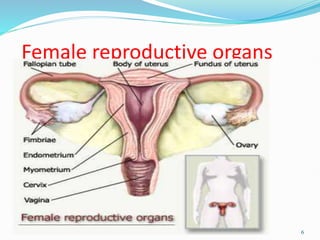
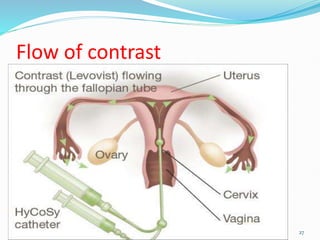
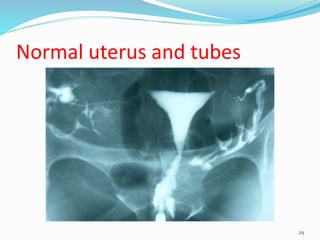
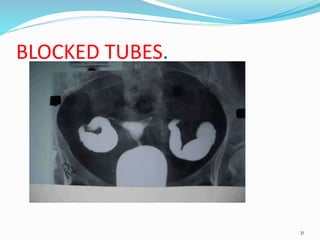
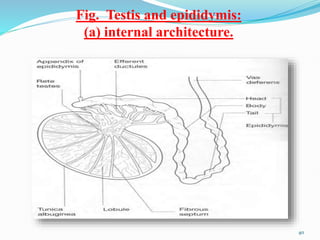
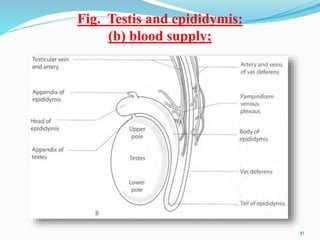
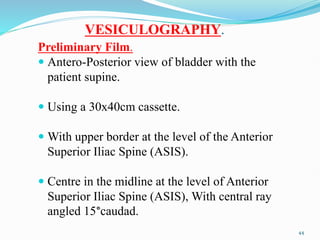
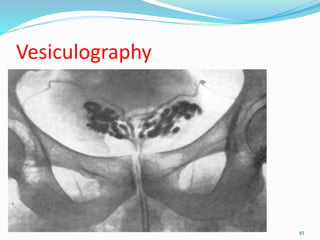
The document describes the anatomy and radiographic procedures related to the male and female reproductive systems. It discusses the internal and external organs of the female system including the ovaries, uterus, fallopian tubes, and vagina. It also describes the male reproductive organs such as the testes, vas deferens, seminal vesicles, and prostate gland. Several radiographic techniques are explained including hysterosalpingography to examine the uterus and fallopian tubes, and vesiculography to examine the vas deferens and seminal vesicles. Both procedures involve injecting contrast medium to visualize the ducts and ensure there are no blockages.