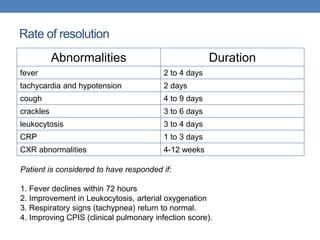
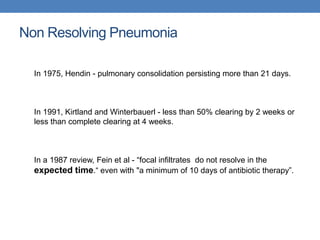
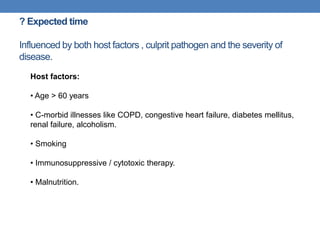
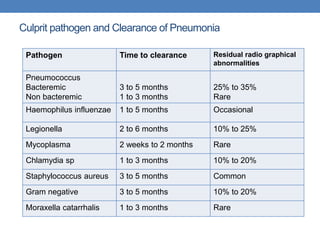
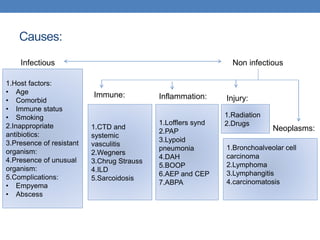
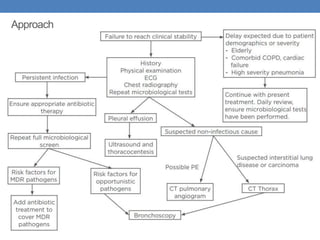
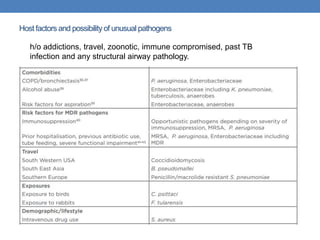
1. Dr. Rajkoti discusses the approach to evaluating and managing non-resolving pneumonia. Key factors that can delay resolution are host factors like age, comorbidities, and smoking as well as drug-resistant or unusual pathogens.
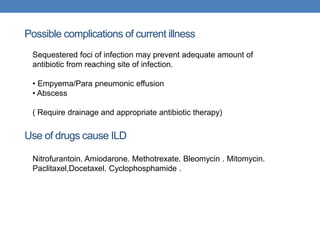
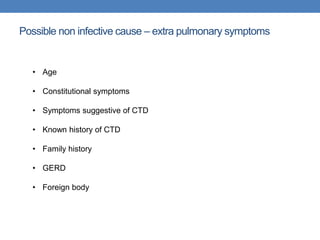
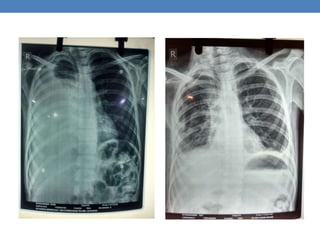
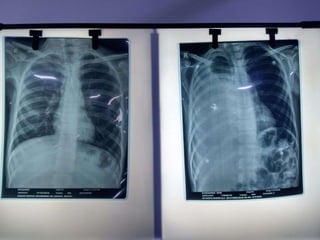
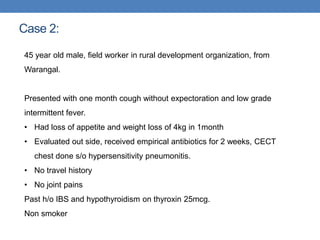
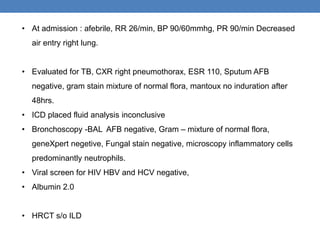
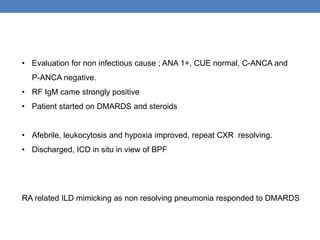
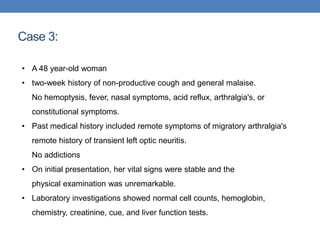
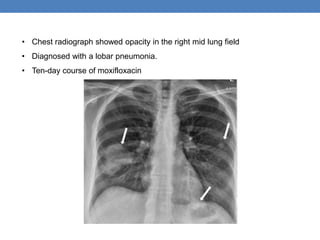
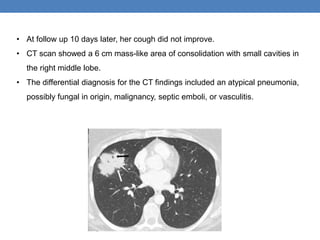
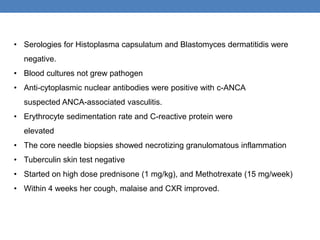
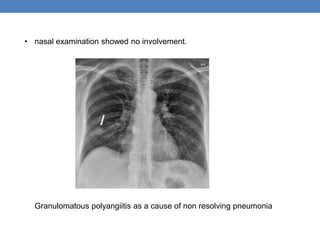
2. Three case studies are presented. The first involves a teenage boy with empyema that required drainage. The second is a middle-aged man with hypersensitivity pneumonitis related to his job that responded to steroids. The third involves further evaluation of a woman's non-productive cough to identify potential non-infectious causes.
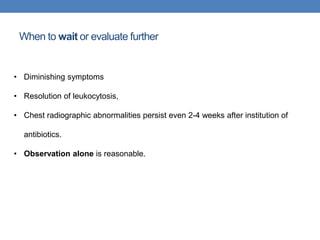
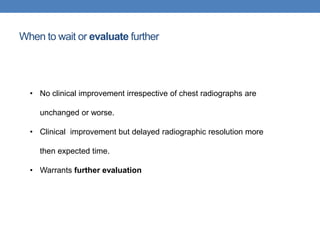
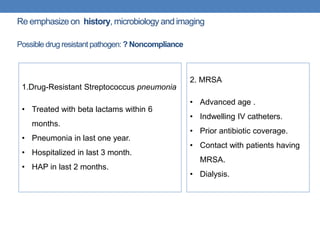
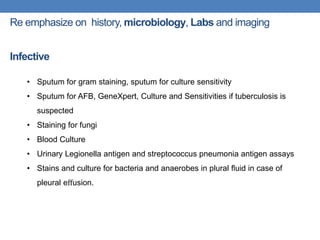
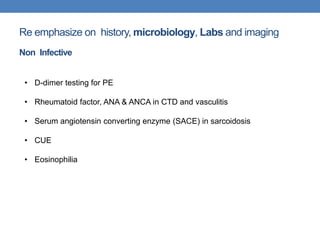
3. For non-resolving pneumonia, re-emphasis is placed on thorough history, microbiology testing, imaging,