Hematology is the scientific study of blood, blood-forming tissues, and related disorders, focusing on diagnoses, treatments, and diseases such as anemia, blood cancers, and clotting disorders. A Complete Blood Count (CBC) tests various blood components including red and white blood cells, hemoglobin, and platelets, providing insight into a patient's overall health and potential medical conditions. The document outlines blood composition, function, laboratory testing methodologies, and the significance of testing results in diagnosing various health issues.


























![Calculating the Hematocrit
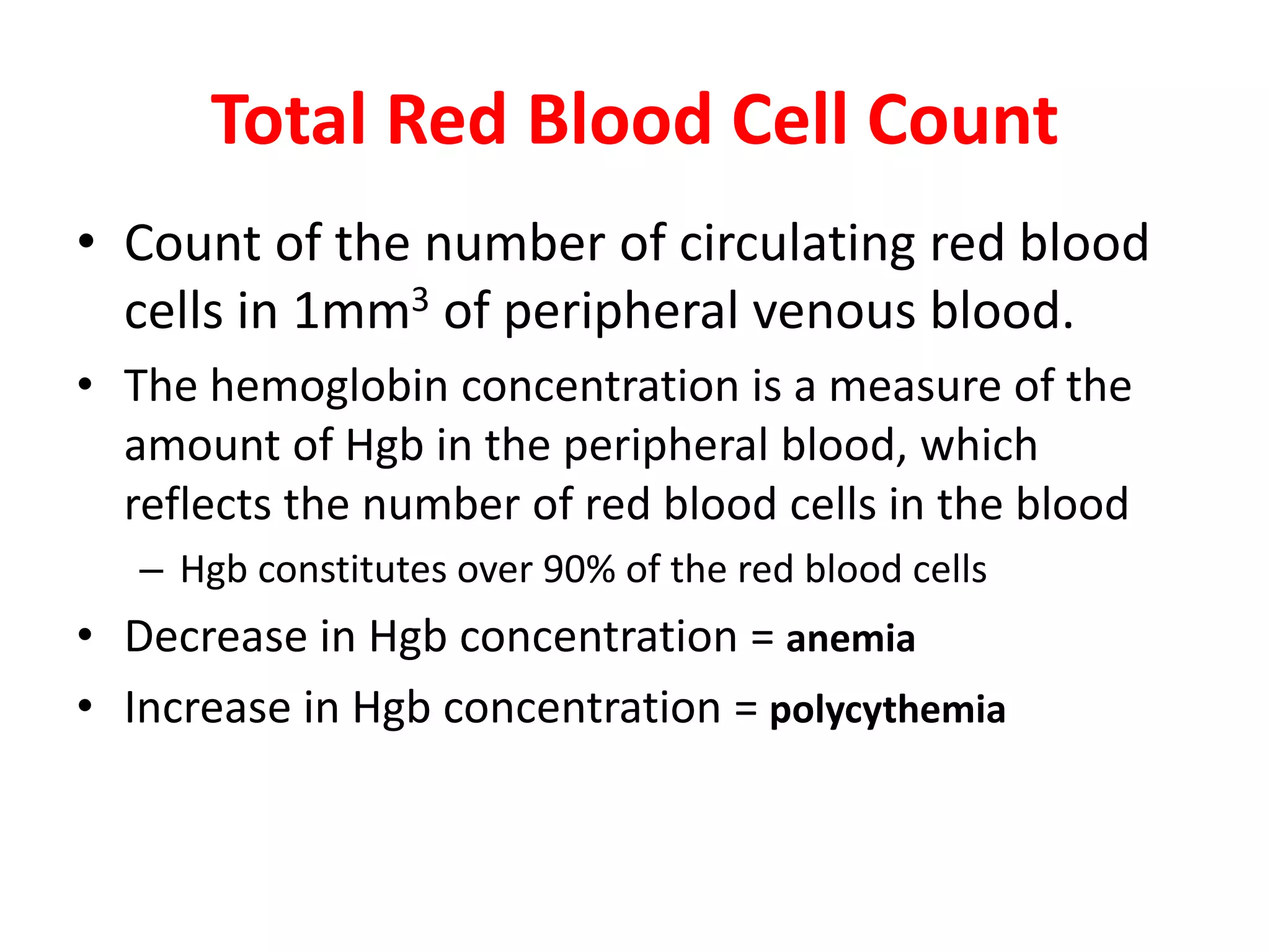
• More commonly the Hct is calculated directly
from the RBC and MCV
– Hematocrit % = RBC (cells/liter) x MCV (liter/cell)
Mean Corpuscular Volume
• The MCV is a measure of the average volume, or size,
of an RBC
• To calculate MCV, the hematocrit (Hct) is divided by
the concentration of RBCs ([RBC])
• For example, if the Hct = 42.5% and [RBC] = 4.58
million per microliter (4,580,000/μL), then
= 92.8 . 1015 or 92.8 fL](https://image.slidesharecdn.com/hematology-211214045901/75/Hematology-30-2048.jpg)