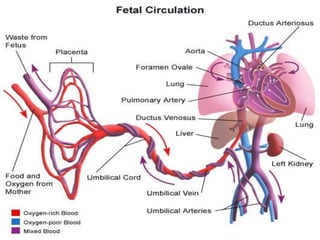
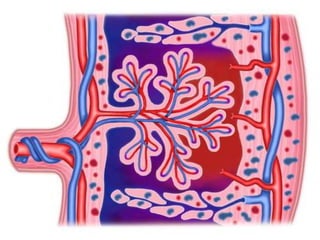
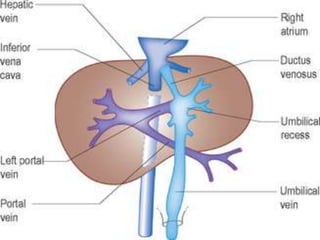
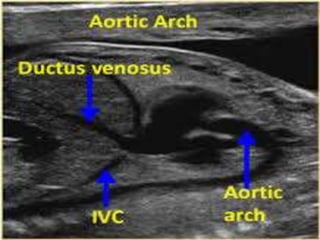
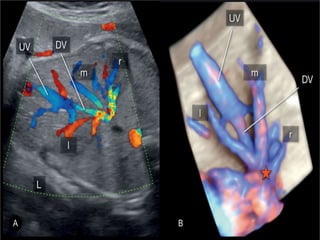
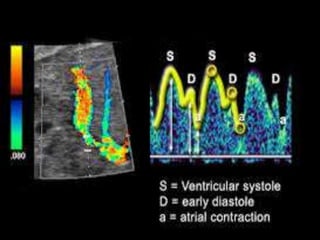
1. The ductus venosus is a blood vessel that shunts oxygenated blood from the umbilical vein directly into the inferior vena cava, bypassing the liver.
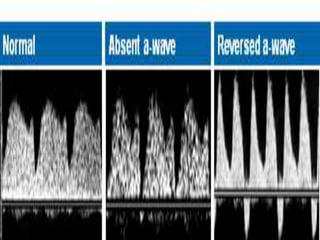
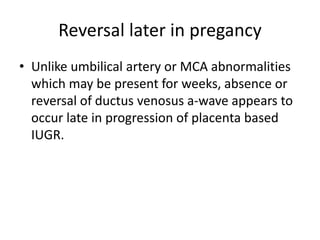
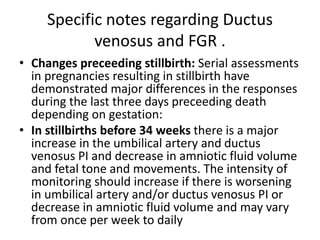
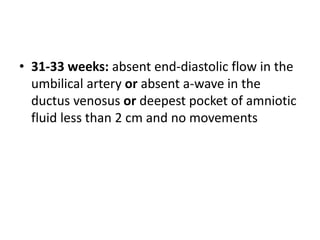
2. Abnormalities in the ductus venosus blood flow waveform, such as reversal of the a-wave, have been associated with fetal growth restriction and adverse pregnancy outcomes like stillbirth.
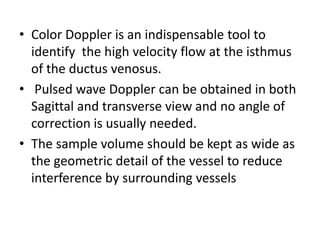
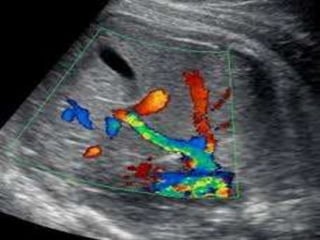
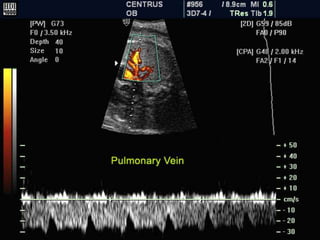
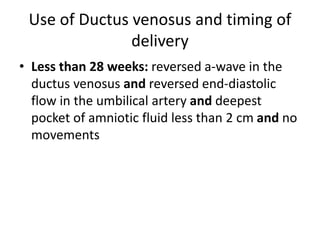
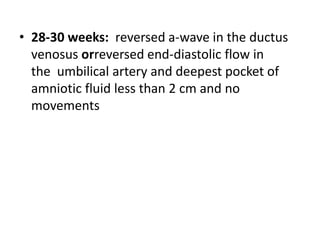
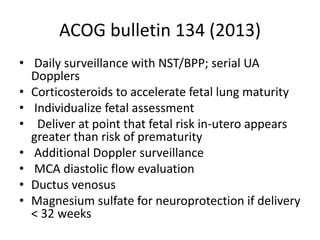
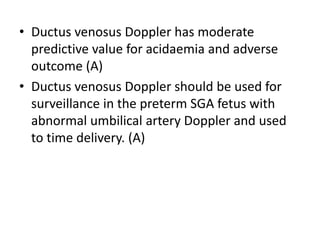
3. Monitoring ductus venosus blood flow using Doppler ultrasound is useful for assessing fetal well-being and timing of delivery in high-risk pregnancies complicated by fetal growth restriction.