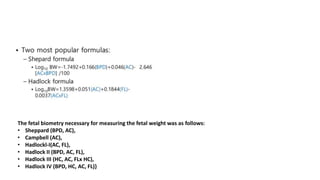
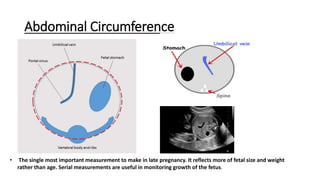
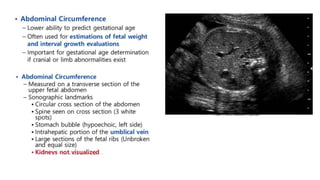
Fetal biometry parameters are ultrasound measurements used to indirectly assess fetal growth and well-being, including biparietal diameter, head circumference, abdominal circumference, and femoral length. These measurements are used in formulas to estimate gestational age and fetal weight. Intrauterine growth restriction is defined as a birth weight below the 10th percentile for gestational age and can be symmetrical, affecting overall growth, or asymmetrical, primarily impacting abdominal growth. Ultrasound biometry, particularly abdominal circumference, allows accurate prenatal diagnosis of growth issues.




![• Formulas that use measurements of the fetal head, abdomen, and
femur have a mean error of 15% (±2 standard deviations [SDs]).
• Formulas that use fewer than three measurements of fetal body
parts perform less well(i.e.,have larger standard deviations).
• Adding other measurements to the head, abdomen, and femur, such
as the thigh circumference or thickness of thigh soft tissue or
three-dimensional volume calculations, does not improve accuracy of weight estimation.
• Despite considerable improvements in sonographic equipment, the
accuracy of estimating fetal weight has not changed since the development of formulas 3 decades
ago.](https://image.slidesharecdn.com/fetalbiometryparameterslk-210514145206/85/Fetal-biometry-parameters-lk-43-320.jpg)