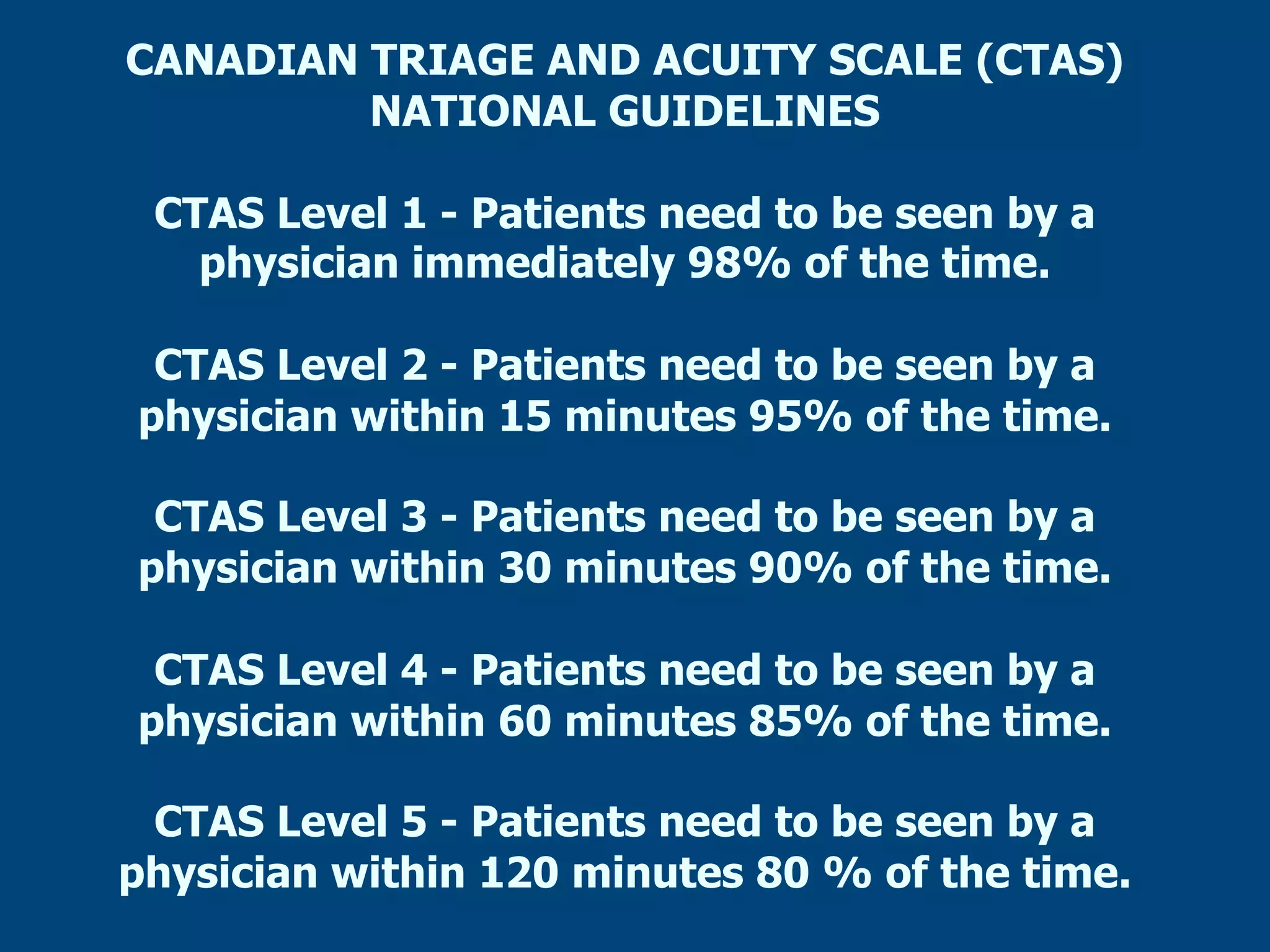
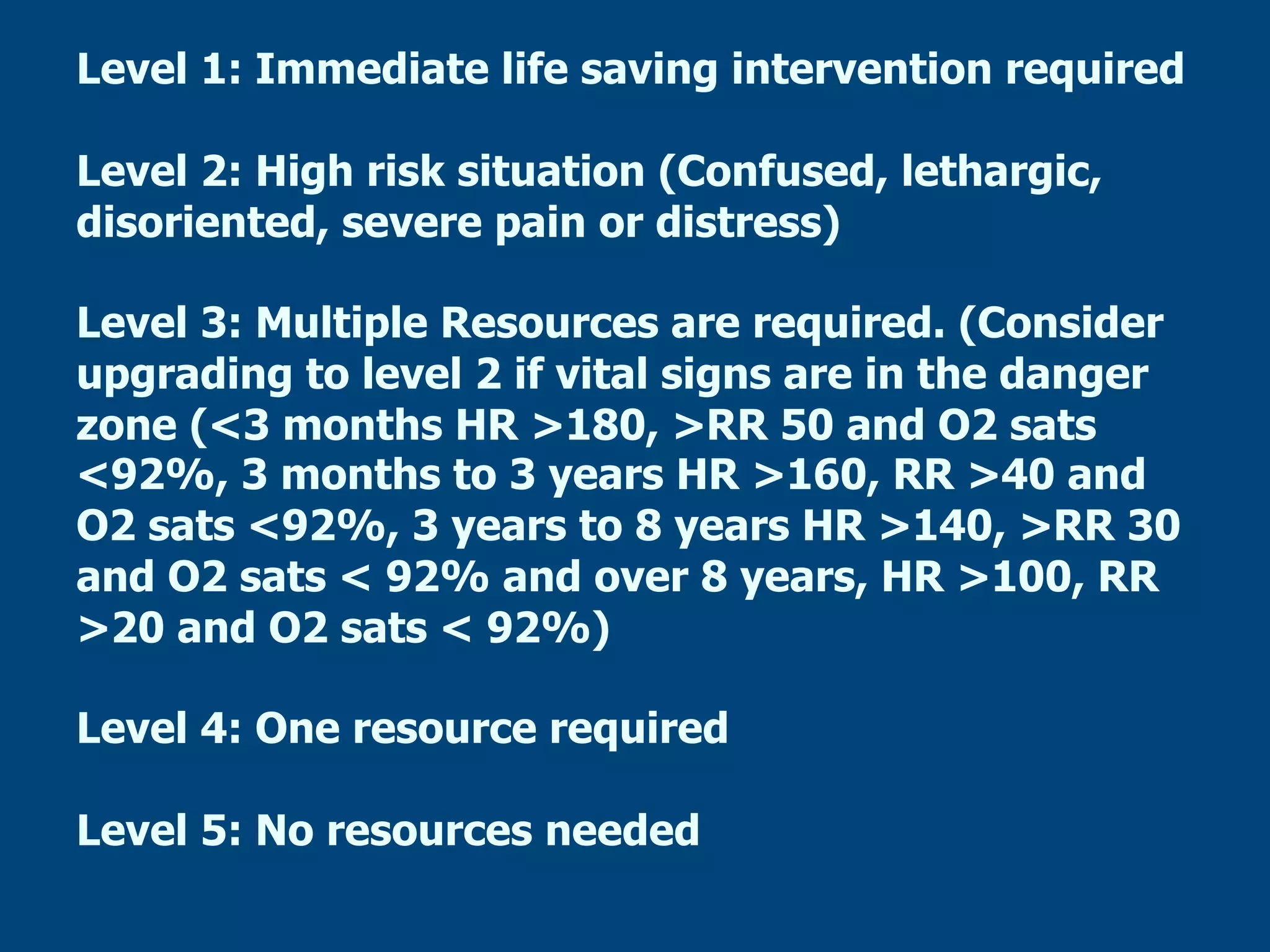
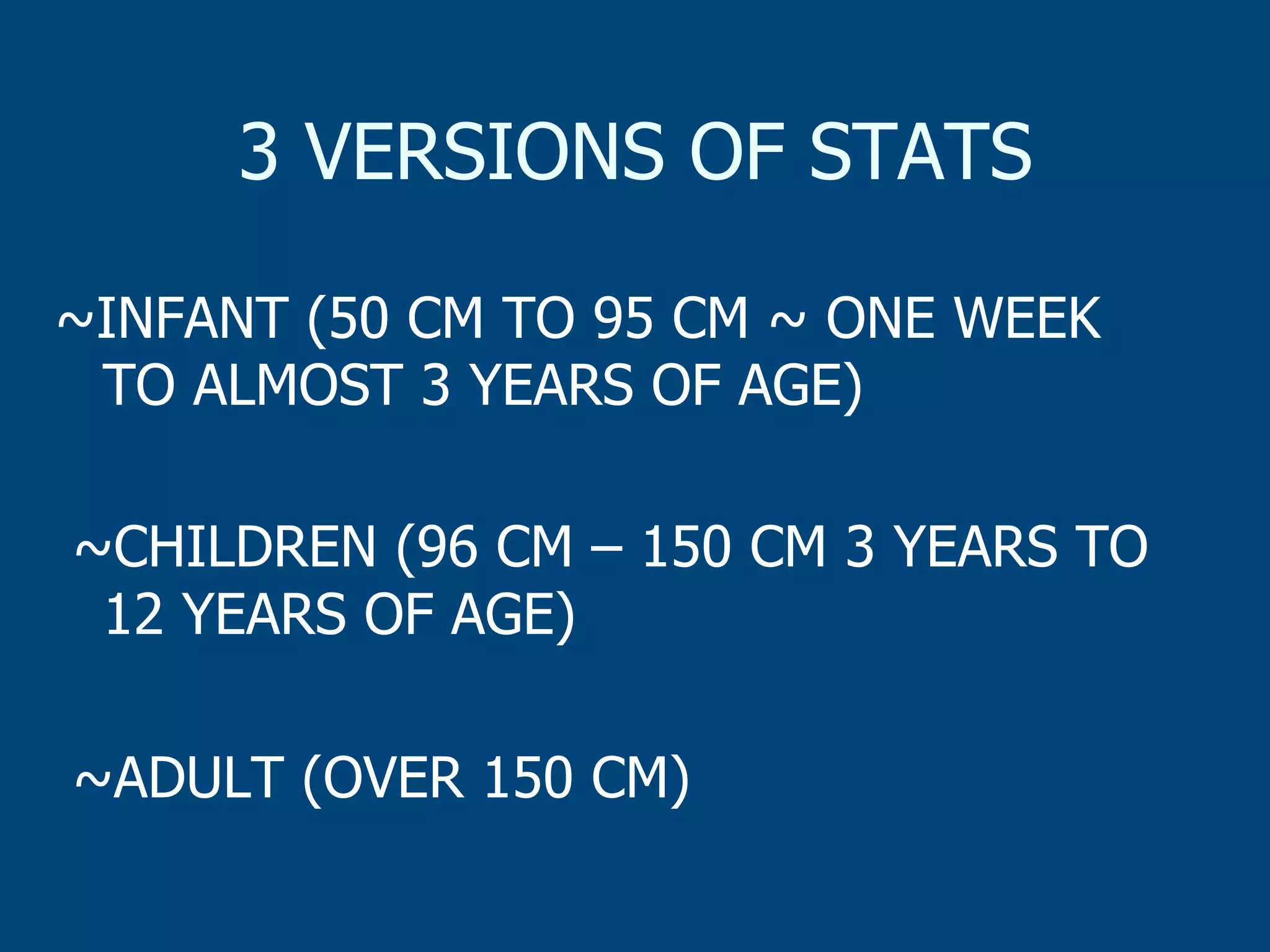
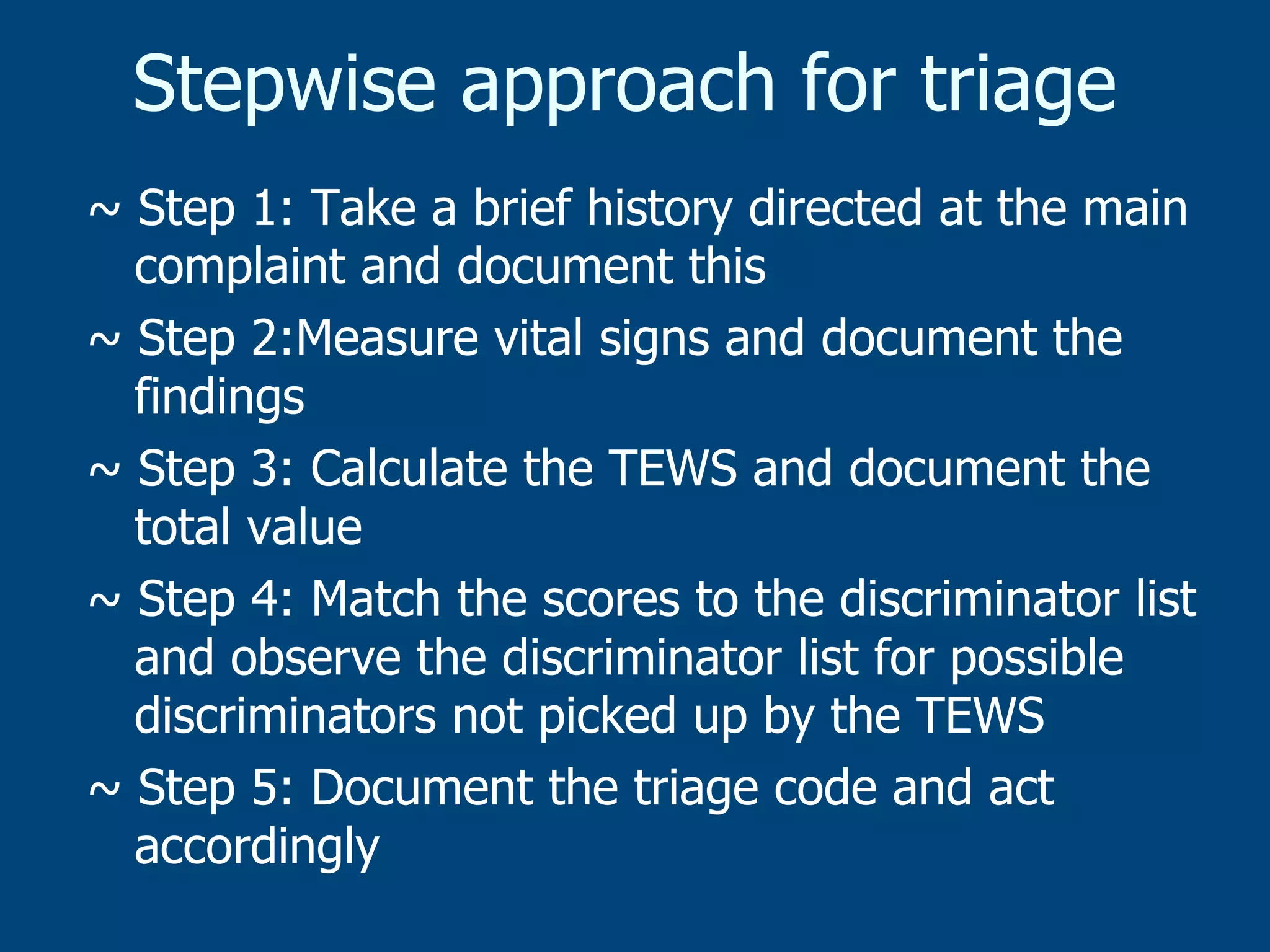
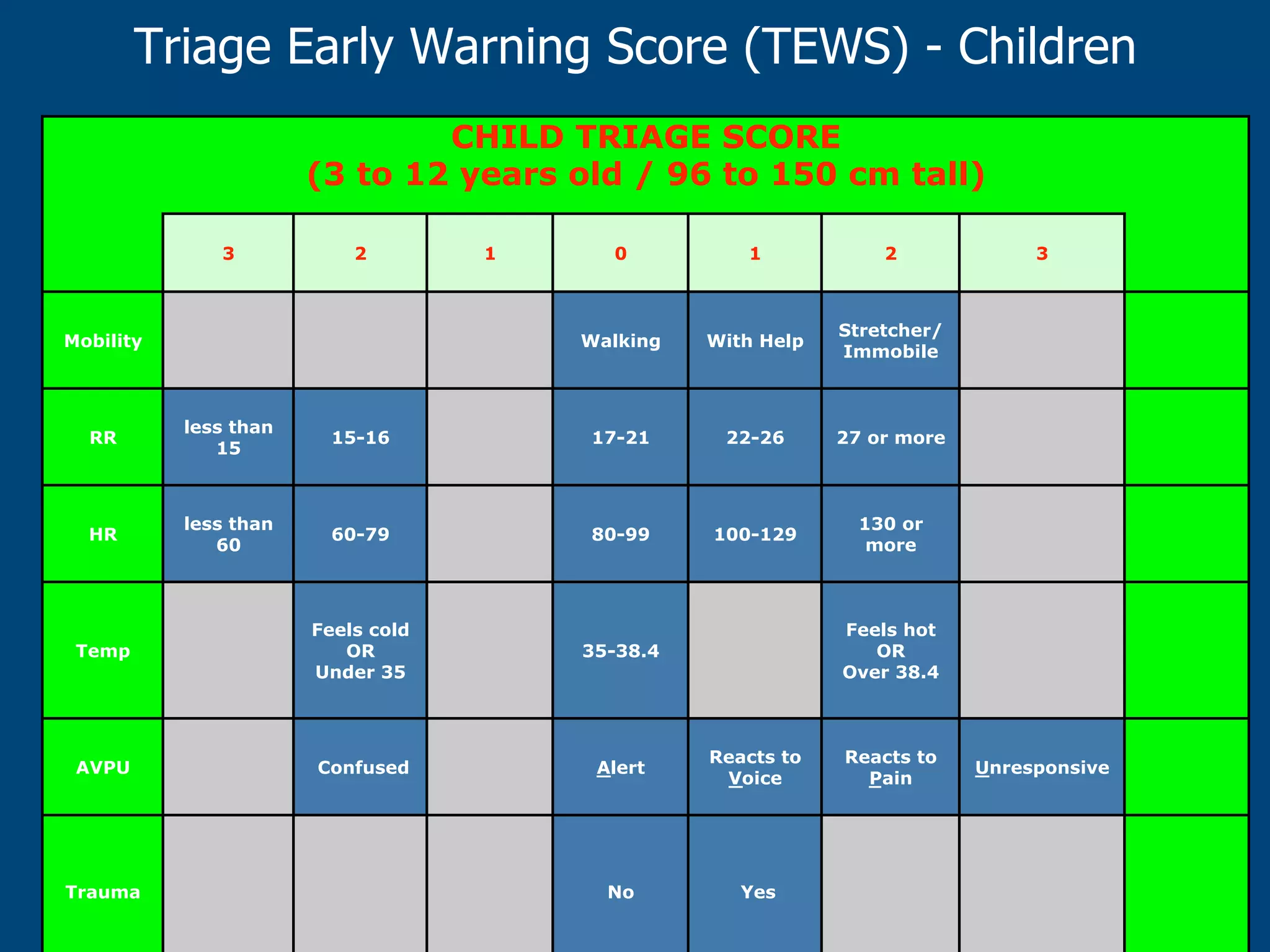
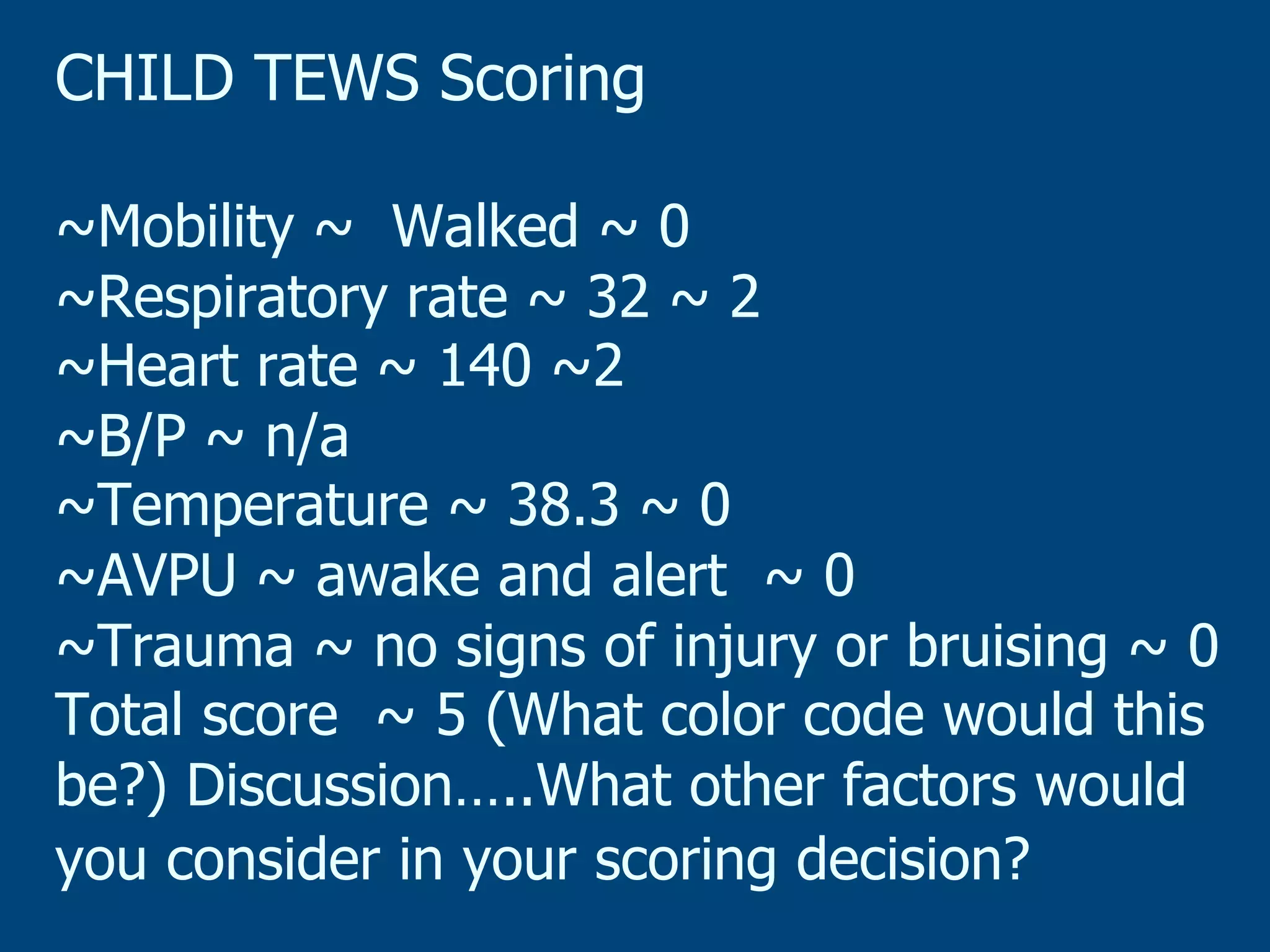
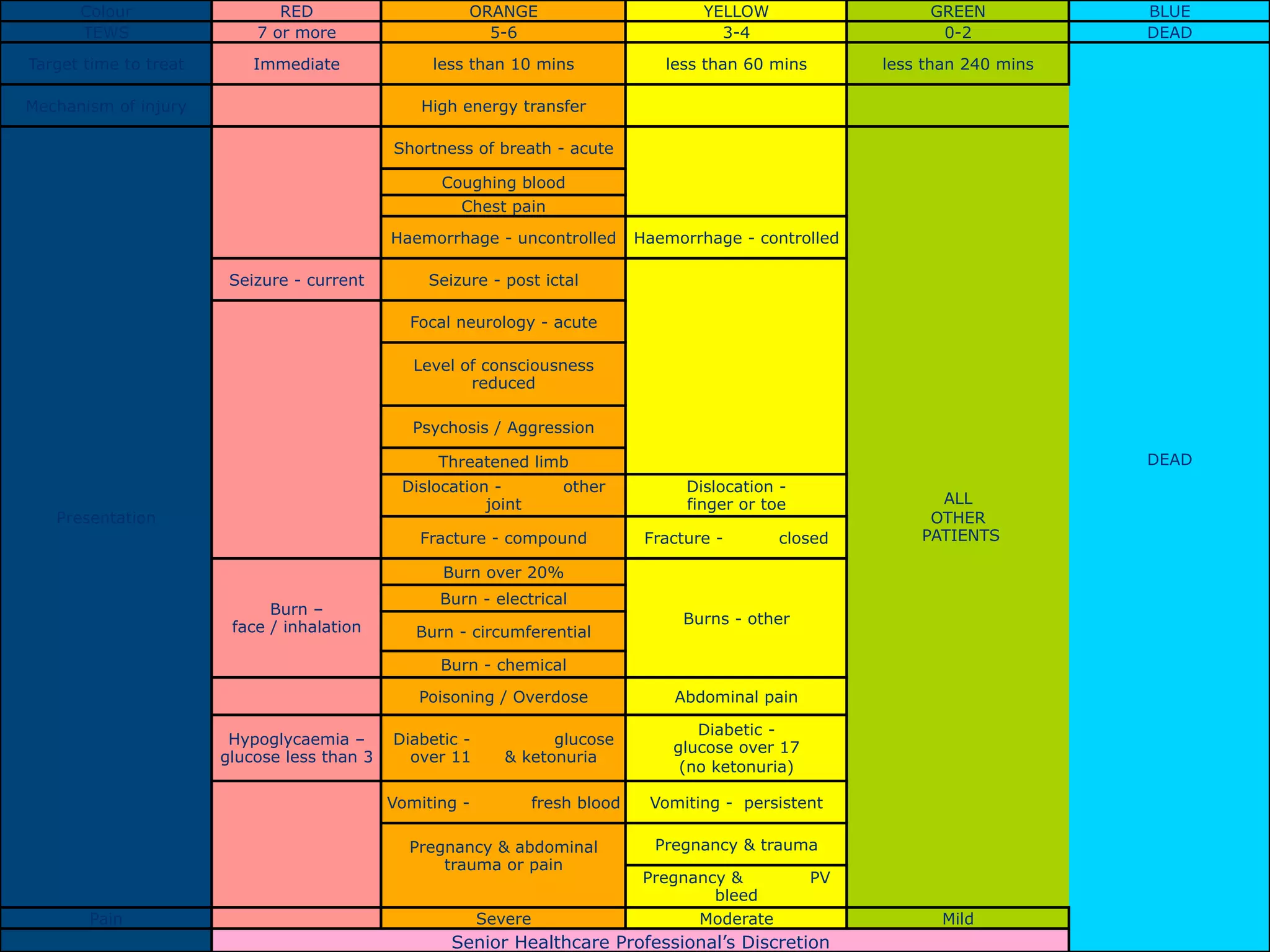
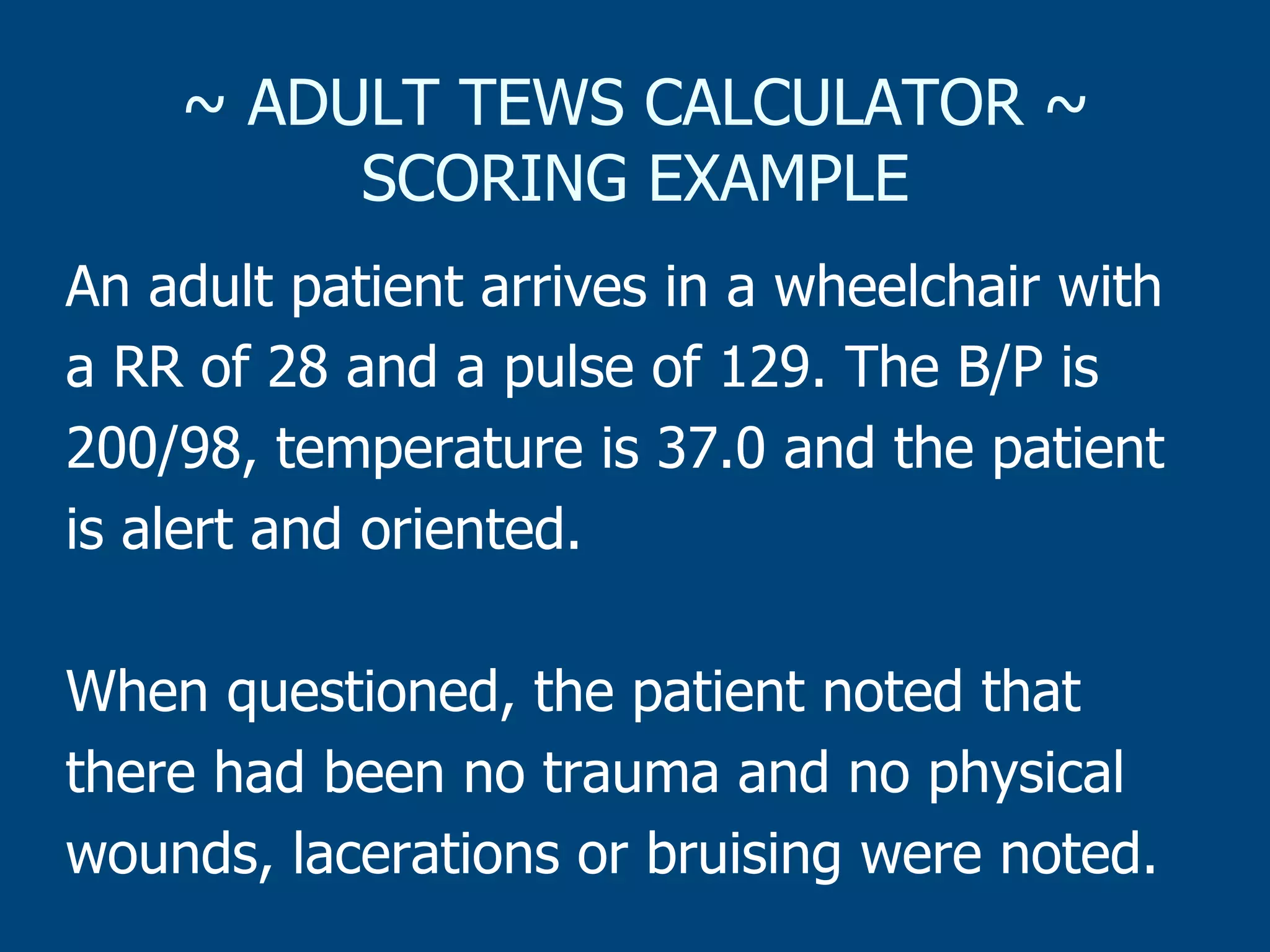
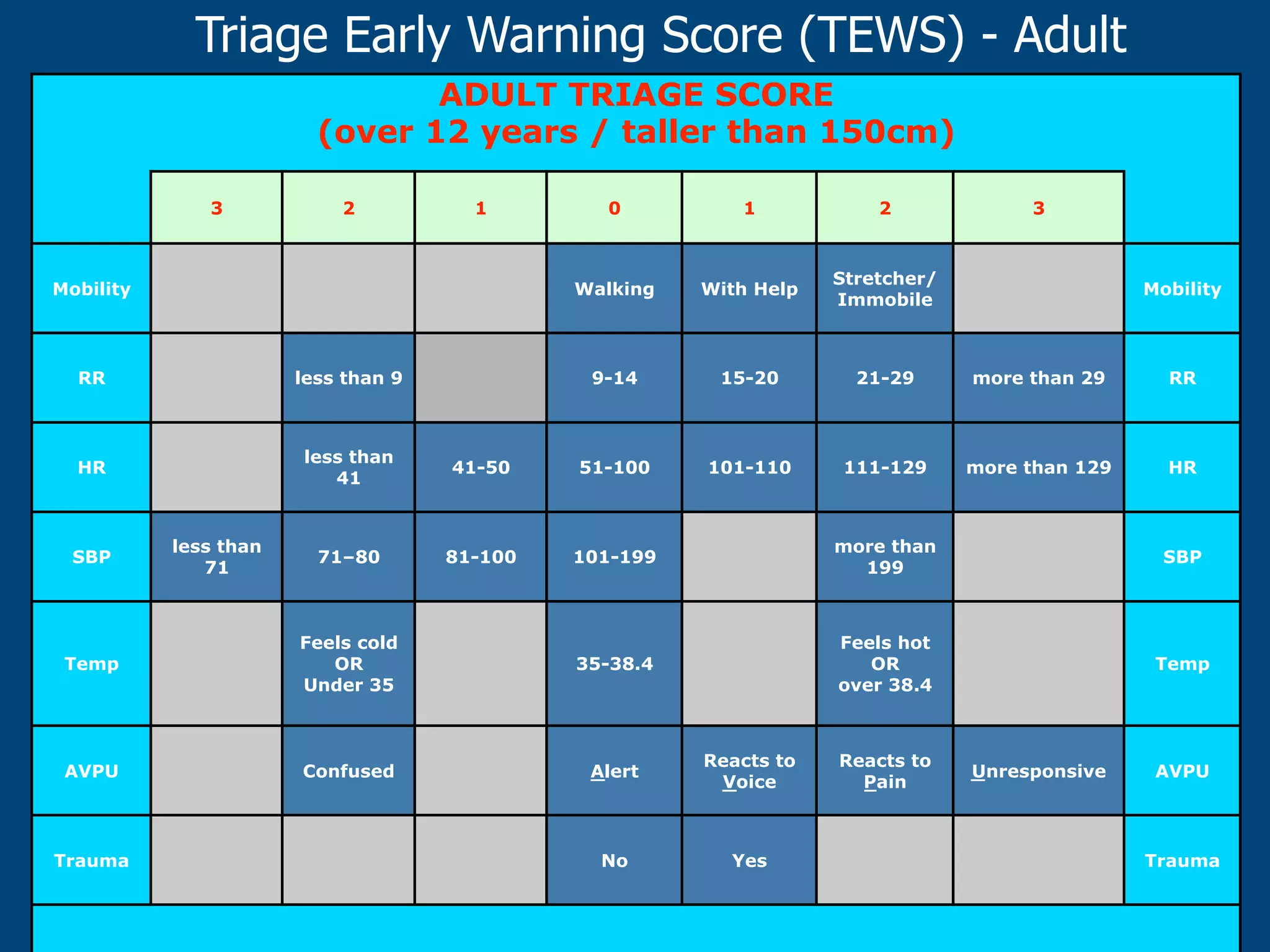
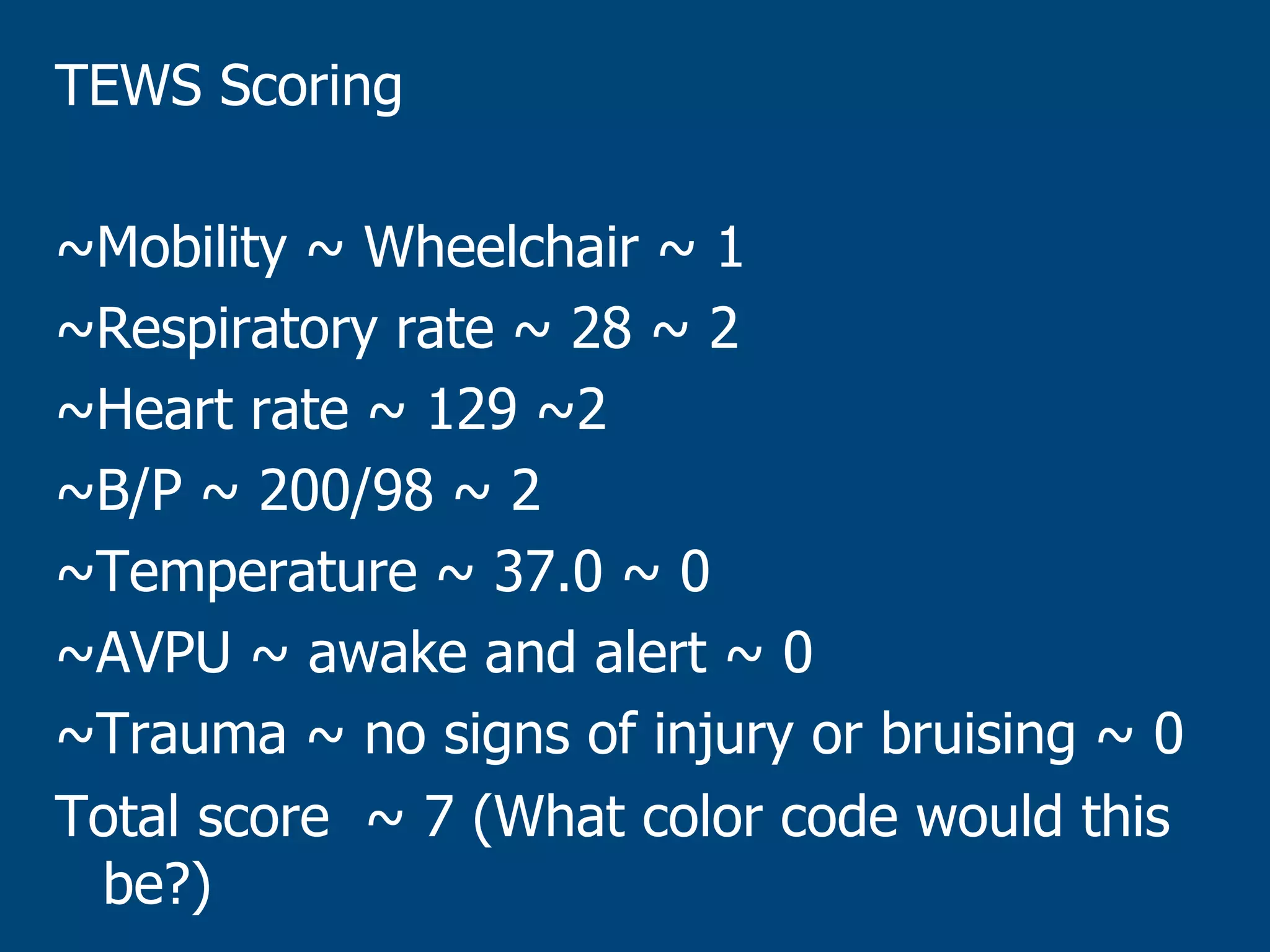
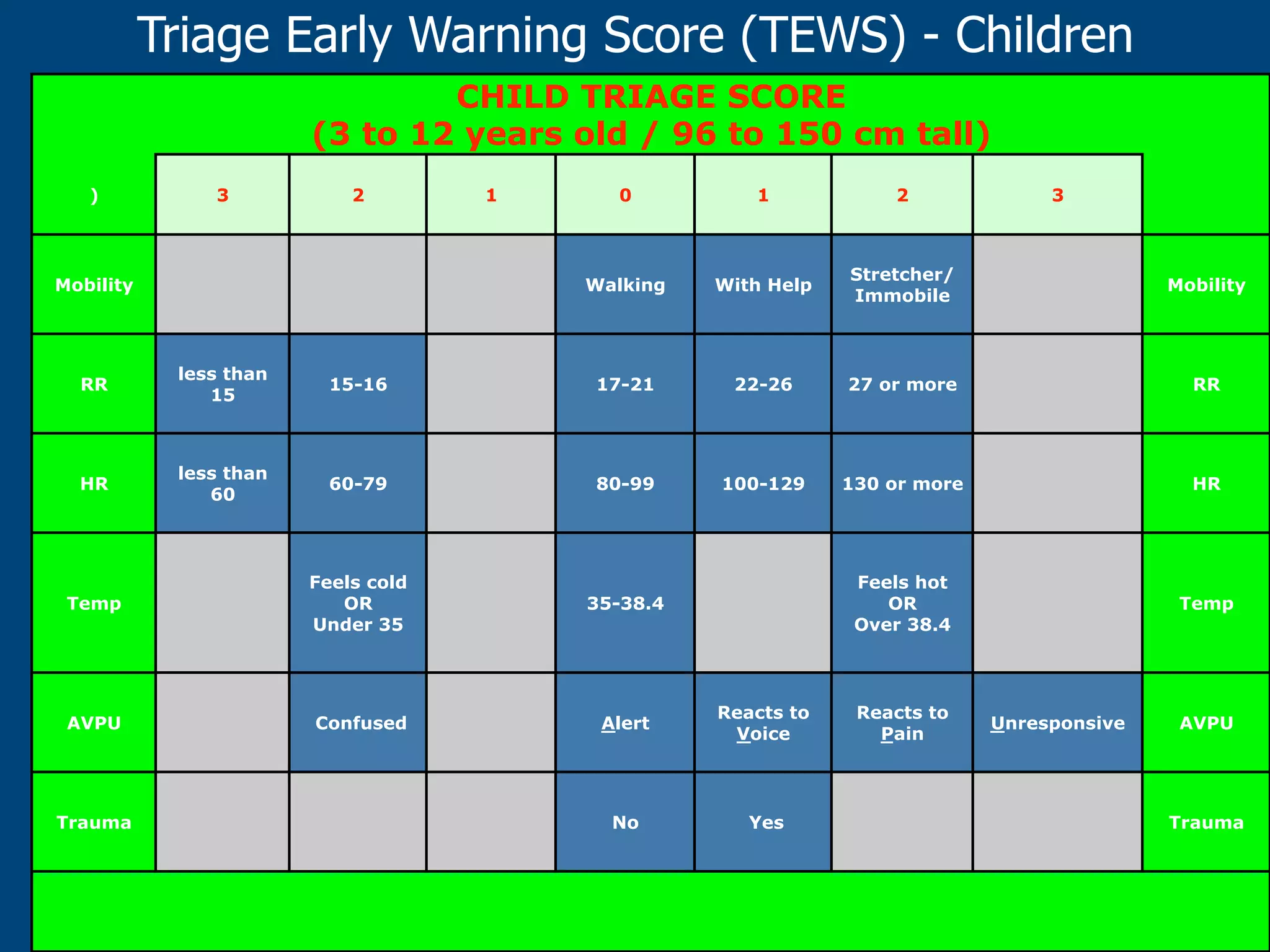
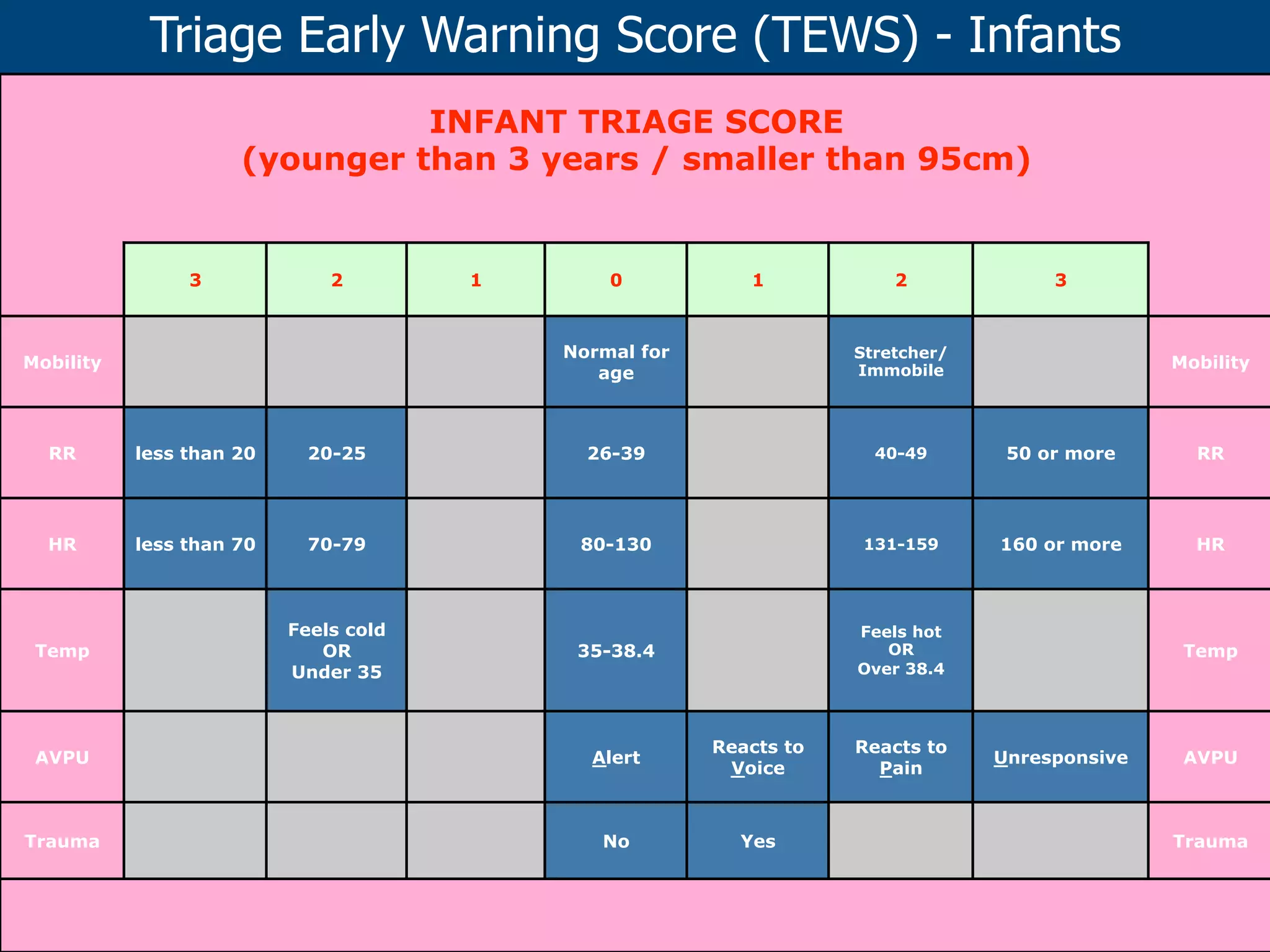
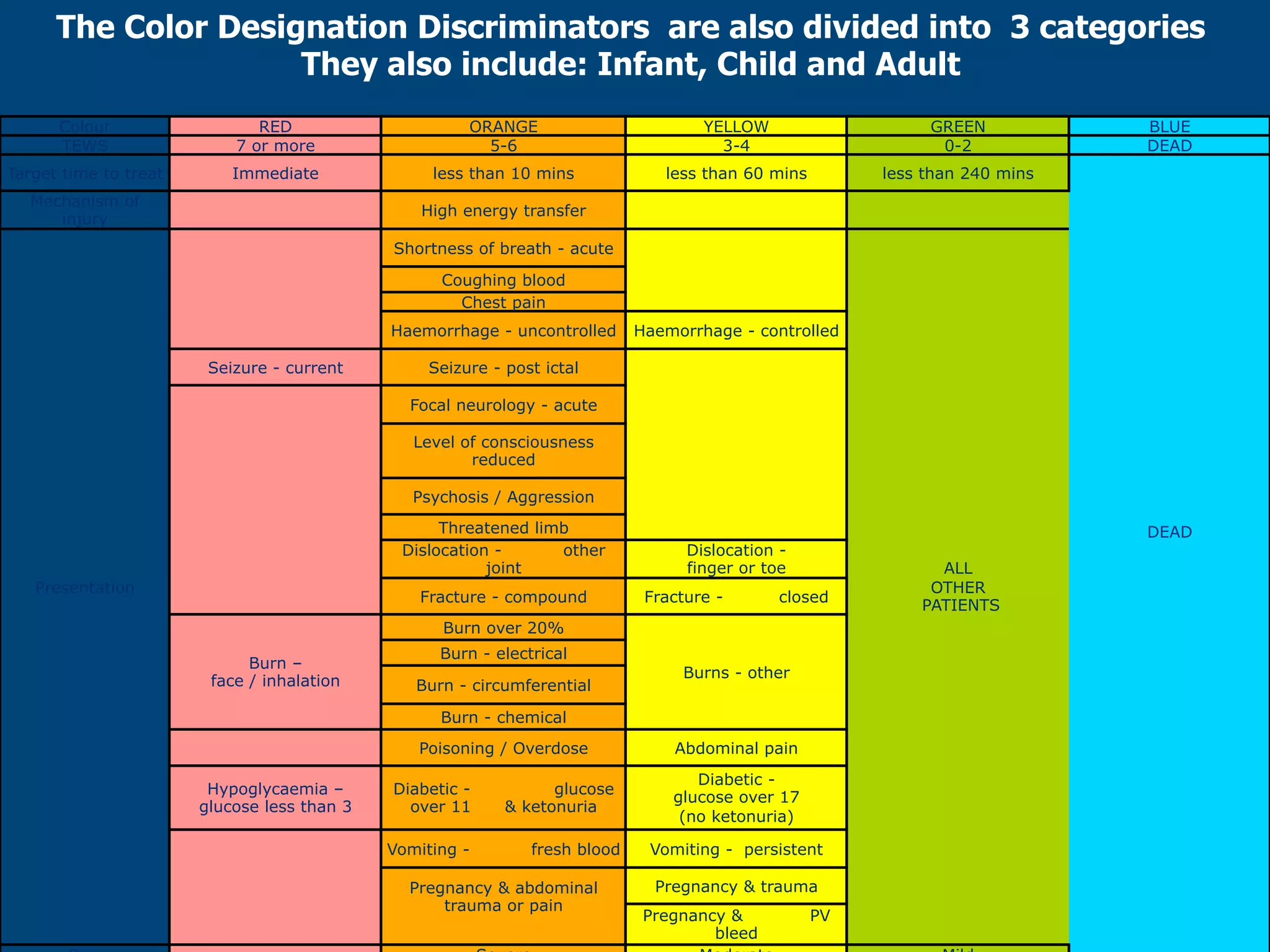
The document outlines triage in emergency nursing, defining its purpose as determining patient treatment priorities based on condition severity. It discusses the roles and qualifications of triage nurses, various triage systems like the Cape Triage Score, and includes details on assessment methods and decision-making processes. Additionally, it emphasizes the importance of skill development through practice to enhance triage efficiency in emergency care settings.