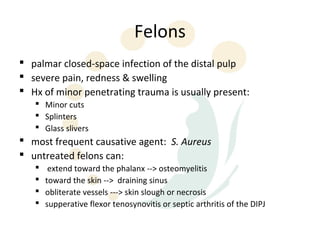
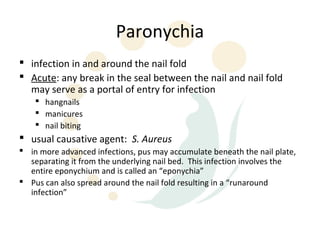
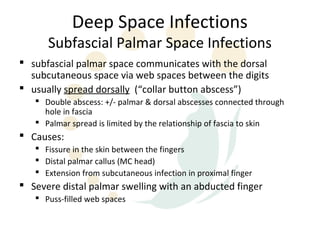
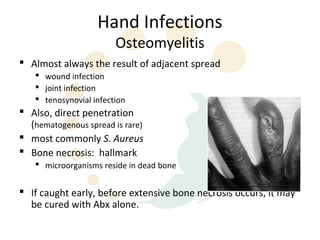
The document discusses hand infections, including their history and treatment principles. It covers topics like felons, paronychia, tenosynovitis, and other specific types of hand infections. Some key points:
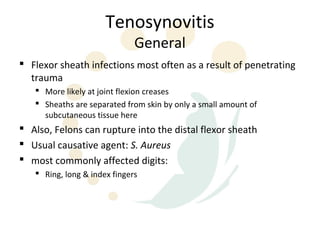
- Prior to antibiotics, many hand deformities and disabilities resulted from minor injuries becoming infected. Careful surgical techniques helped treatment.
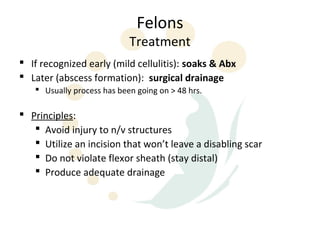
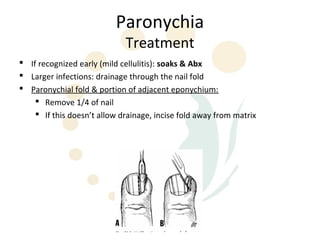
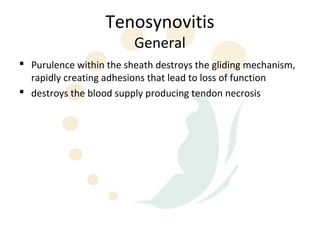
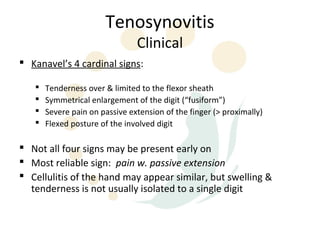
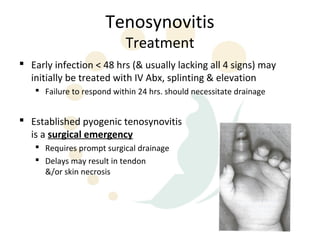
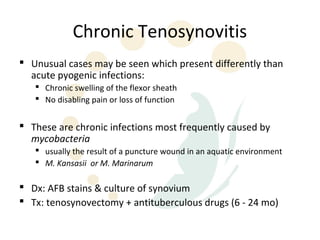
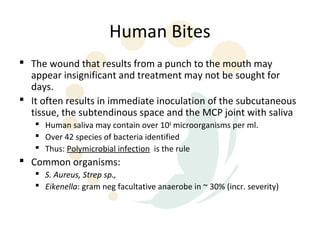
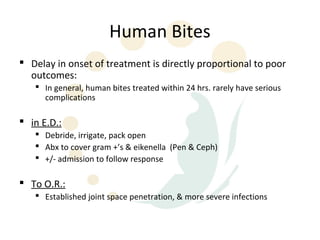
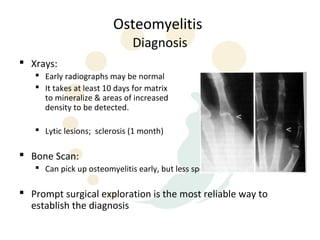
- Penicillin revolutionized treatment by making severe infections less common today. Early diagnosis and treatment with antibiotics, splinting and elevation can help cure some infections.
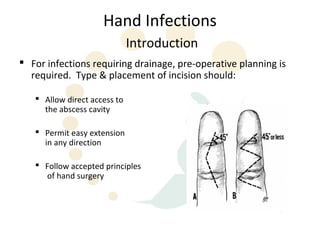
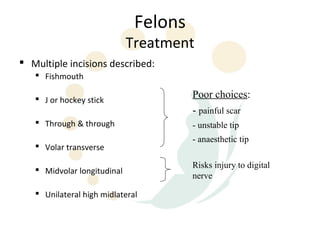
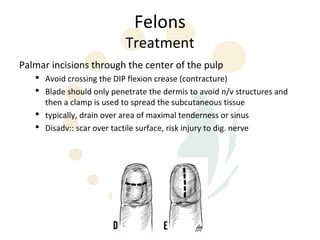
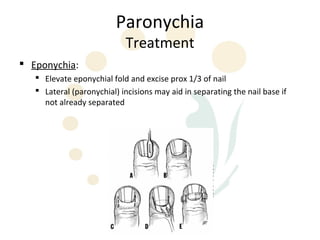
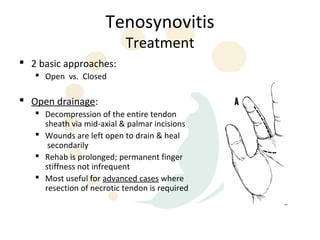
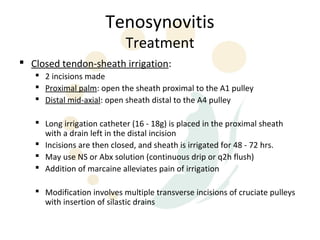
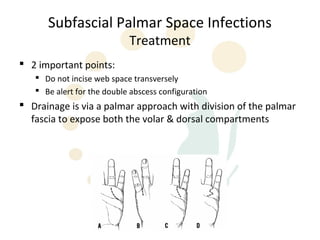
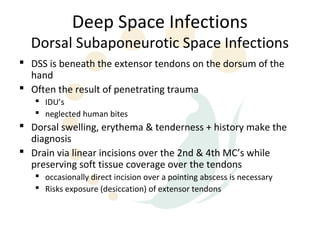
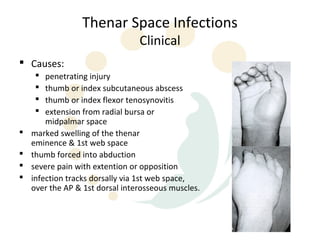
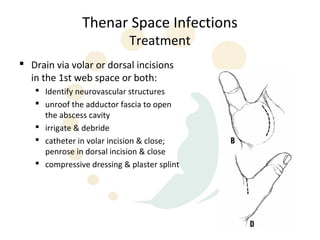
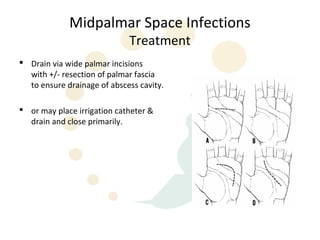
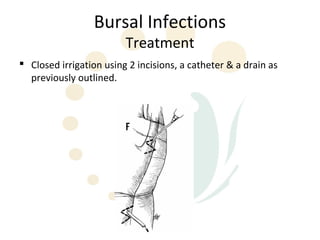
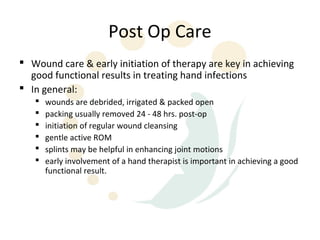
- Surgical drainage and debridement may be needed for established infections to prevent complications like joint stiffness or contractures. Appropriate antibiotic use and incision placement are important for optimal outcomes.