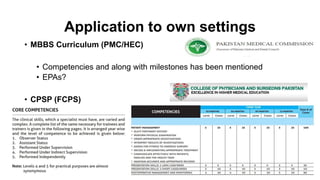
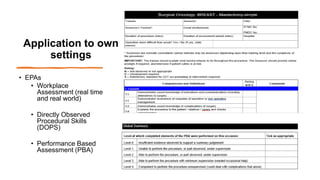
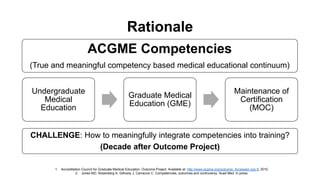
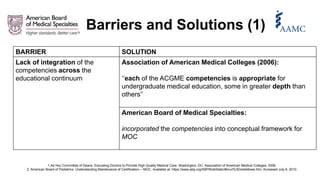
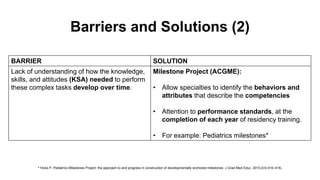
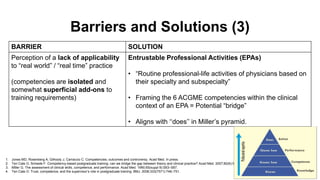
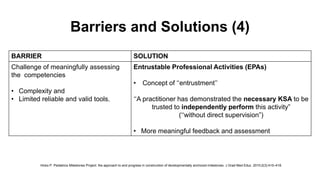
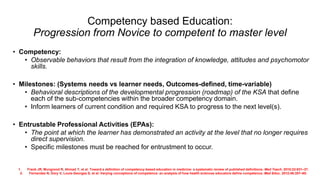
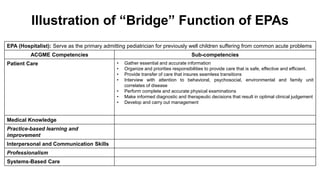
The document discusses the integration of ACGME competencies into medical education, emphasizing the need for meaningful incorporation of these standards throughout training. It identifies barriers to effective competency-based education, such as lack of integration and real-world applicability, and proposes solutions like the use of entrustable professional activities (EPAs) to bridge the gap between theory and practice. The commentary highlights the movement towards standardizing competency language across the medical education continuum, advocating for a focus on developmental roadmaps and effective workplace assessments.
![Competencies
• Six Core Competency domains for residency education in North America (ACGME
Outcome Project 1999) [1,2]
• Patient care
• Medical Knowledge
• Practice-based learning and improvement
• Interpersonal and Communication Skills
• Professionalism
• Systems-Based Care
• 2013 review: [3-5]
• Interprofessionalism (2011)
• Personal and Professional Identity Formation. (2010 Carnegie report)
1. Swing SR. The ACGME outcome project: retrospective and prospective. Med Teach. 2007;29:648–54.
2, ten Cate O, Snell L, Carraccio C. Medical competence: the interplay between individual ability and the health care environment. Med Teach. 2010;32:669–75.
3. Englander R, Cameron T, Ballard AJ, et al. Toward a common taxonomy of competency domains for the health professions and competencies for physicians. Acad Med. 2013;88:1088–94.
4. Interprofessional Education Collaborative Expert Panel. Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel. Washington, D.C.: Interprofessional Education Collaborative;
2011.
5. Cooke M, Irby DM, O’Brien BC. Educating Physicians: A Call for Reform of Medical School and Residency. San Francisco: Jossey-Bass; 2010. P. 41.](https://image.slidesharecdn.com/epapresentation-220319063717/85/Beyond-Competencies-and-Milestones-Adding-Meaning-Through-Context-10-320.jpg)
![Association of American Medical Colleges (AAMC) : 2013
• Reference List of General Physician Competencies
• All medical schools map their educational program objectives accordingly.
• Core Entrustable Professional Activities
for Entering Residency (CEPEAR)
• For medical students
1. Englander R, Cameron T, Ballard AJ, et al. Toward a common taxonomy of competency domains for the health professions and competencies for physicians. Acad Med. 2013;88:1088–94.
2. Association of American Medical Colleges. Core Entrustable Professional Activities for Entering Residency (CEPEAR) [Internet]. Washington, D.C. March 2014. Available at www
.mededportal.org/icollaborative/resource/887.](https://image.slidesharecdn.com/epapresentation-220319063717/85/Beyond-Competencies-and-Milestones-Adding-Meaning-Through-Context-12-320.jpg)