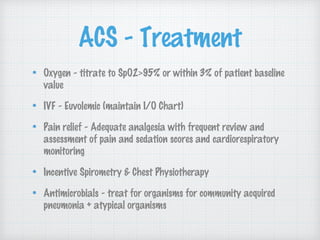
This document defines and discusses acute chest syndrome (ACS) in patients with sickle cell disease. ACS is characterized by fever, respiratory symptoms, and new lung infiltrates seen on chest x-ray. It is commonly caused by infection, fat embolism, or hypoventilation. Clinical features include chest pain and symptoms like cough. Diagnosis can be challenging as symptoms may be mild and radiological signs lag behind. Treatment involves oxygen, IV fluids, pain management, respiratory support like bronchodilators, and antibiotics. Preventing recurrent ACS involves therapies like hydroxyurea and long-term blood transfusions. Distinguishing asthma from wheezing caused by sickle cell disease can also be difficult.