This document summarizes several neurological conditions associated with HIV, including:
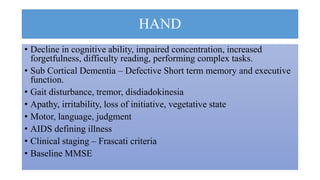
1. HIV-associated neurocognitive disorder (HAND), which has three stages from asymptomatic to HIV-associated dementia.
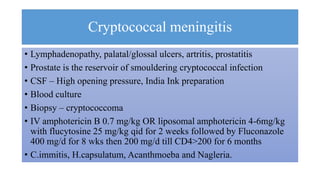
2. Aseptic meningitis, cryptococcal meningitis, toxoplasmosis, progressive multifocal leukoencephalopathy (PML), and spinal cord diseases like vacuolar myelopathy are also discussed.
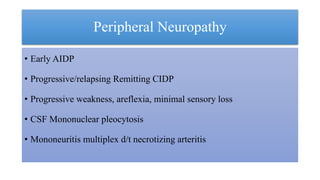
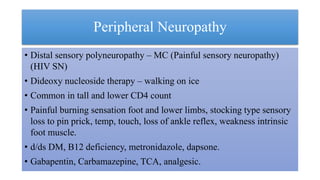
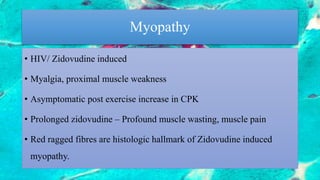
3. Peripheral neuropathies are common, especially a painful sensory neuropathy, as well as myopathies related to HIV or antiretroviral medications.