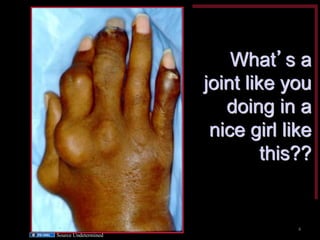
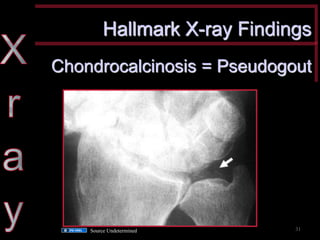
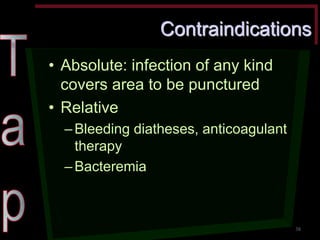
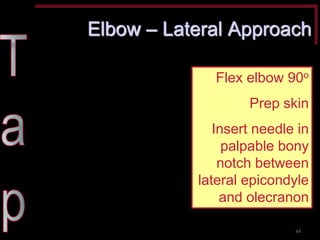
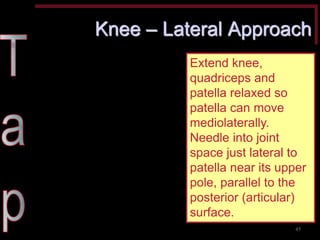
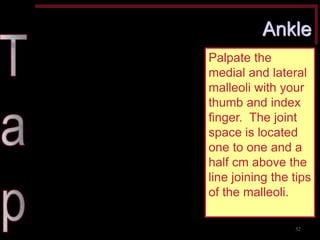
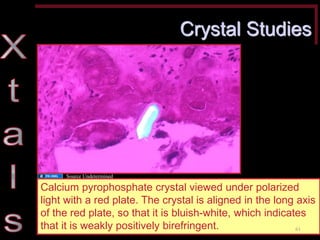
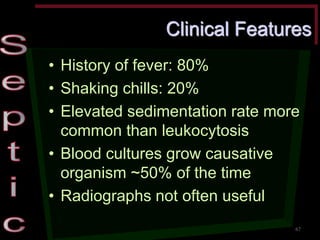
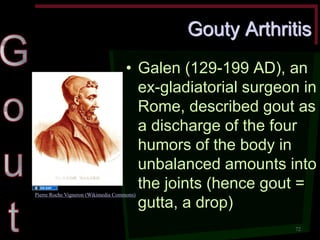
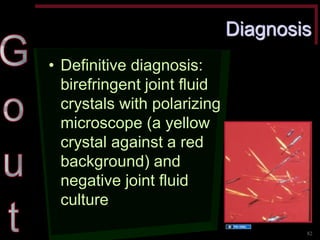
This document discusses arthritis and arthrocentesis, outlining the types of joints, arthritis pathophysiology, and differential diagnoses based on various clinical features. It emphasizes the importance of synovial fluid studies for diagnosis and offers detailed procedures for arthrocentesis, including indications, contraindications, and techniques. Additionally, it covers gout pathophysiology, presentation, and management strategies.