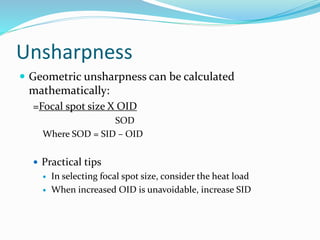
This document discusses factors that affect radiographic image quality. It defines key terms like image, noise, contrast, sharpness and resolution. It explains how controlling factors like exposure, kilovoltage and grid usage impact the photographic properties of density and contrast. Geometric properties like sharpness and distortion are also influenced by the focal spot size, SID, OID and motion. Both film-based and digital systems consider these technical parameters to optimize visibility and accuracy of anatomical details in medical images.