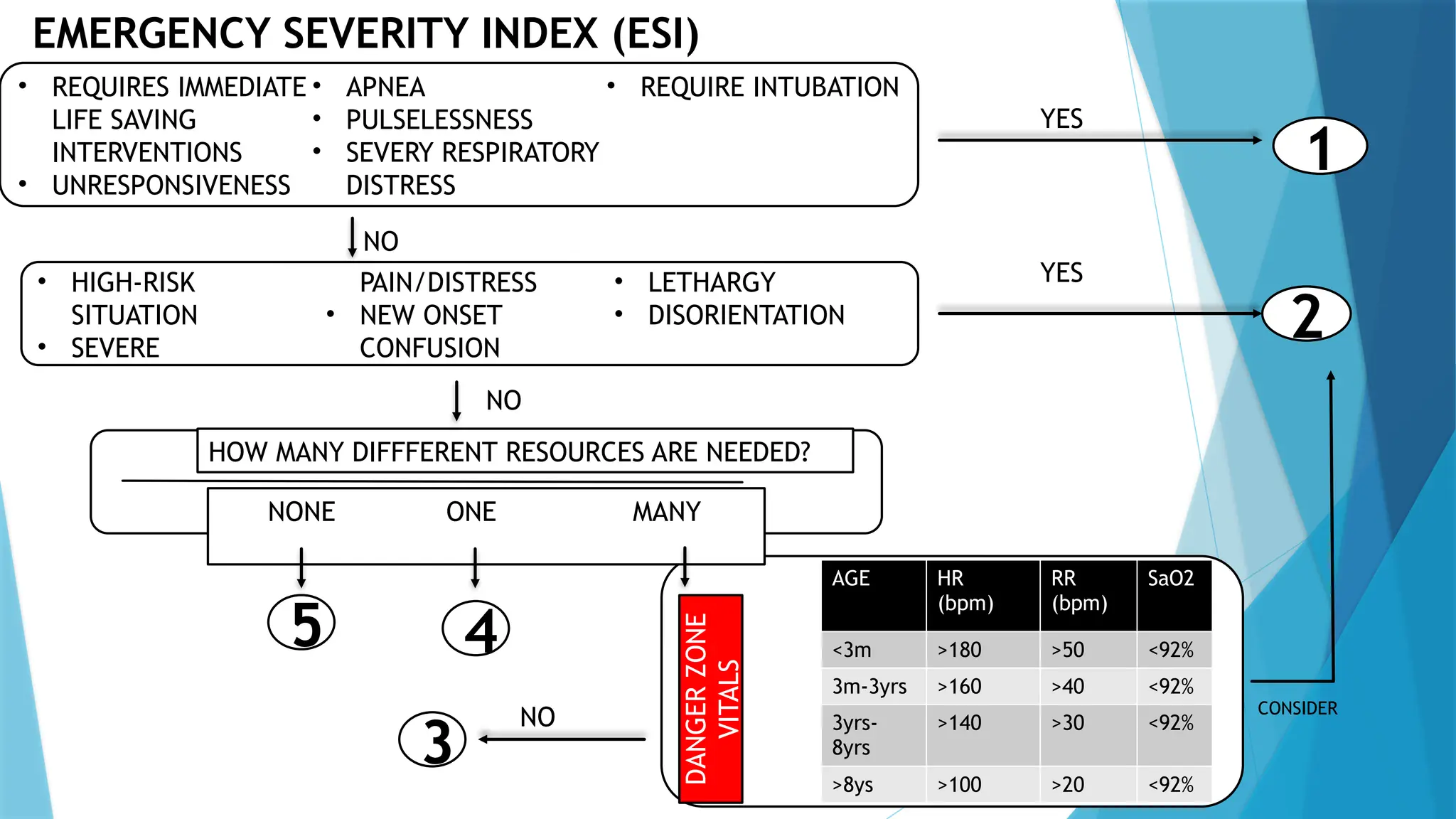
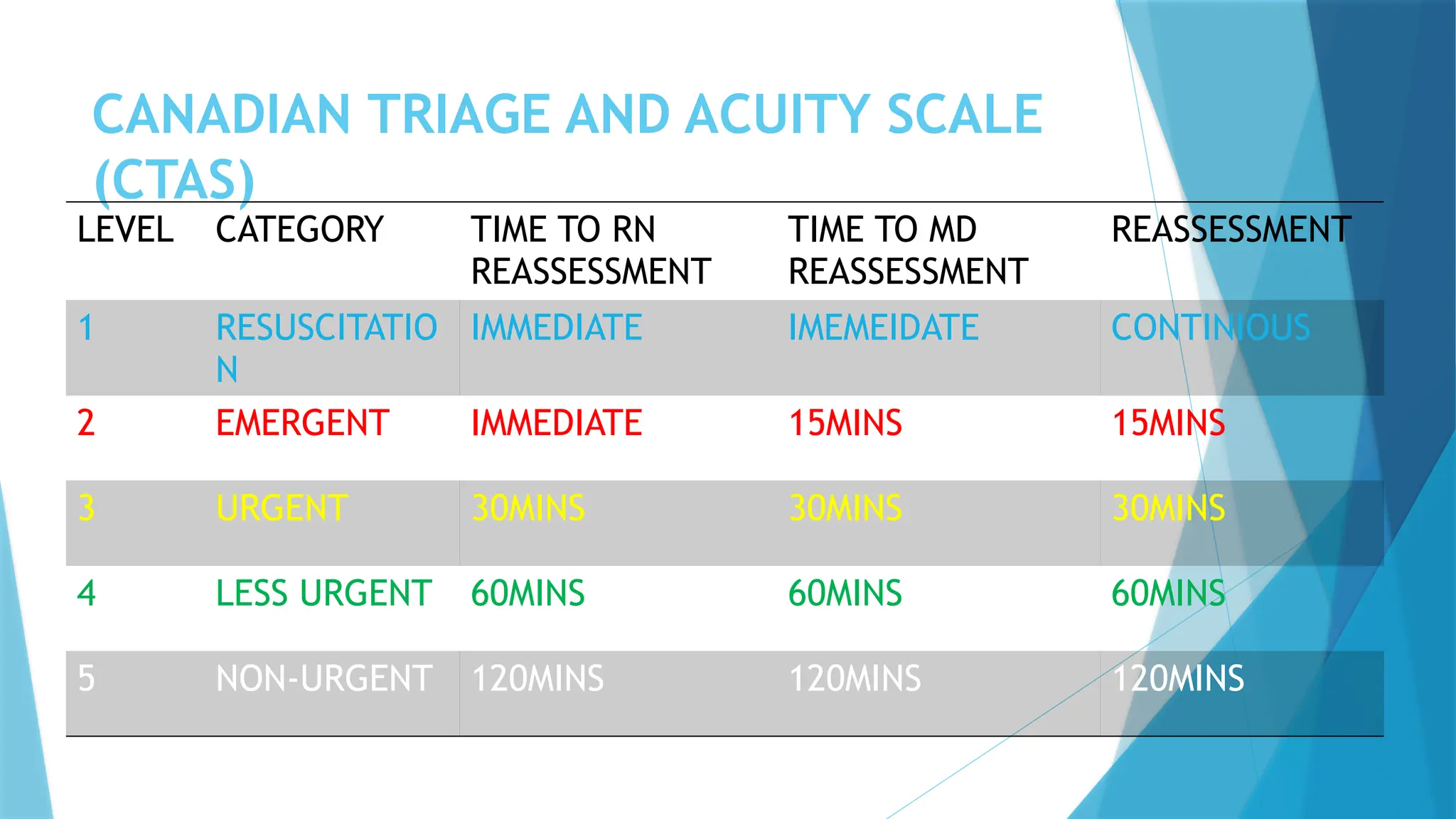
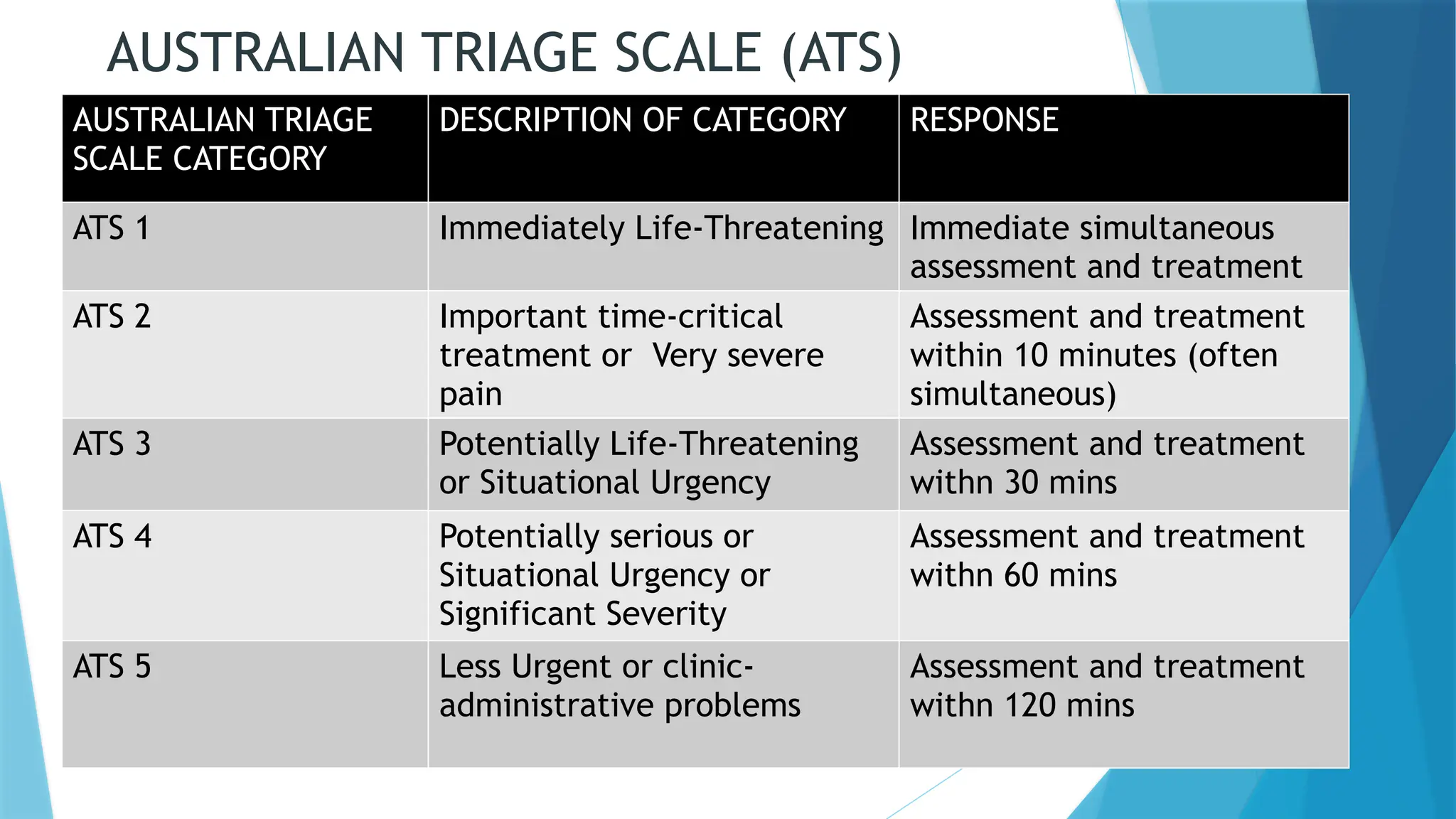
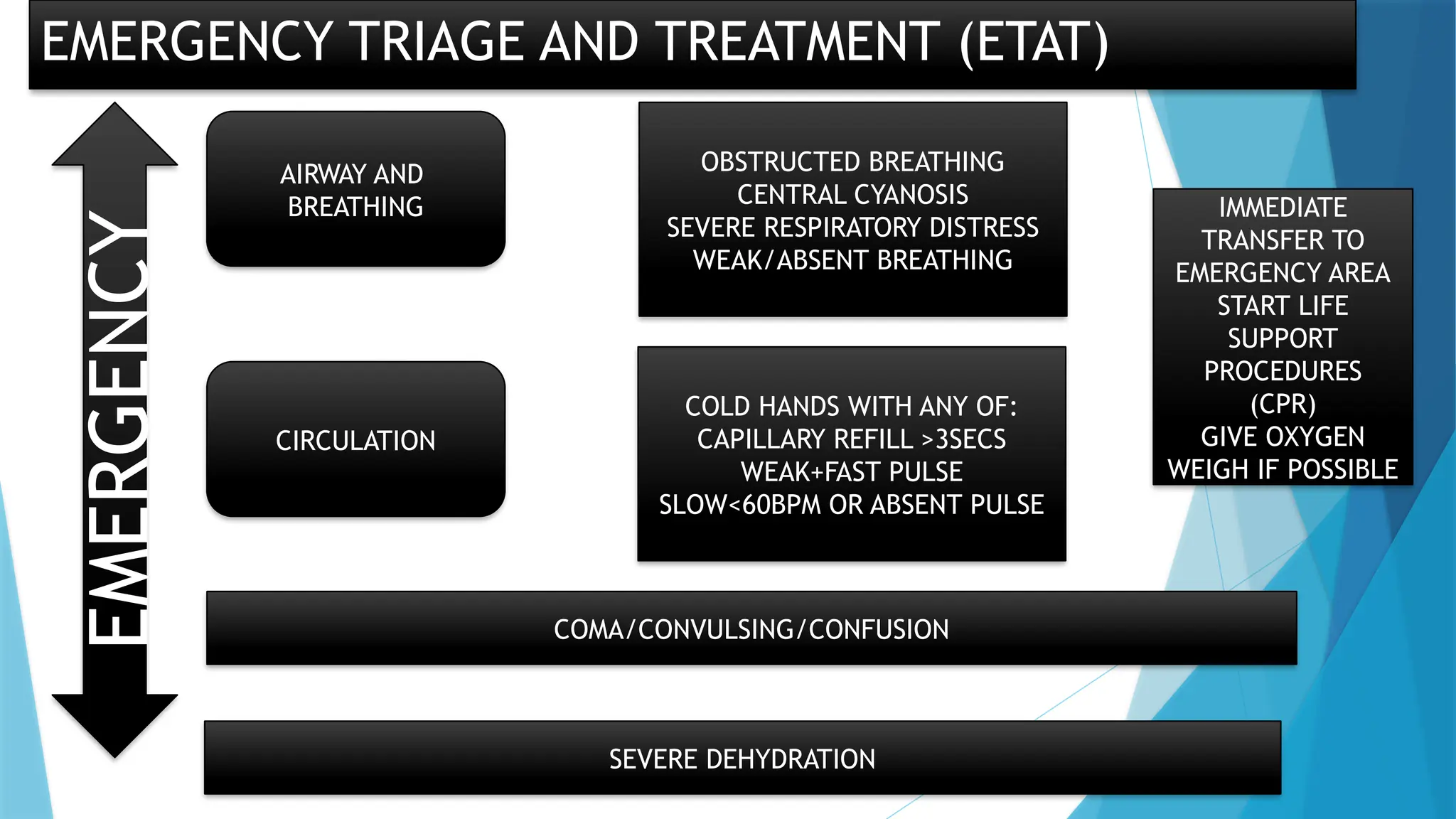
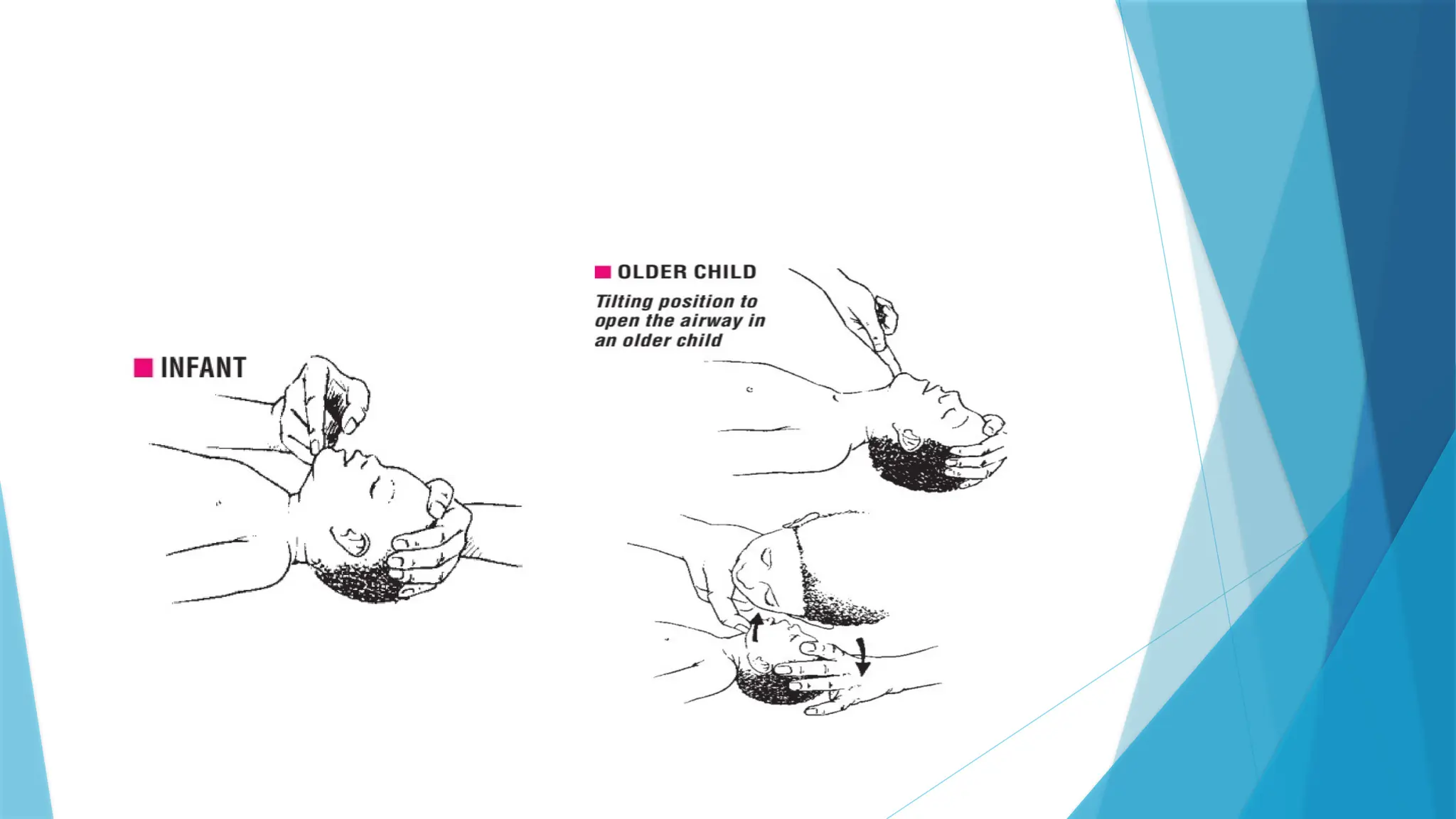
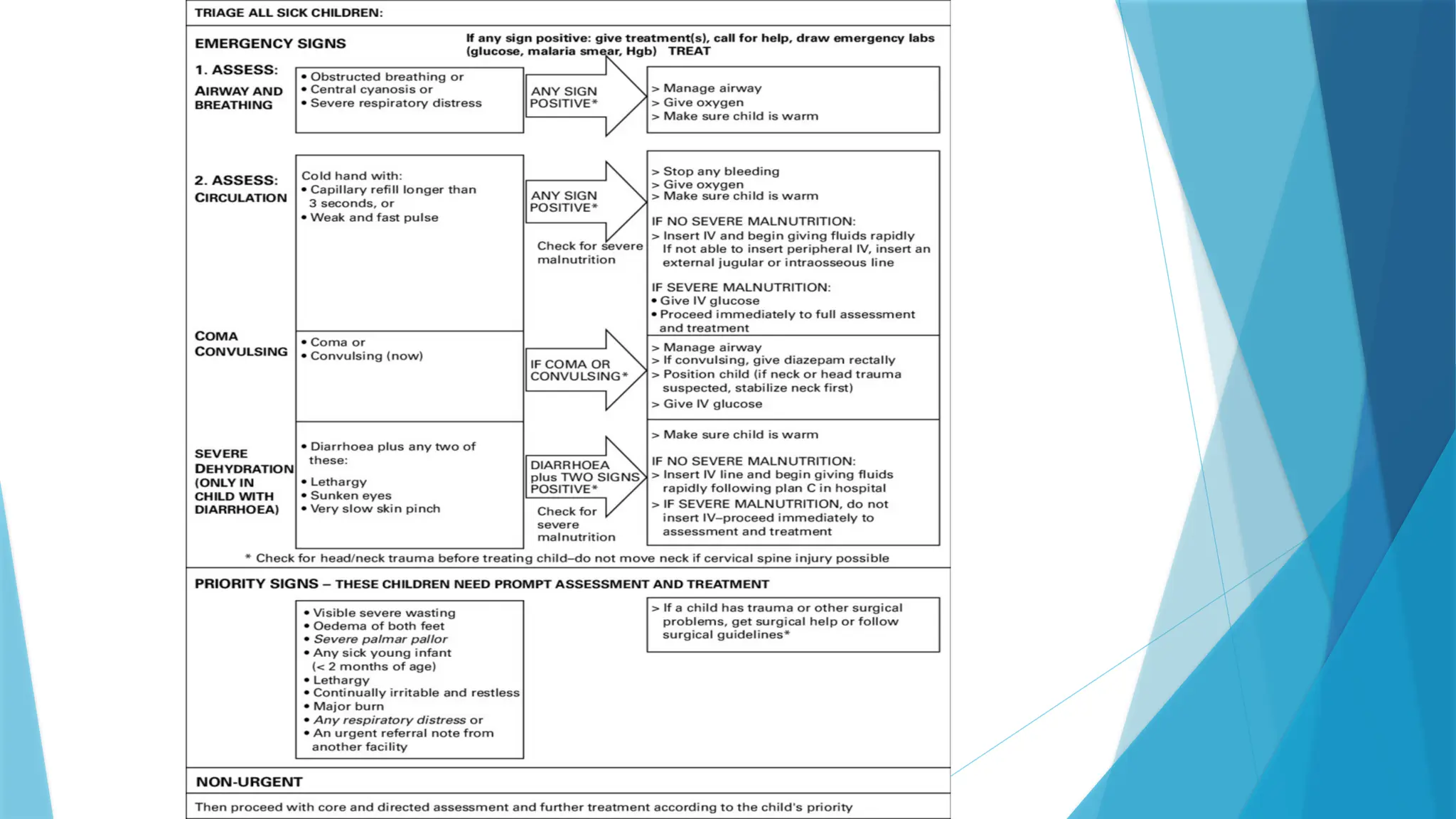
The document discusses the importance of triage in emergency settings, highlighting the need for quickly identifying and prioritizing sick children upon their arrival to prevent avoidable deaths. It elaborates on different triage systems, assessment processes, and the challenges faced in implementing these systems effectively. Recommendations are provided to improve triage practices in healthcare facilities, emphasizing staff training, proper equipment, and efficient record-keeping.