The document discusses concepts related to x-ray attenuation including:
1. Attenuation is the reduction in intensity of an x-ray beam as it passes through matter by absorption or deflection of photons.
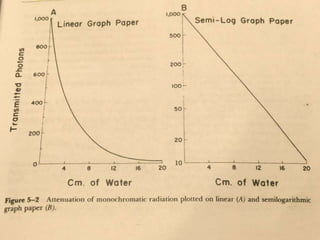
2. Exponential attenuation occurs when the number of photons decrease by the same percentage with each increment of absorber thickness, as seen with monochromatic radiation.
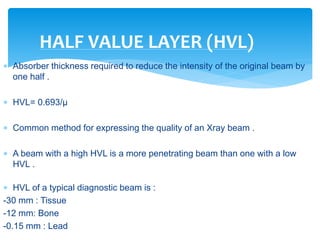
3. The half value layer is the thickness of absorber needed to reduce the intensity of an x-ray beam by half.