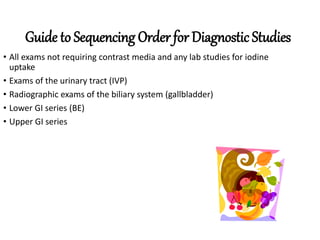
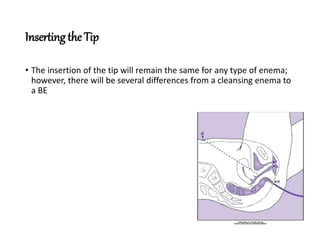
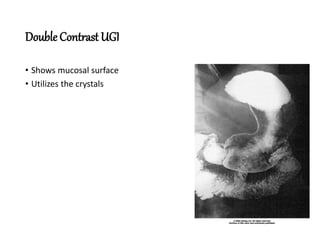
This document provides information on preparing patients and performing various gastrointestinal (GI) imaging exams. It discusses scheduling considerations, common prep methods like diet restrictions and laxatives, and specifics on barium and water-soluble contrast exams of the upper and lower GI tract. Key preparation steps are outlined for upper GI series, double contrast UGI, lower GI series including bowel cleansing techniques, and special considerations for certain patient conditions.