This document discusses the considerations surrounding anticoagulation treatment in a 76-year-old female patient who experienced a cardioembolic stroke likely due to atrial fibrillation. It examines the balance of risks and benefits related to anticoagulation therapy, citing various studies and guidelines that support the use of anticoagulants such as heparin or warfarin for stroke prevention while also addressing concerns about hemorrhagic transformation. Ultimately, the document emphasizes the need for individualized treatment strategies in managing the patient's condition.
![STROKE RISK IN PATIENTS WITH NONVALVULAR
AF NOT
TREATED WITH ANTICOAGULATION ACCORDING
TO THE CHADS2 INDEX
[1]van Walraven WC, Hart RG, Wells GA, et al. A clinical prediction rule to identify patients with atrial fibrillation and a low risk for stroke while taking aspirin.
Arch Intern Med 2003;163:936–43415;
[2] Gage BF, Waterman AD, Shannon W, et al. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial
Fibrillation. JAMA 2001;285:2864 –70.](https://image.slidesharecdn.com/anticoagulationinstroke-adebate-121005100115-phpapp01/85/Anticoagulation-in-cardio-embolic-stroke-a-debate-12-320.jpg)
![ACCP GUIDELINES
ANTITHROMBOTIC AND THROMBOLYTIC THERAPY
FOR ISCHEMIC STROKE
Oral anticoagulant therapy is highly effective for both primary
and secondary prevention of stroke in patients with atrial
fibrillation .
In the European Atrial Fibrillation Trial, patients with
recent stroke or TIA and atrial fibrillation were treated with
oral anticoagulation.
In about half of the patients, anticoagulation was initiated
within 2 weeks after symptom onset. No increase in brain
hemorrhage was apparent in patients treated early vs later.
In general, we recommend initiation of oral anticoagulation
therapy within 2 weeks of a cardioembolic stroke.
Recommendation:In patients with atrial fibrillation
who have suffered a recent stroke or TIA, we
recommend long-term oral anticoagulation (target INR,
2.5; range, 2.0 to 3.0) [Grade 1A].
Chest - Volume 133, Issue 6 (June 2008)
EAFT (European Atrial Fibrillation Trial) Study Group : Secondary prevention in
non-rheumatic atrial fibrillation after transient ischaemic attack or minor
stroke. Lancet 342. 1255-1262.1993](https://image.slidesharecdn.com/anticoagulationinstroke-adebate-121005100115-phpapp01/85/Anticoagulation-in-cardio-embolic-stroke-a-debate-20-320.jpg)
![ A large metaanalysis of 22 trials among 23,547 patients
showed that immediate anticoagulation of patients with acute
ischemic stroke was not associated with a significant reduction
in death or dependency. [1]
Although anticoagulants were associated with about 9 fewer
recurrent ischemic strokes per 1,000 treated, this was offset by
a similar increase of 9 symptomatic intracranial hemorrhages
per 1,000 treated.
Only a single randomized trial has evaluated this regimen
compared with placebo for patients with acute stable stroke
since 1980.
No significant difference in stroke progression or neurologic
outcome was detected in this relatively small study (n = 225).
[2]
[1]Gubitz G, Sandercock P, Counsell C: Anticoagulants for acute ischaemic
stroke. Cochrane Database Syst Rev . CD000024.2004
[2]Duke RJ, Bloch RF, Turpie AG, et al: Intravenous heparin for the
prevention of stroke progression in acute partial stable stroke. Ann Intern
Med 105. 825-828.1986](https://image.slidesharecdn.com/anticoagulationinstroke-adebate-121005100115-phpapp01/85/Anticoagulation-in-cardio-embolic-stroke-a-debate-28-320.jpg)
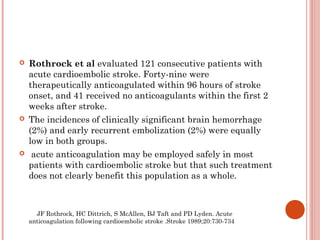
![ The Cerebral Embolism Study Group reported that 22 of
24 patients with symptomatic hemorrhagic transformation
were associated with anticoagulation therapy[1] .
Some reports suggest that although anticoagulation does
not precipitate hemorrhagic transformation,
anticoagulation may worsen the severity of spontaneous
bleeding (Cerebral Embolism Study Group
1983[1]; 1987[2]).
[1]Immediate anticoagulation of embolic stroke: a randomized trial.
Cerebral Embolism Study Group. Stroke 1983, 14:668-676
[2]Cardioembolic stroke, early anticoagulation, and brain
hemorrhage. Cerebral Embolism Study Group.Arch Intern Med.
1987 Apr;147(4):636-40.](https://image.slidesharecdn.com/anticoagulationinstroke-adebate-121005100115-phpapp01/85/Anticoagulation-in-cardio-embolic-stroke-a-debate-30-320.jpg)
![DVT & PE
DVT and PE are frequent complications of stroke, with about 5%
of early deaths attributed to PE. [1]
In an overview analysis among acute stroke patients,
anticoagulants were associated with 4 fewer pulmonary emboli
per 1,000 (OR, 0.60; 95% CI, 0.44–0.81). [2]
In the IST, there was a significant reduction in the frequency of
fatal or nonfatal PE, from 0.8 to 0.5%, among those treated with
SC UFH (p < 0.05). [3]
In a metaanalysis among 740 acute ischemic stroke subjects from
four trials, there was a significant reduction in the odds of DVT
(OR, 0.52; 95% CI, 0.56–0.79) among those allocated to low-
molecular-weight heparins or heparinoids vs standard UFH. [4]
Two trials of direct comparisons between a low-molecular-weight
heparin and UFH have shown similar safety and efficacy for
enoxaparin and noninferiority for certoparin. [5] , [6]](https://image.slidesharecdn.com/anticoagulationinstroke-adebate-121005100115-phpapp01/85/Anticoagulation-in-cardio-embolic-stroke-a-debate-32-320.jpg)
![PREVAIL
PREVENTION OF VENOUS
THROMBOEMBOLISM AFTER ACUTE
ISCHEMIC STROKE
Open-label, randomized comparison of enoxaparin 40 mg
SC qd or UFH 5,000 U SC q12h in patients with ischemic
stroke [7]
1,762 patients randomized within 48 h of symptom onset
and stratified on stroke severity (NIHSS < or ≥14).
10% patients in the enoxaparin group had a primary end
point compared to 18% in patients randomized to UFH,
yielding a 43% RRR (0.57; 95% CI, 0.44–0.76; p = 0.0001).
The results for proximal DVT were 5% in the enoxaparin
group and 10% in the UFH group (p = 0.0003).
The risk of both symptomatic intracranial bleeding and
major extracranial hemorrhage was also similar in both
groups (1% each)](https://image.slidesharecdn.com/anticoagulationinstroke-adebate-121005100115-phpapp01/85/Anticoagulation-in-cardio-embolic-stroke-a-debate-33-320.jpg)
![ANTITHROMBOTIC AND THROMBOLYTIC
THERAPY 8TH ED: ACCP GUIDELINES
ANTITHROMBOTIC AND THROMBOLYTIC
THERAPY FOR ISCHEMIC STROKE
For acute stroke patients with restricted mobility,
we recommend prophylactic low-dose SC heparin
or low-molecular-weight heparins (Grade 1A).
[1] Antiplatelet Trialists' Collaboration : Collaborative overview of randomised trials of antiplatelet therapy: III. Reduction
in venous thrombosis and pulmonary embolism by antiplatelet prophylaxis among surgical and medical patients.
BMJ 308. 235-246.1994
[2] Gubitz G, Sandercock P, Counsell C: Anticoagulants for acute ischaemic stroke. Cochrane Database Syst
Rev . CD000024.2004
[3] International Stroke Trial (IST) : A randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435
patients with acute ischaemic stroke: International Stroke Trial Collaborative Group. Lancet 349. 1569-1581.1997;
[4] Sandercock P, Counsell C, Stobbs SL: Low-molecular-weight heparins or heparinoids versus standard unfractionated
heparin for acute ischaemic stroke. Cochrane Database Syst Rev . CD000119.2005;
[5] Diener HC, Ringelstein EB, von Kummer R, et al: Prophylaxis of thrombotic and embolic events in acute ischemic
stroke with the low-molecular-weight heparin certoparin: results of the PROTECT Trial. Stroke 37. 139-144.2006
[6 ]Hillbom M, Erila T, Sotaniemi K, et al: Enoxaparin vs heparin for prevention of deep-vein thrombosis in acute
ischaemic stroke: a randomized, double-blind study. Acta Neurol Scand 106. 84-92.2002;
[7] Sherman DG, Albers GW, Bladin C, et al: The efficacy and safety of enoxaparin versus unfractionated heparin for the
prevention of venous thromboembolism after acute ischaemic stroke (PREVAIL Study): an open-label randomised
comparison. Lancet 369. 1347-1355.2007;](https://image.slidesharecdn.com/anticoagulationinstroke-adebate-121005100115-phpapp01/85/Anticoagulation-in-cardio-embolic-stroke-a-debate-34-320.jpg)