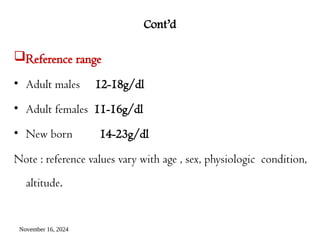
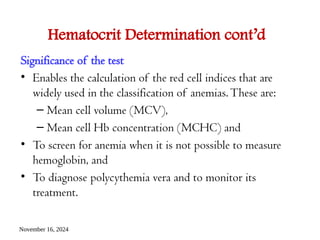
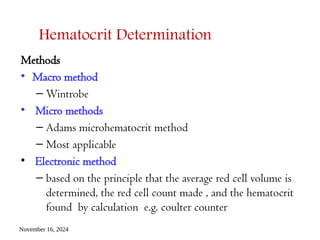
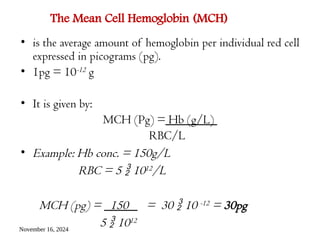
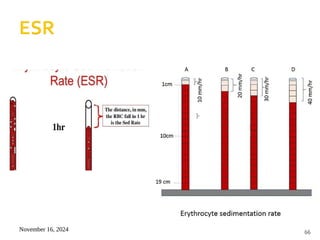
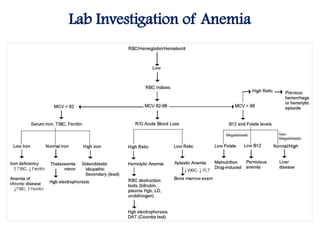
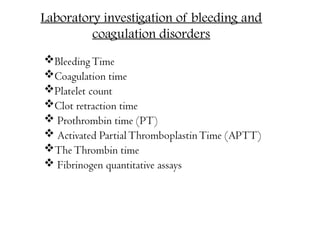
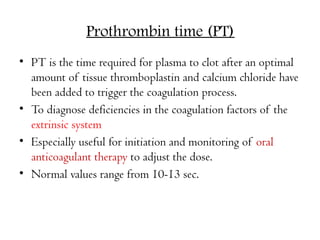
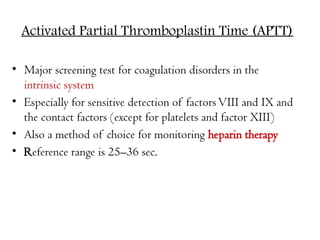
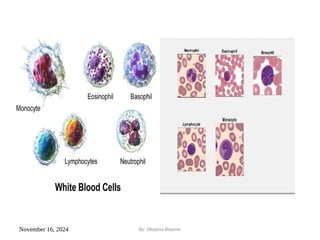
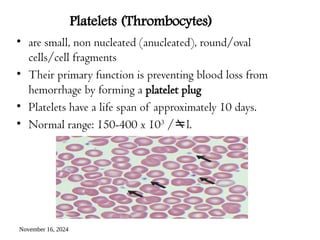
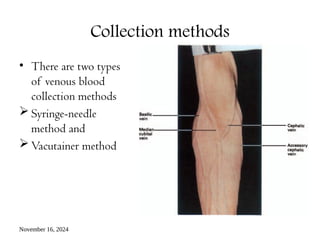
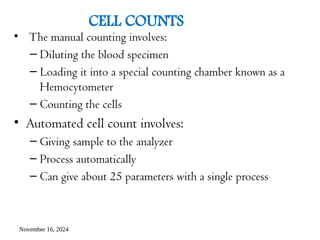
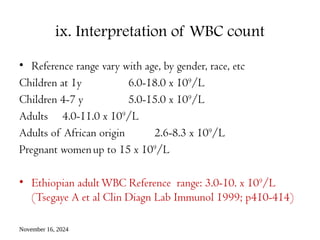
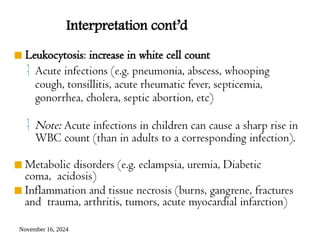
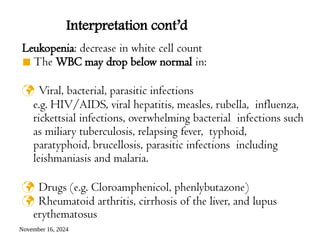
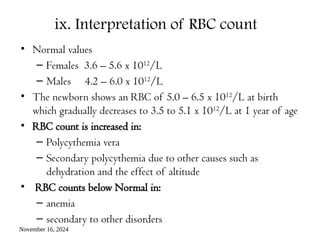
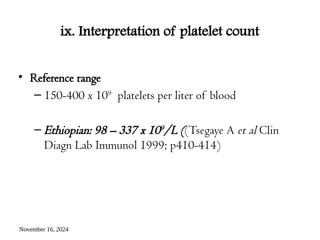
Chapter two focuses on basic hematological tests, outlining objectives for students covering blood composition, formation, and basic testing methods. Key components discussed include blood cell types (erythrocytes, leukocytes, and platelets), their functions, and the significance of various blood tests such as cell counts, hemoglobin determination, and packed cell volume (PCV). The chapter emphasizes sample collection techniques and interpretation of test results, including normal ranges and implications of deviations.














![November 16, 2024
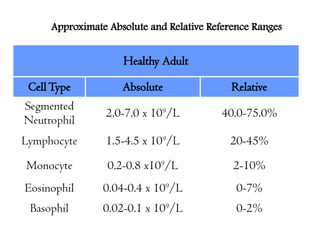
Neutrophils
• are the most common type of WBCs in adults
• The segmented neutrophils “segs,” also called
polymorphonuclear leukocytes [PMNs or
“polys”]
• are the primary defense against bacterial
infection](https://image.slidesharecdn.com/ch2basichematologicaltests-241116213302-6802fa45/85/CH-2-basic-hematological-tests-pptx-clinical-28-320.jpg)