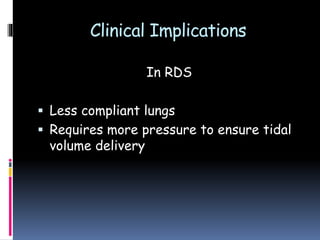
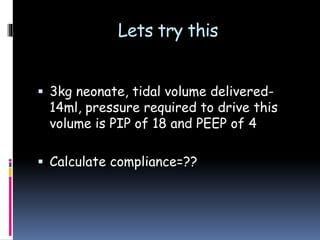
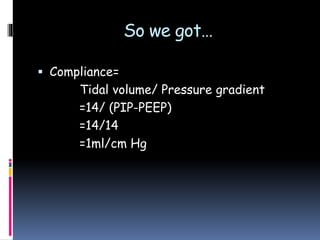
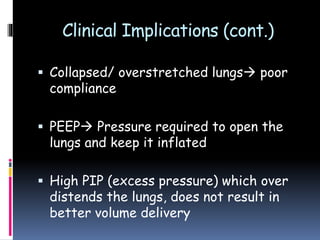
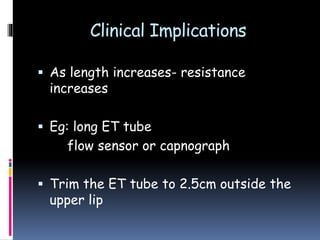
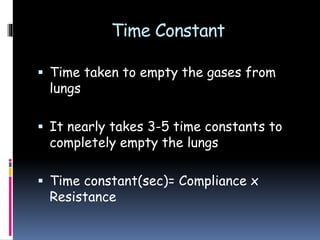
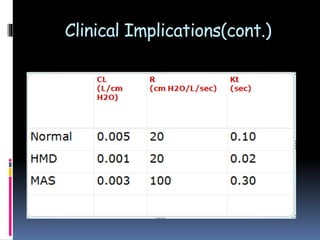
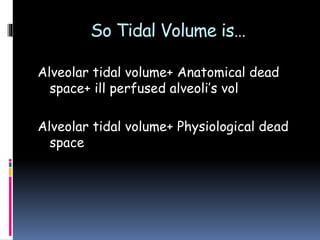
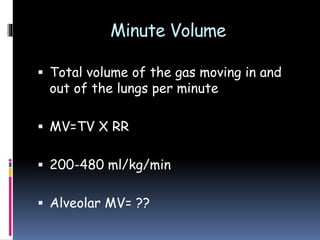
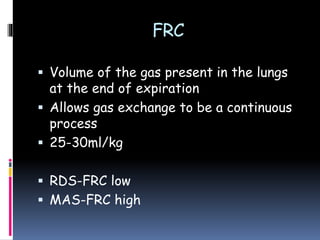
This document discusses neonatal respiratory mechanics, including compliance, resistance, time constant, lung volumes, oxygenation, and carbon dioxide removal. It defines key terms and explores their clinical implications. Compliance refers to lung distensibility, resistance is the oppositional force to airflow, and time constant is the time to empty the lungs. Together these properties determine ventilation and gas exchange effectiveness. Various ventilation strategies aim to optimize these factors to achieve goals of oxygenation and carbon dioxide removal.




























![Question 1
1]True about RDS is?
A] Low compliance, High resistance
B]High compliance, Low resistance
C]Low compliance, Normal Resistance
D]High compliance, High resistance](https://image.slidesharecdn.com/mec0711-170420180545/85/NEONATAL-RESPIRATORY-MECHANICS-51-320.jpg)
![Question 2
2]Which of the following will affect
PaCO2 maximum?
A]Secretions in the ET tube
B]Respiratory Rate
C]Tidal volume
D]Dead space](https://image.slidesharecdn.com/mec0711-170420180545/85/NEONATAL-RESPIRATORY-MECHANICS-52-320.jpg)
![Question 3
3] Which is a wrong match?
A] FRC—PVR
B] PaO2—MAP
C] PaCO2—TV
D] MAP—FiO2](https://image.slidesharecdn.com/mec0711-170420180545/85/NEONATAL-RESPIRATORY-MECHANICS-53-320.jpg)