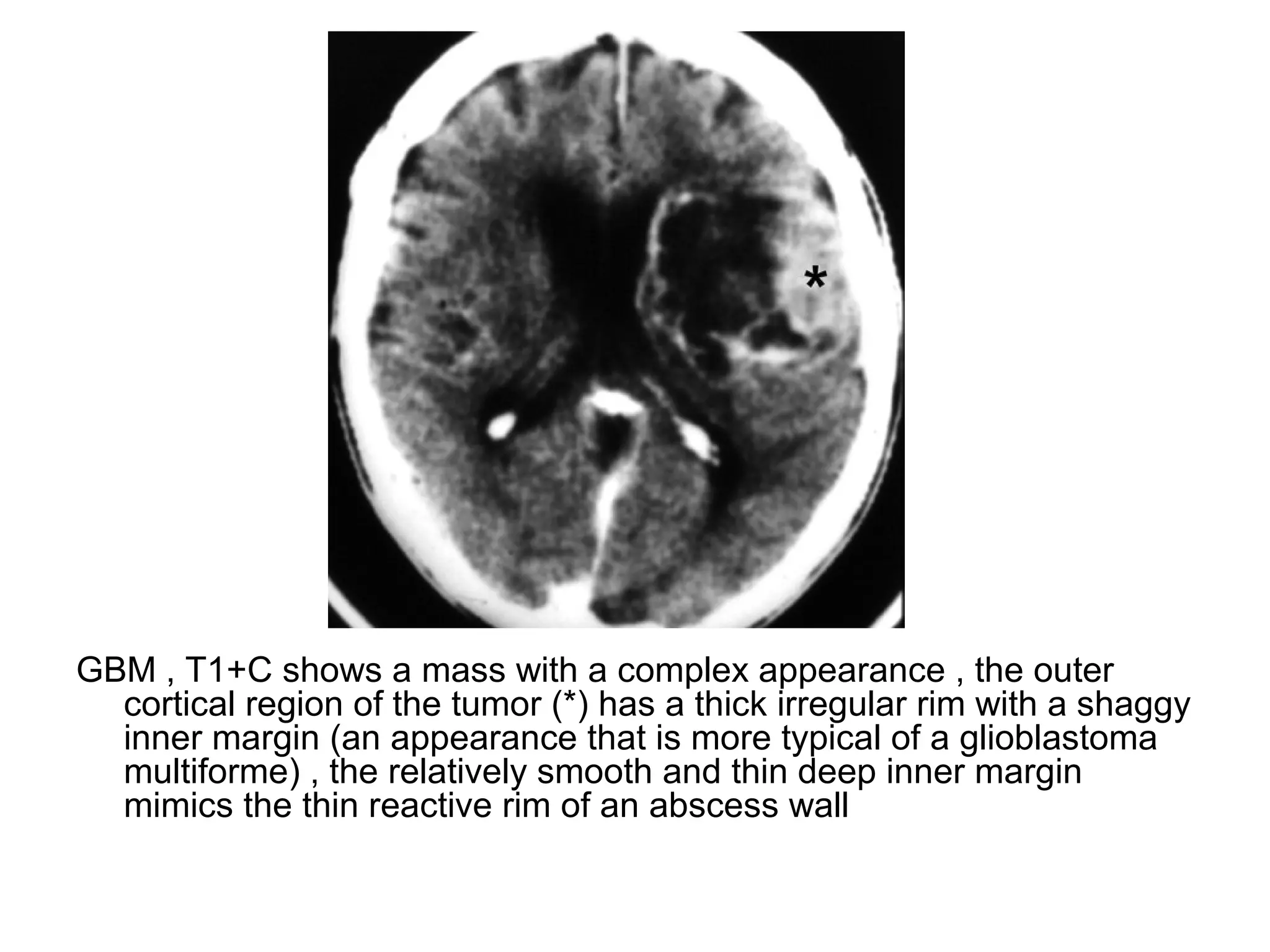
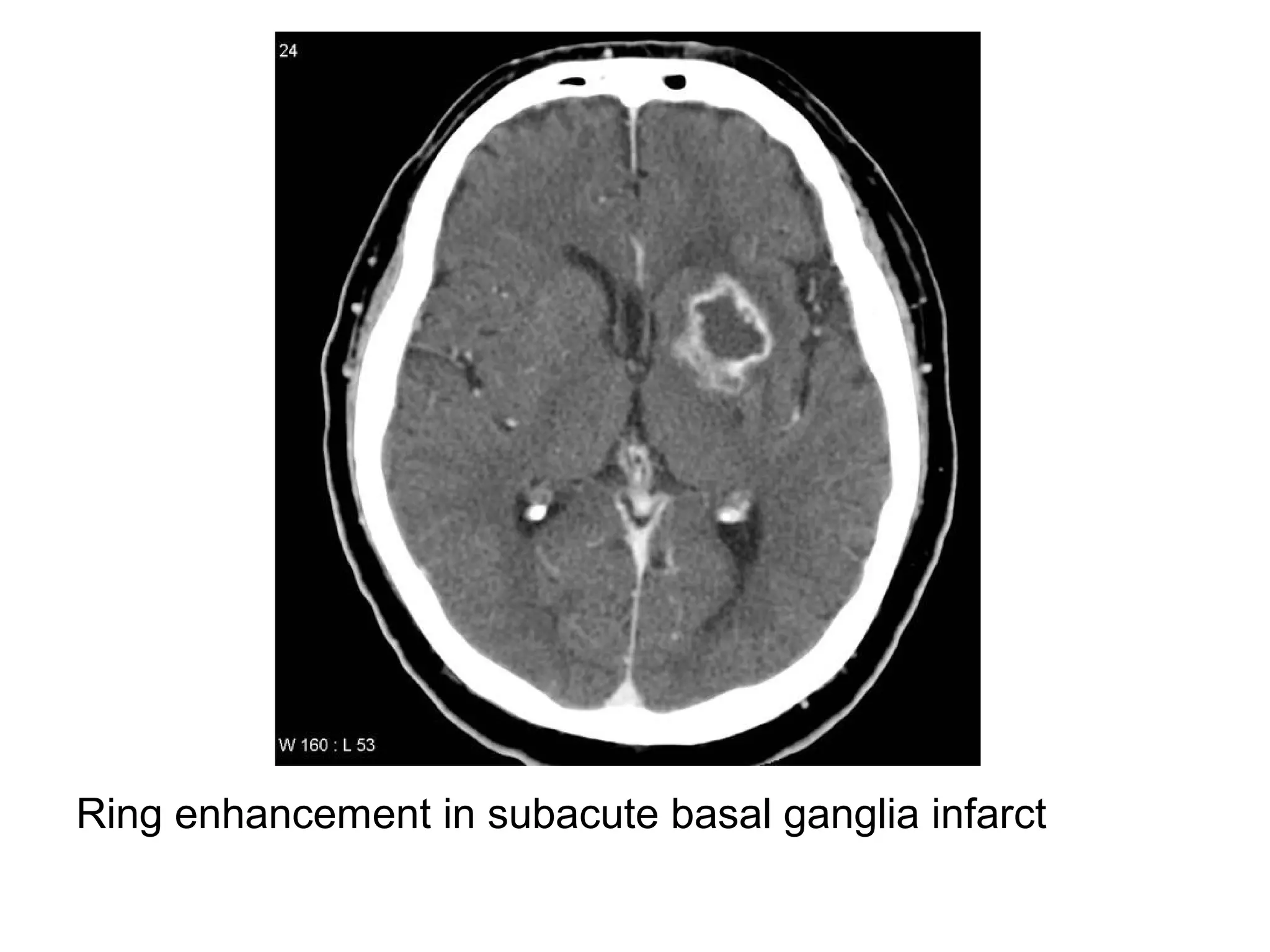
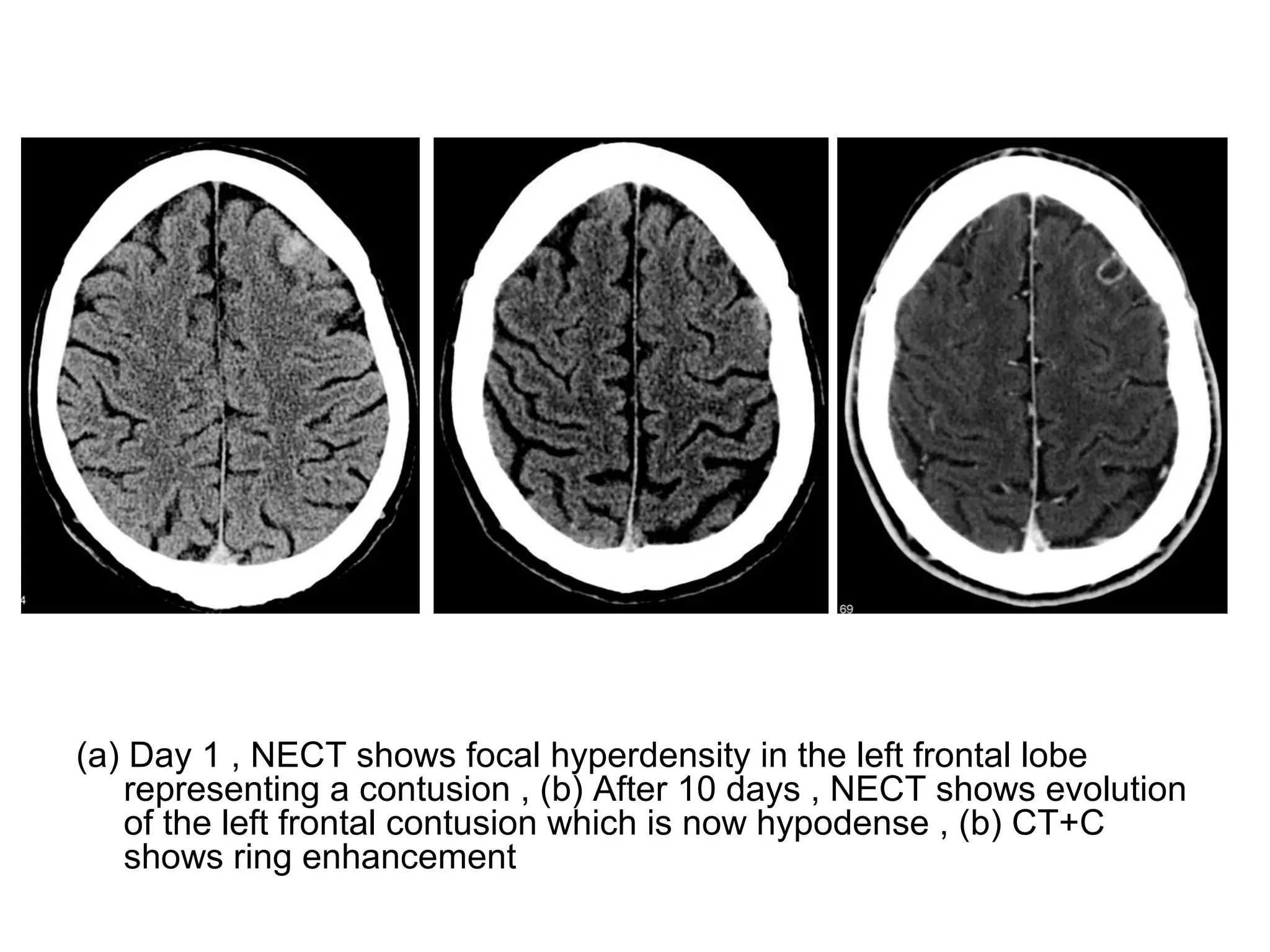
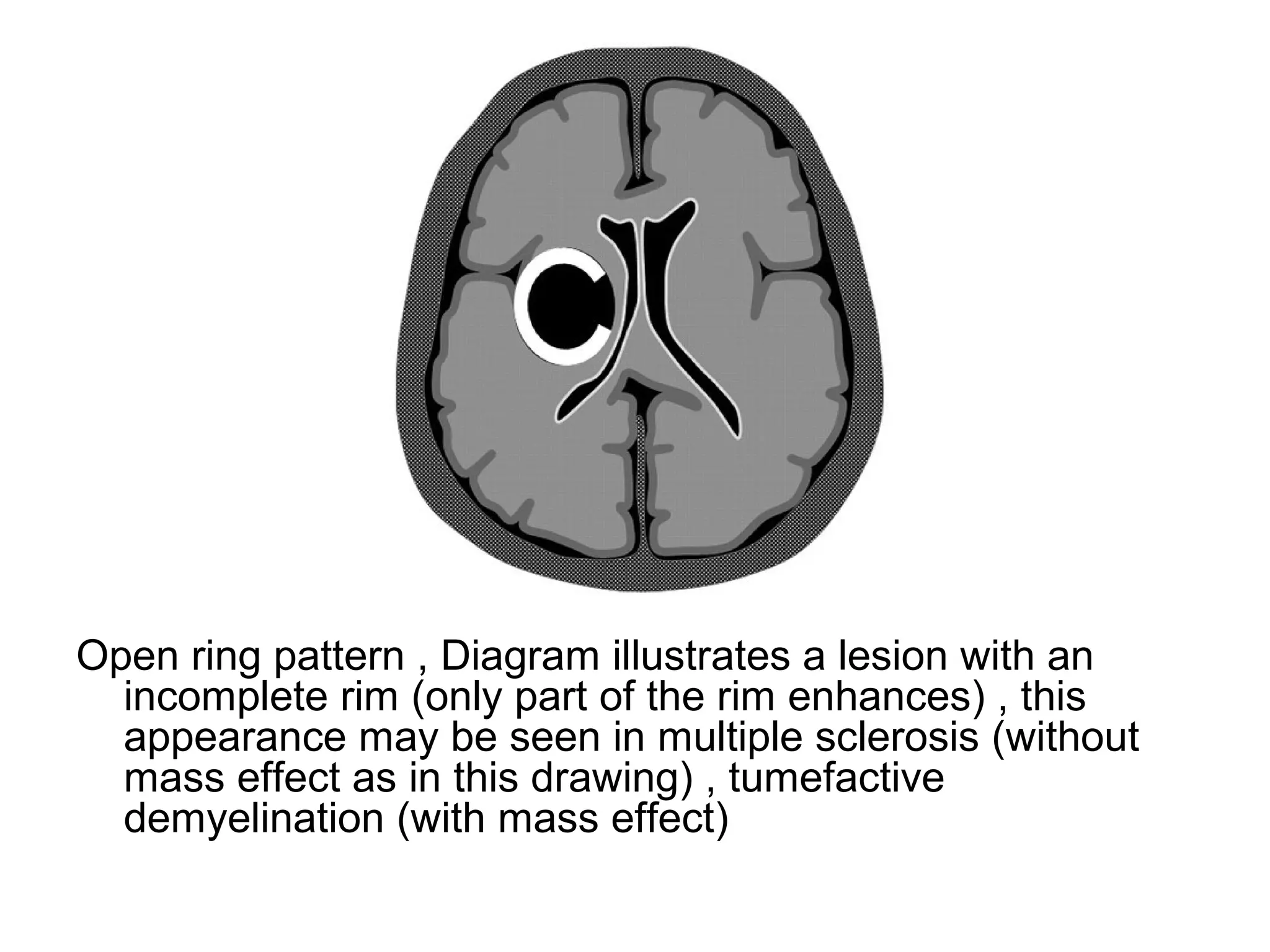
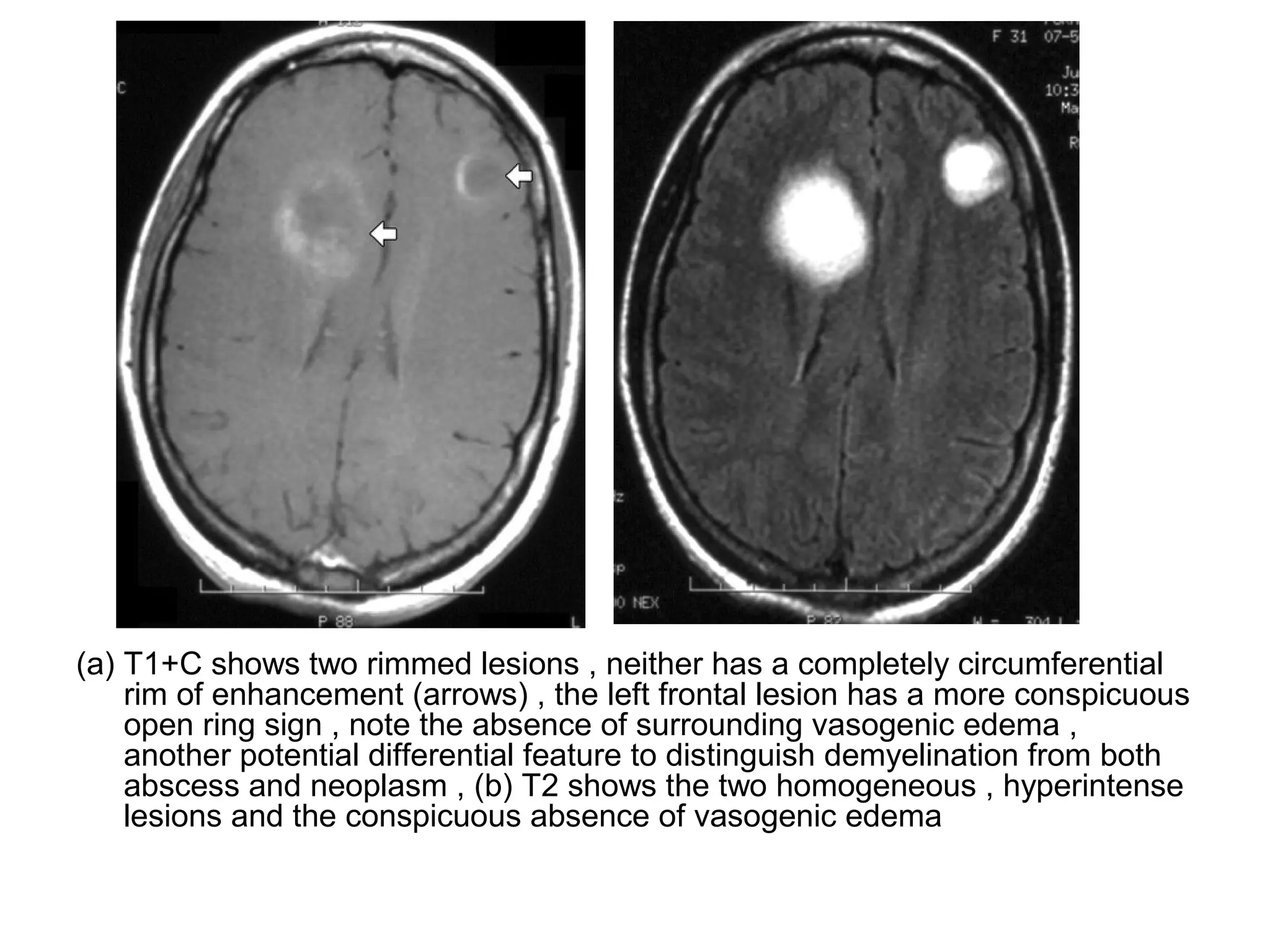
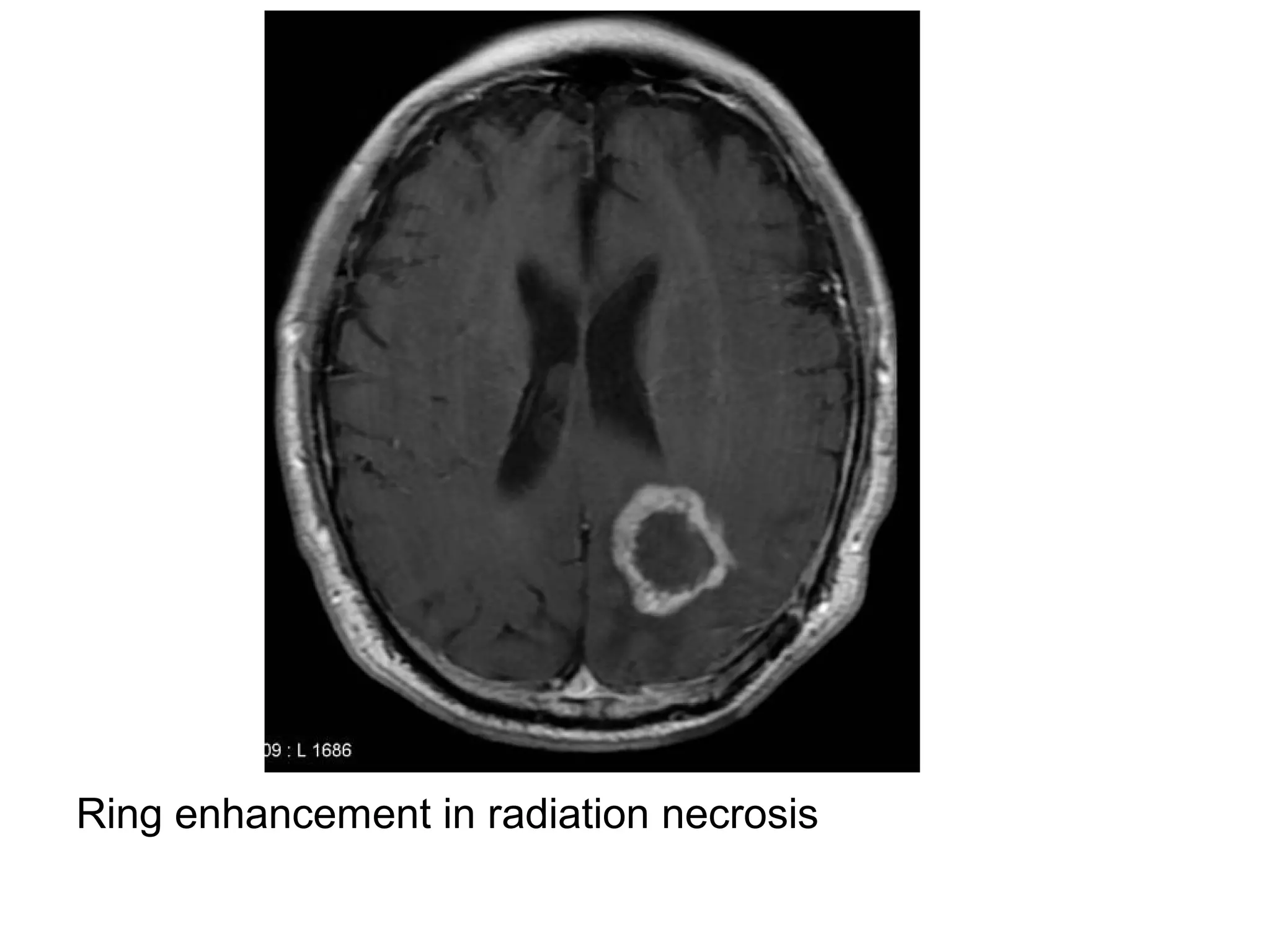
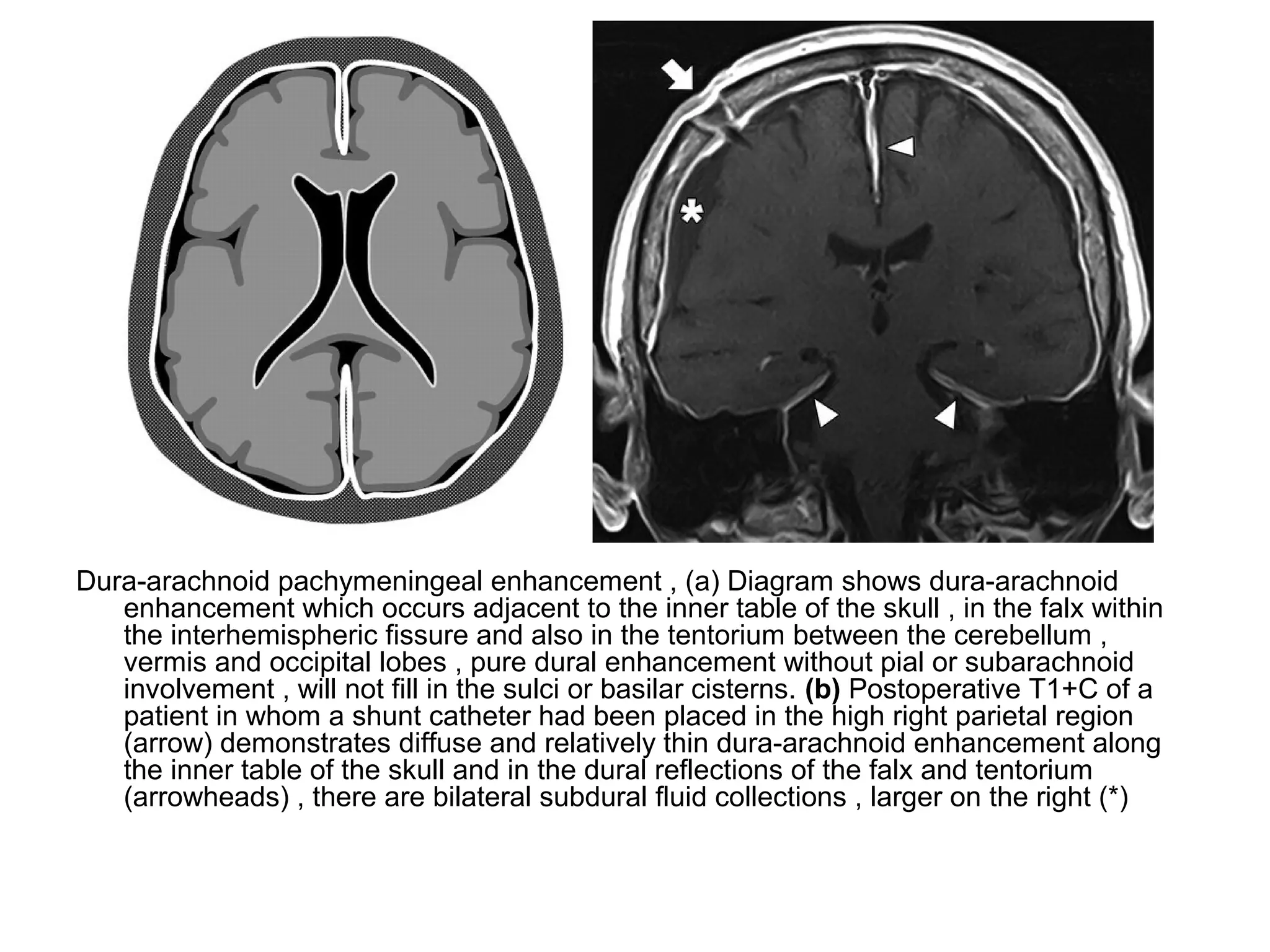
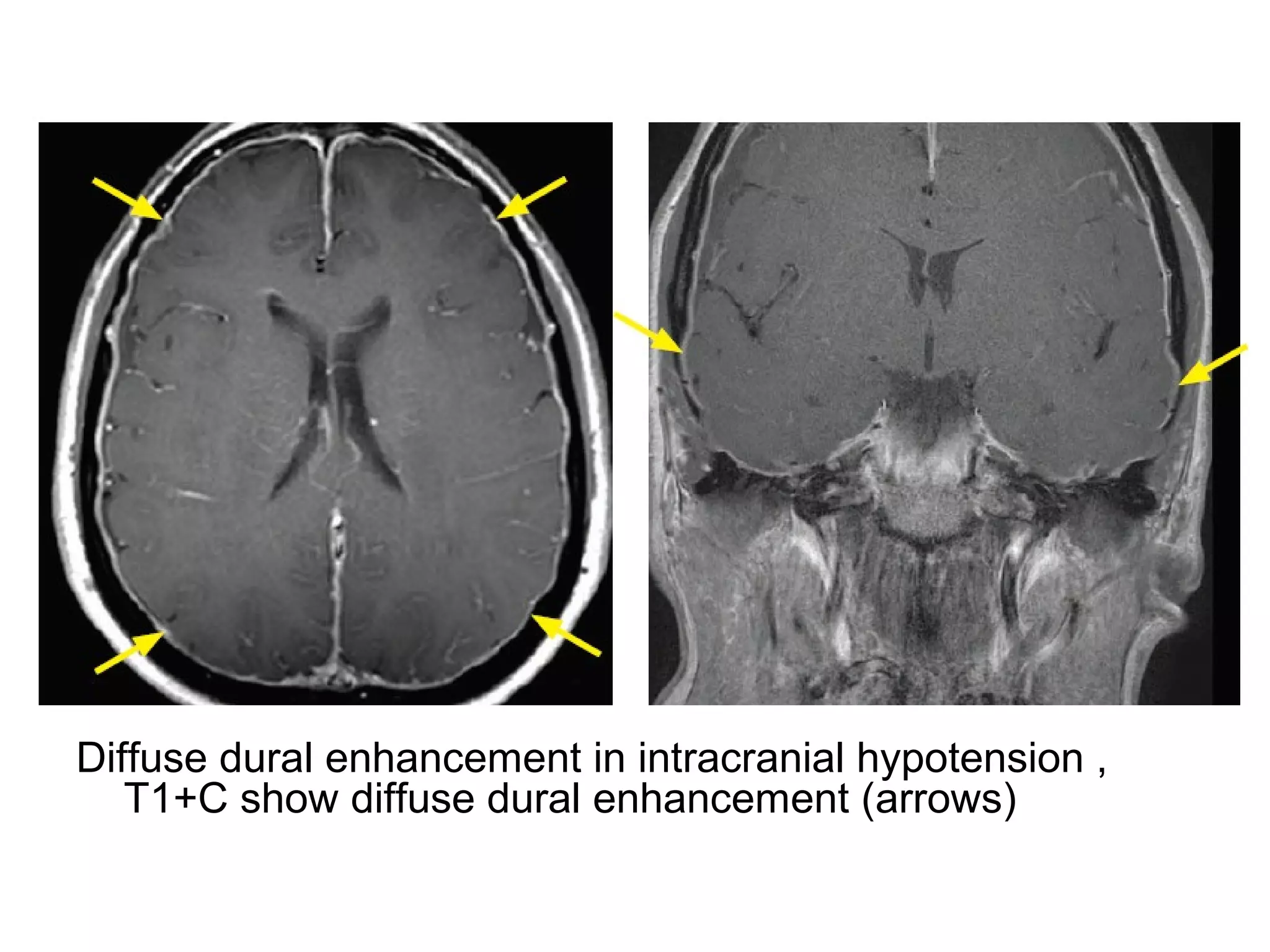
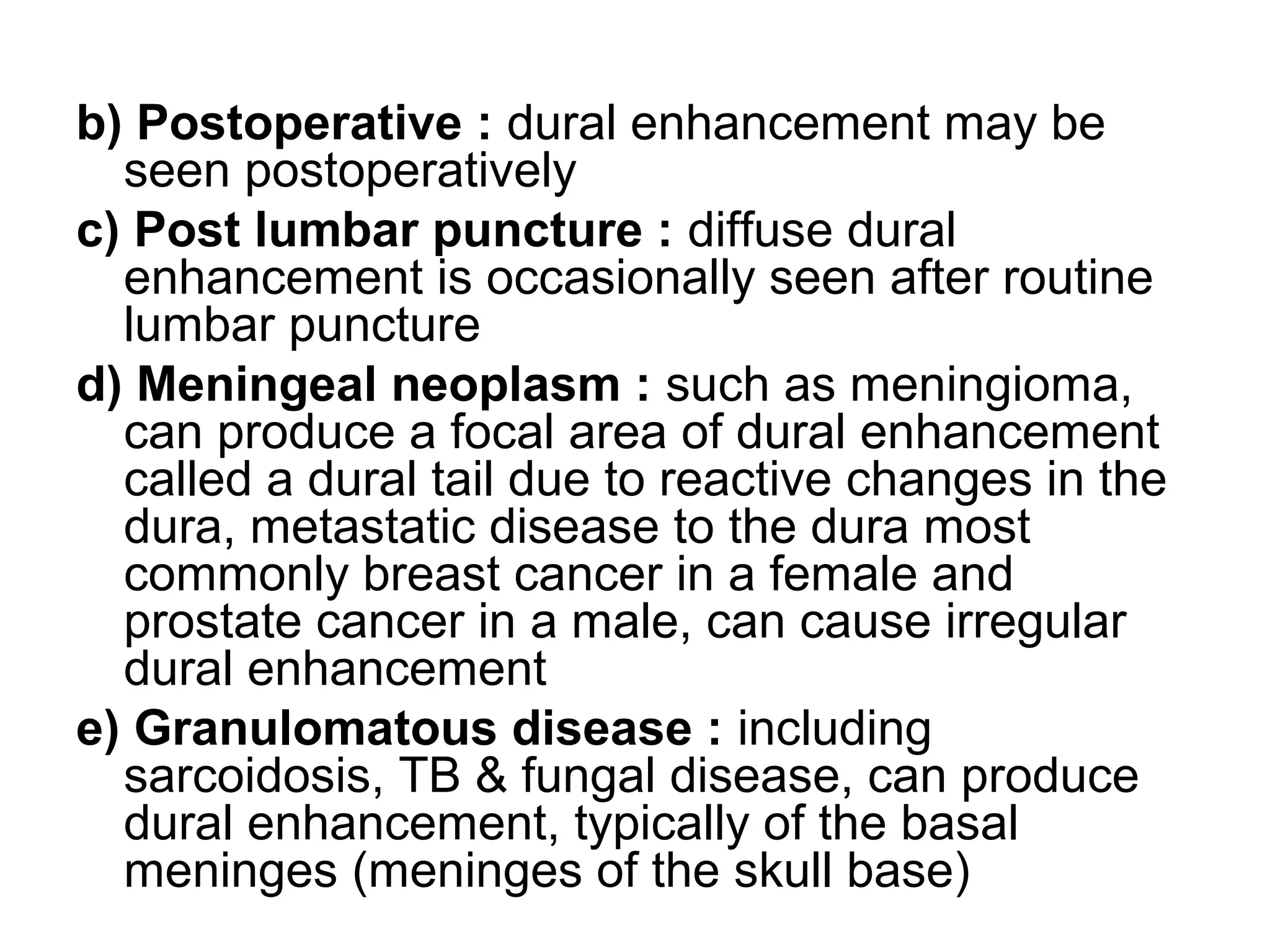
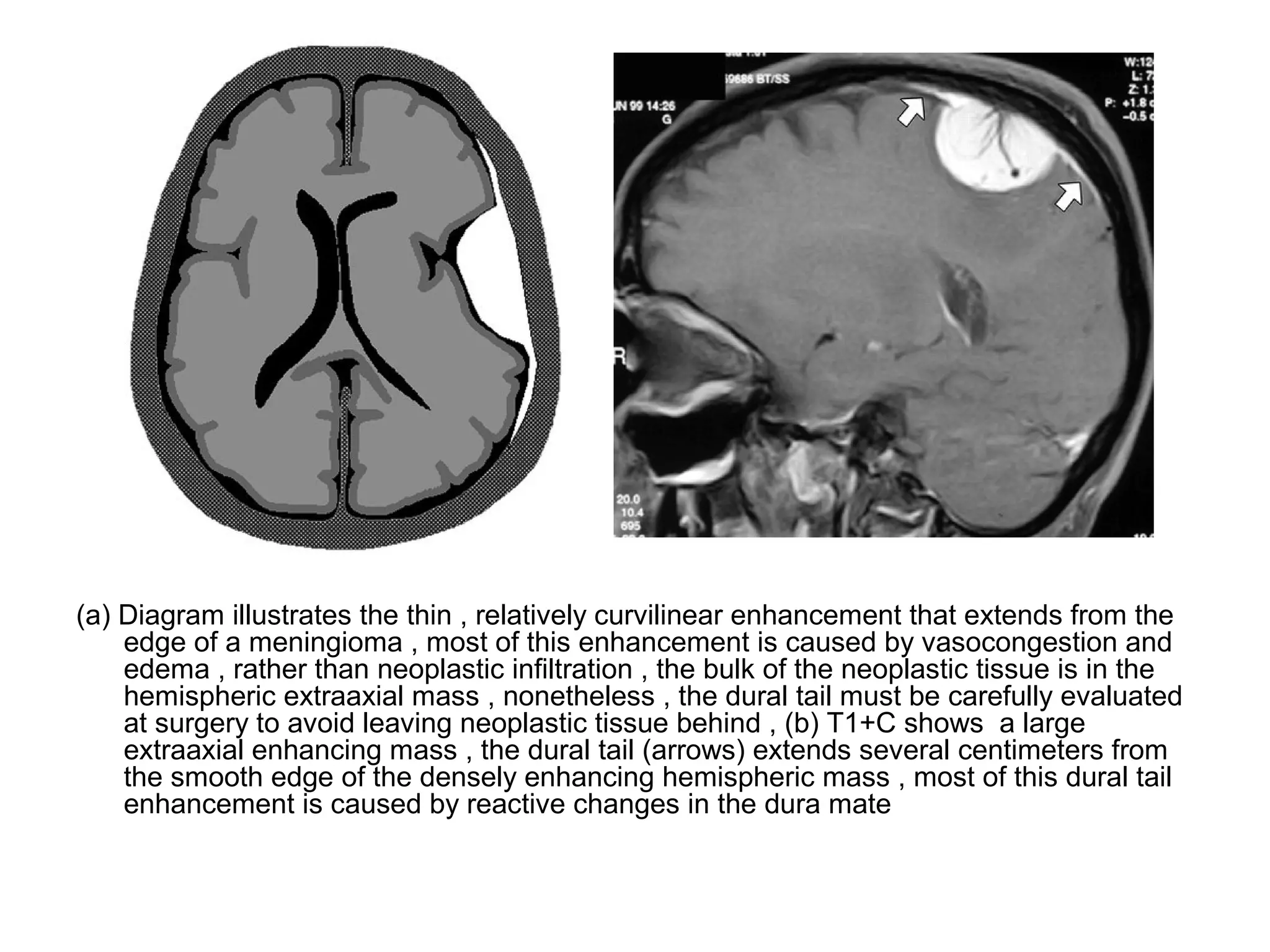
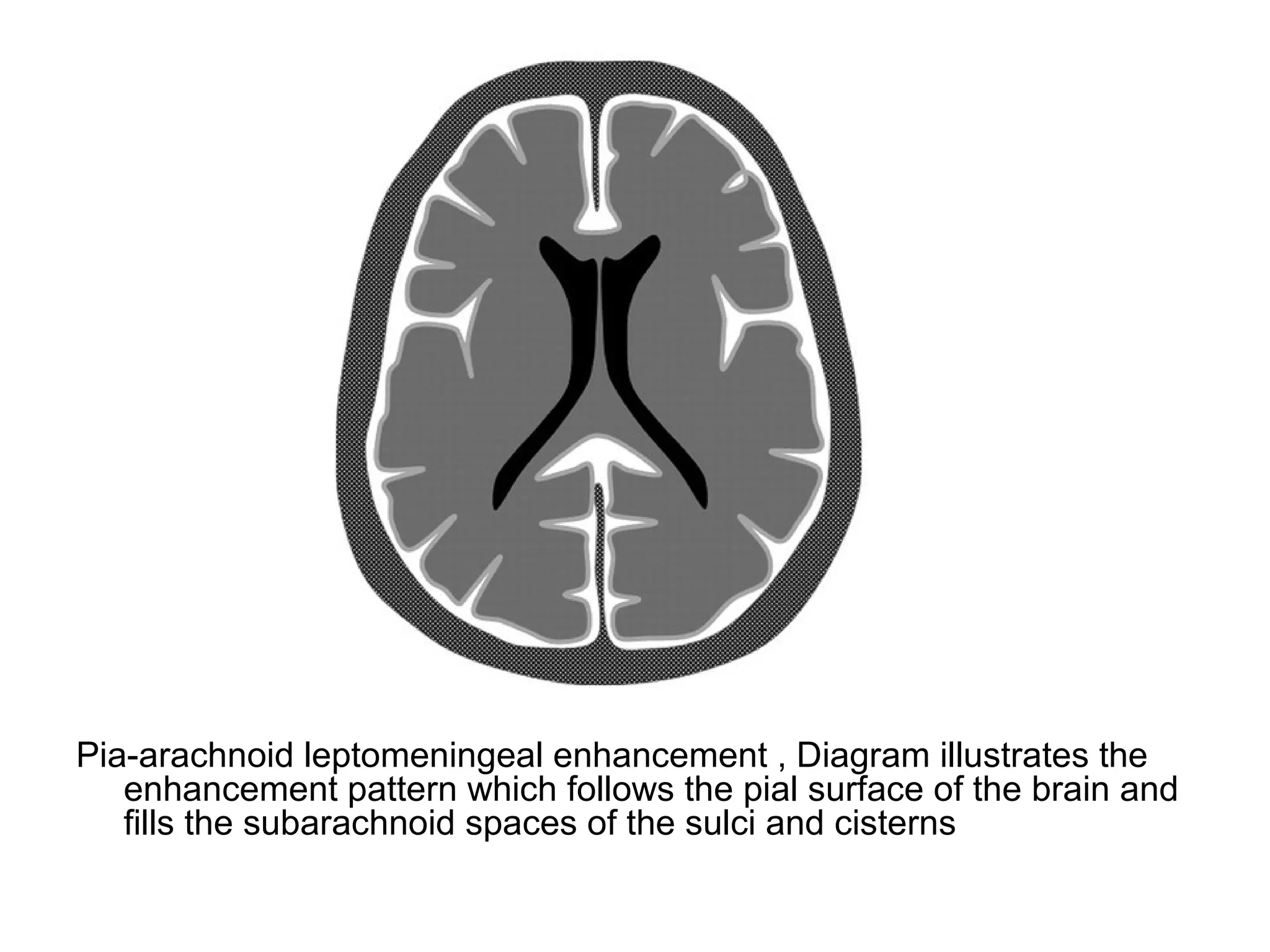
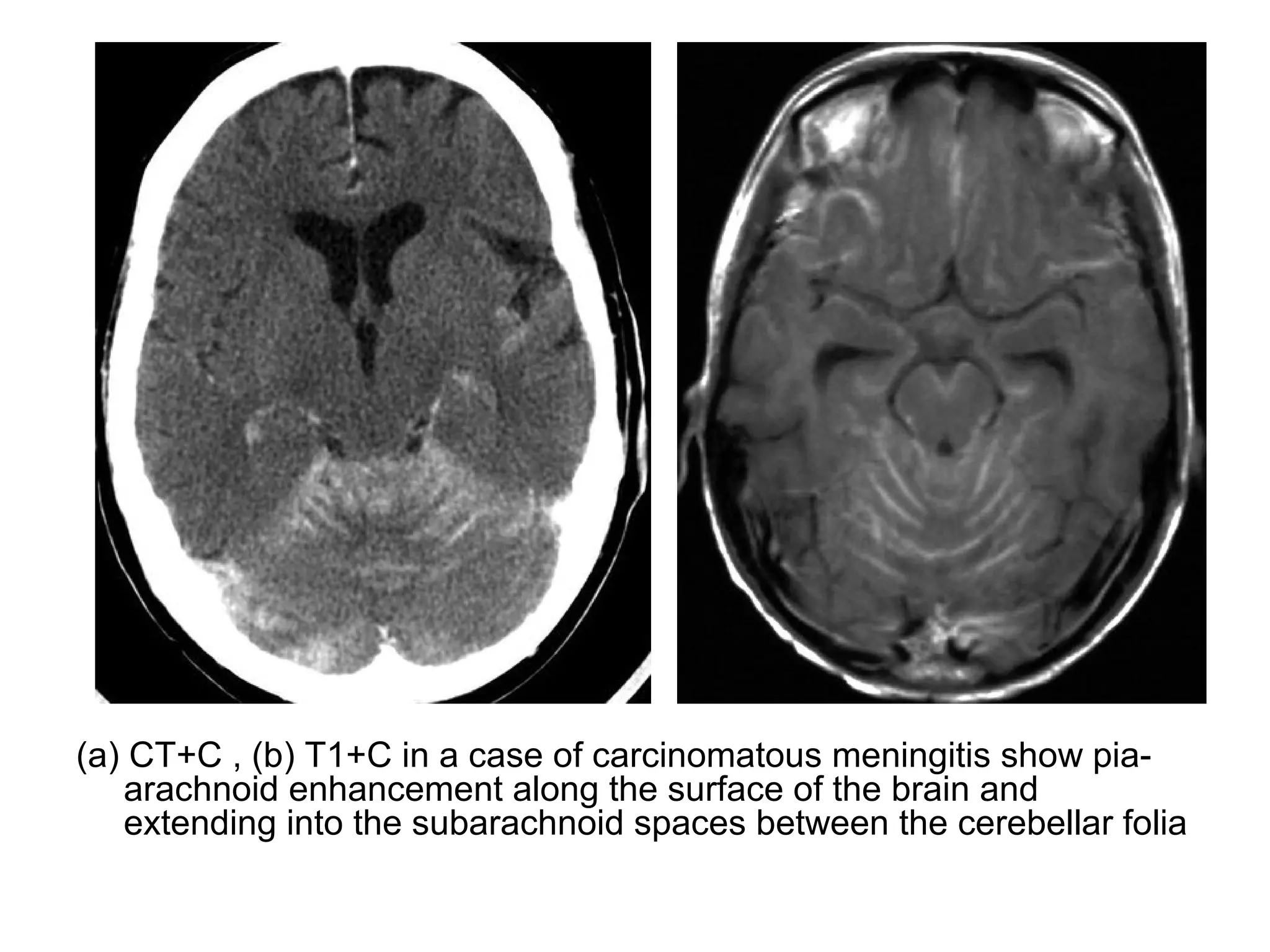
The document discusses patterns of brain enhancement seen on MRI or CT after contrast administration. It describes 6 common patterns: 1) Periventricular enhancement which can be seen in conditions like lymphoma, infections, or multiple sclerosis. 2) Gyriform enhancement seen in herpes encephalitis, infarcts, or PRES. 3) Nodular subcortical enhancement typically seen in metastatic disease. 4) Ring enhancement commonly from abscesses, metastases, or high grade tumors. 5) Pachymeningeal enhancement of the dura. 6) Leptomeningeal enhancement of the pia-arachnoid membranes. Normal structures that enhance include the choroid plexus, pituitary gland, pineal