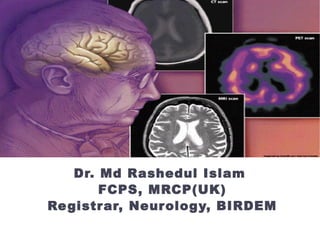
A 60-year old diabetic male presented with progressive walking difficulty over 1 year and slurred speech for 10 months. Examination found masked face, mild cognitive impairment, spastic dysarthria, vertical gaze palsy, and unstable broad-based gait. MRI showed atrophy of the dorsal midbrain. He was diagnosed with progressive supranuclear palsy and diabetes. Treatment included medications, physiotherapy, and speech therapy, with some improvement in instability and falls over 2 months.