This document provides an overview of ascites, including:
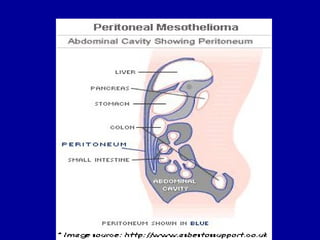
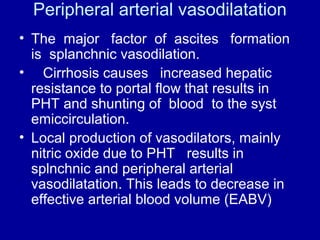
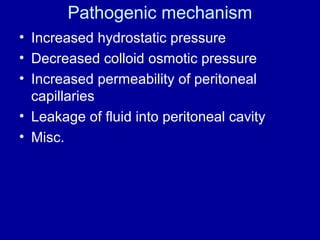
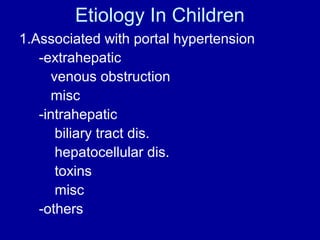
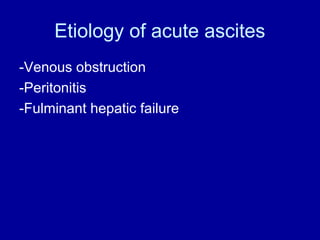
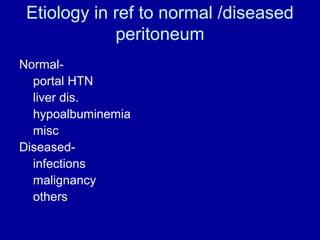
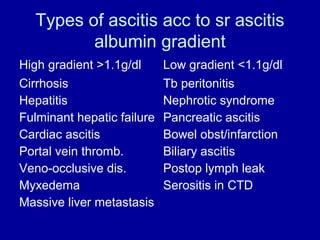
- Ascites is an accumulation of fluid in the peritoneal cavity. It is usually caused by cirrhosis and portal hypertension which increases hydrostatic pressure in blood vessels in the abdomen.
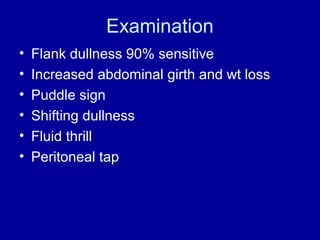
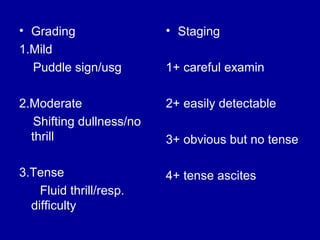
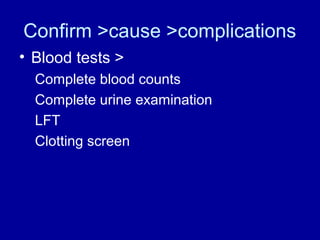
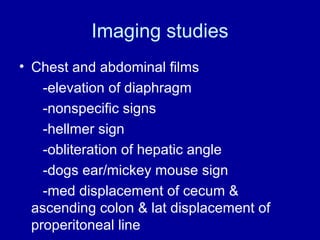
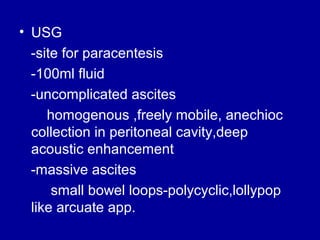
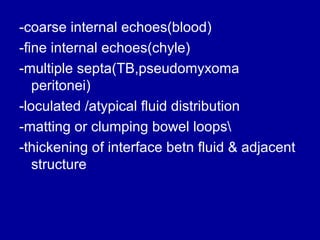
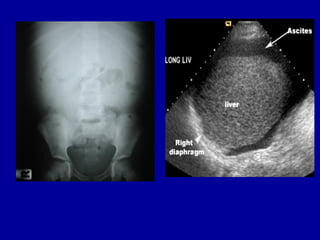
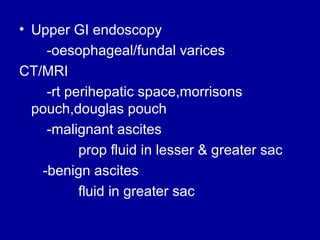
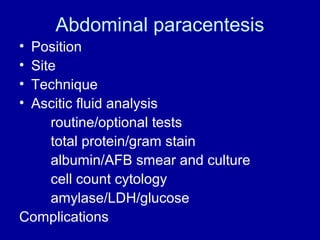
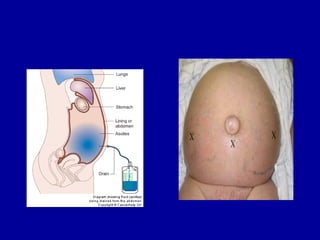
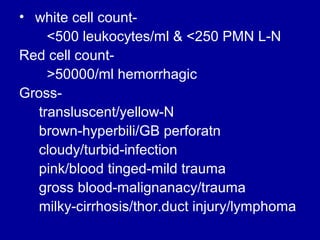
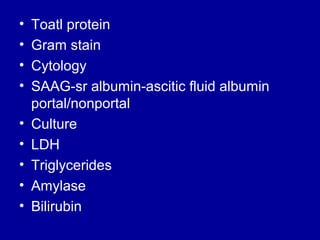
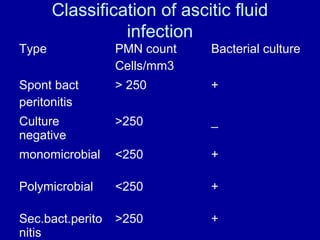
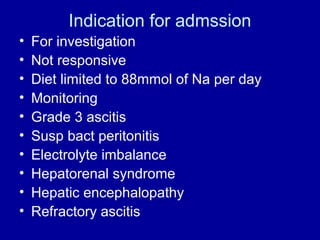
- Diagnosis involves physical exam findings like abdominal distension. Imaging like ultrasound can identify fluid levels. Paracentesis analyzes fluid for causes like spontaneous bacterial peritonitis.
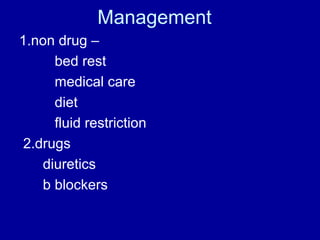
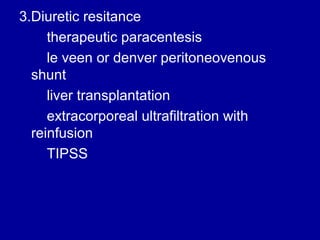
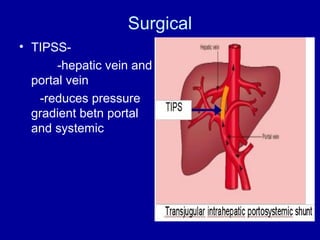
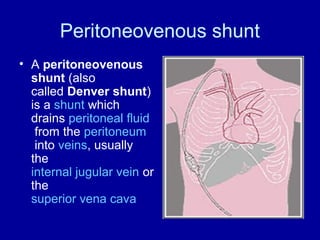
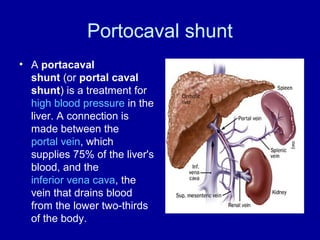
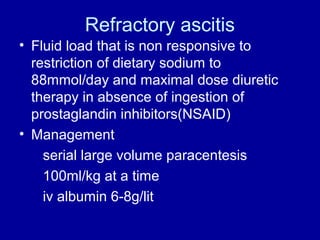
- Treatment depends on the underlying cause but may include dietary sodium restriction, diuretics, large volume paracentesis, TIPSS procedure to lower pressure, or liver transplantation for cirrhosis. Refractory ascites requires more aggressive management.