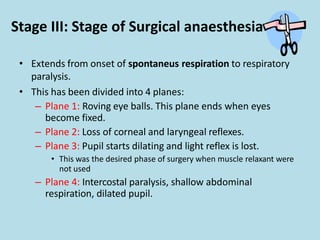
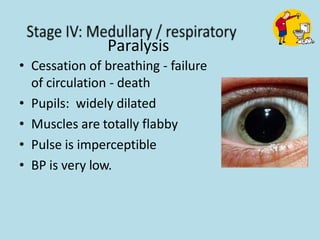
General anaesthesia involves drugs that cause reversible loss of sensation and consciousness. Common general anaesthetics include inhalation gases like nitrous oxide, volatile liquids like halothane and isoflurane, and intravenous drugs like thiopentone, propofol, and ketamine. Anaesthesia involves stages including loss of consciousness, excitement, and surgical anaesthesia. Complications can occur during or after anaesthesia involving respiratory, cardiac, or organ issues. Pre-anaesthetic medication is used to relieve anxiety, cause amnesia, decrease secretions, and provide analgesia and antiemetic effects to make anaesthesia safer.