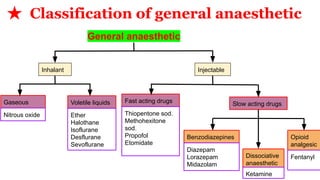
The document provides an overview of general anesthetics, including their definition, classification, mode of action, stages of anesthesia, and various drugs used. It highlights the characteristics of general anesthetics, such as inducing unconsciousness and muscle relaxation, while detailing specific drugs, their uses, contraindications, dosages, and potential adverse effects. Key examples include inhalational anesthetics like halothane and nitrous oxide, and intravenous options like thiopental sodium.