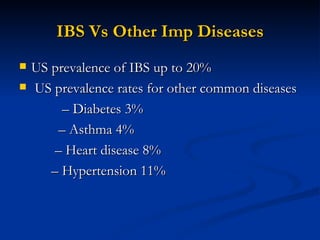
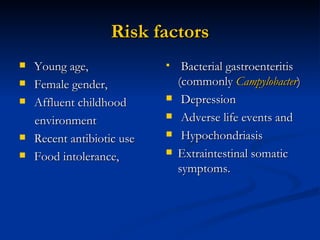
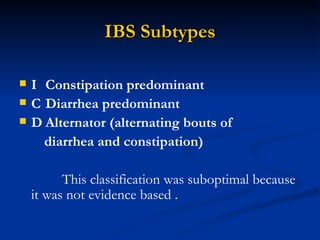
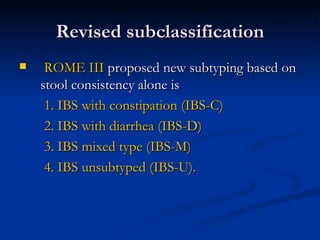
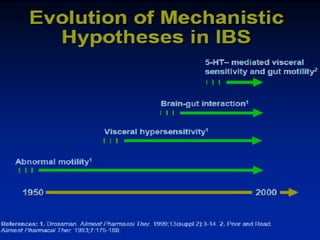
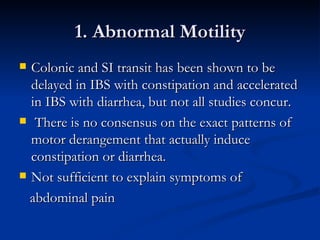
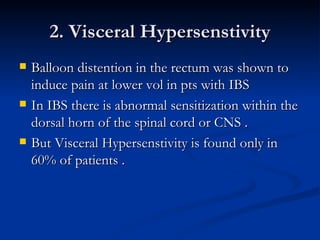
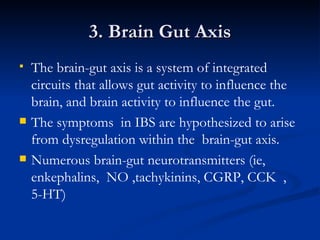
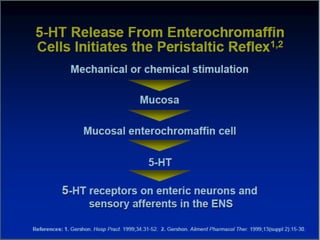
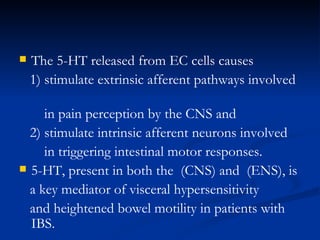
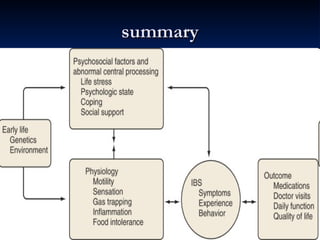
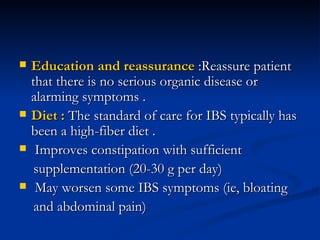
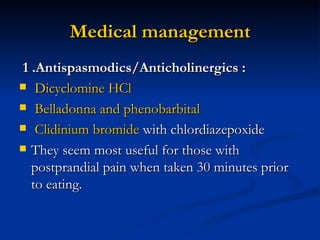
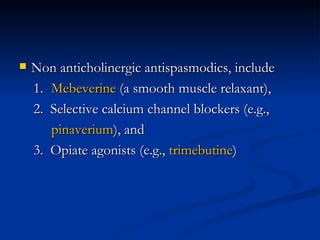
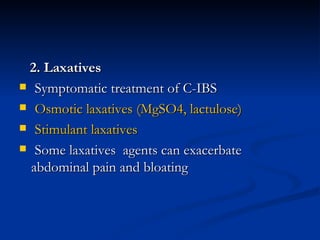
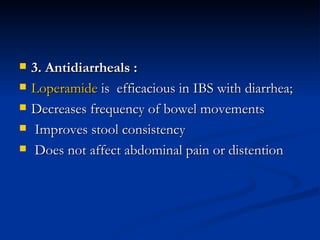
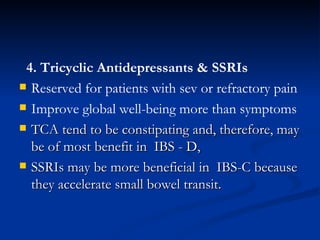
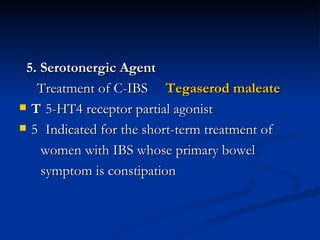
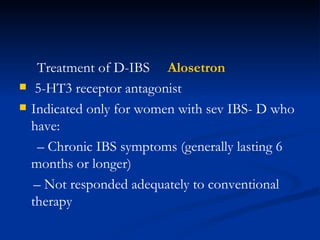
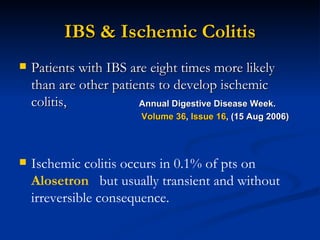
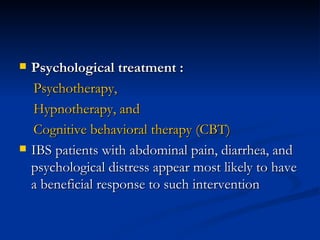
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder defined by abdominal pain associated with changes in bowel habits. IBS prevalence ranges from 3-20% worldwide and is more common in younger individuals and women. IBS has subtypes including constipation-predominant, diarrhea-predominant, and mixed-type based on stool consistency. The pathophysiology of IBS involves abnormal gut motility, visceral hypersensitivity, brain-gut axis dysregulation, and abnormal chemical signaling. Treatment focuses on diet, medication to relieve symptoms, and psychological therapies depending on the individual's dominant symptoms and severity.