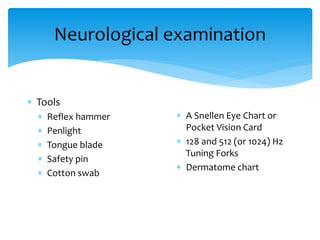
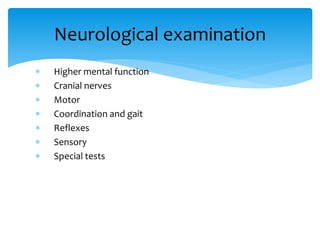
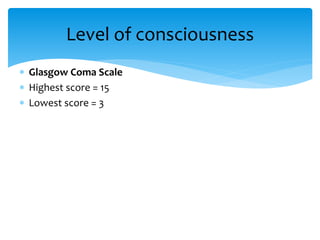
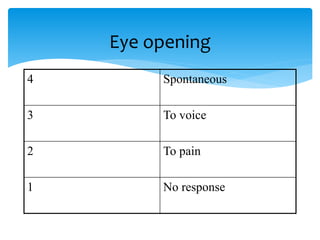
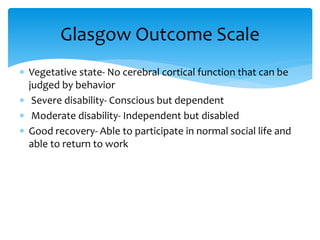
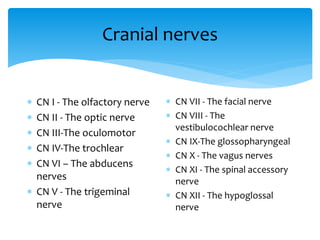
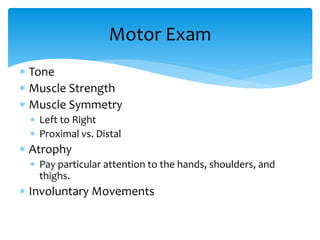
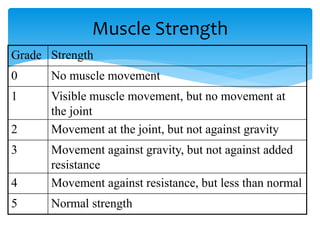
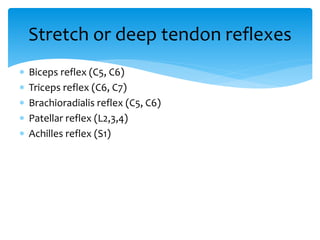
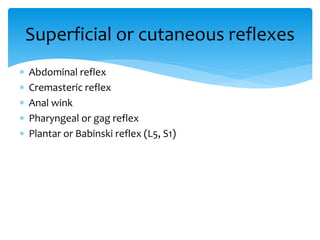
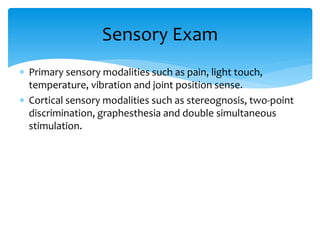
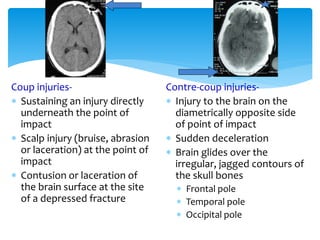
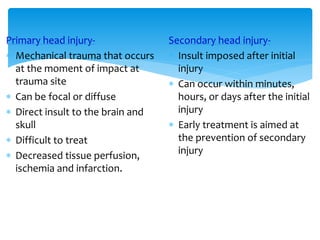
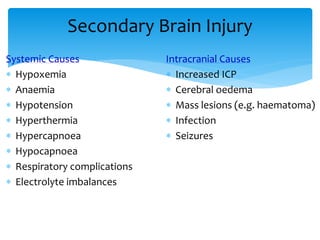
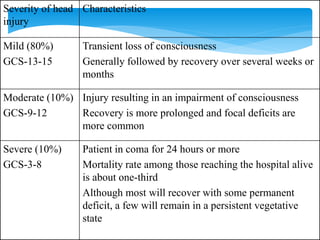
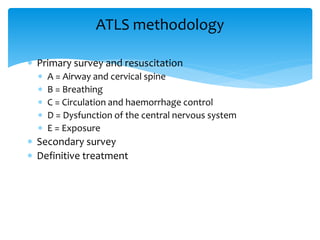
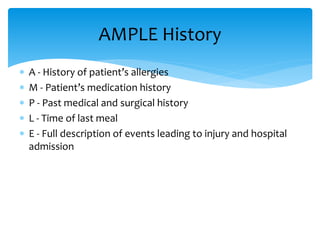
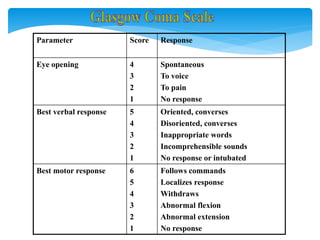
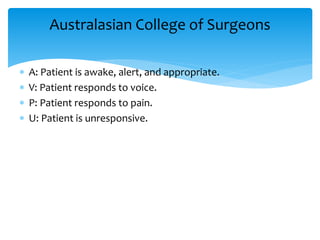
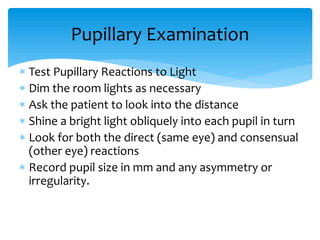
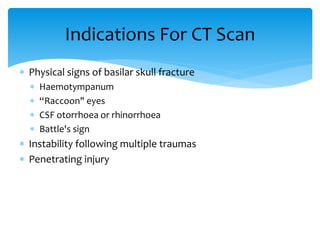
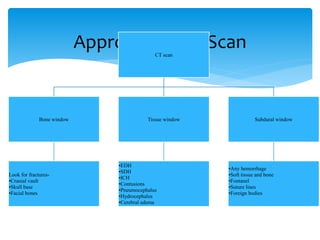
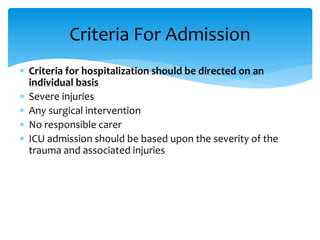
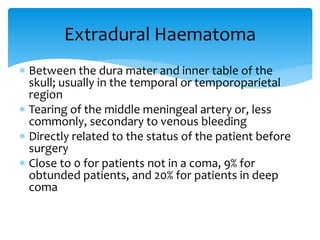
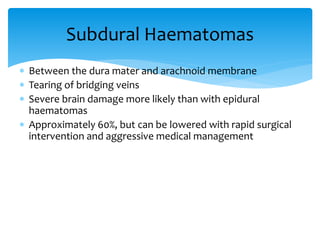
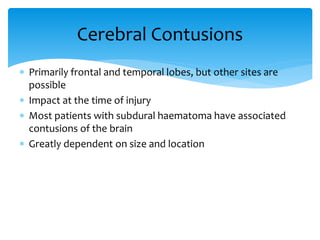
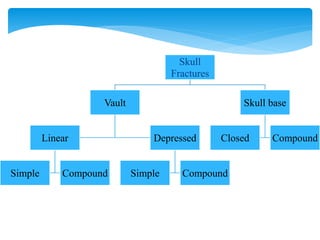
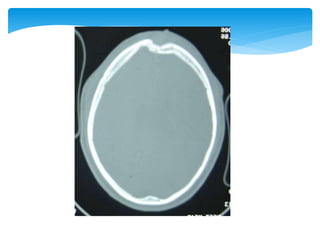
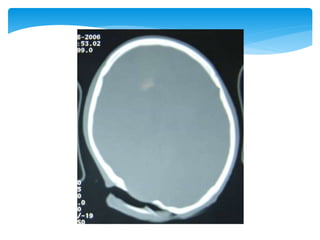
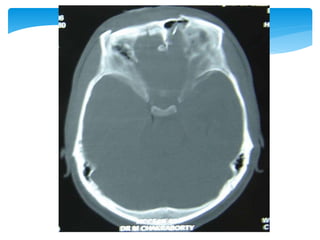
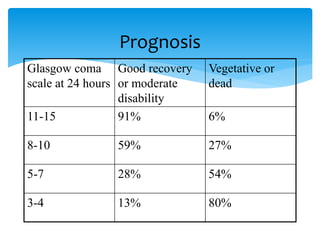
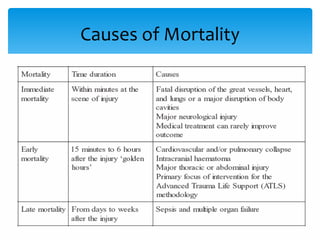
This document provides information on performing a neurological examination. It discusses taking a patient history including personal details and history of present illness. It then describes performing a physical examination including vital signs and systematic examination of body systems. The neurological exam section details assessing higher mental functions, cranial nerves, motor function, coordination, reflexes, sensation and special tests. It also discusses tools used in the exam and evaluating conditions like head injuries.