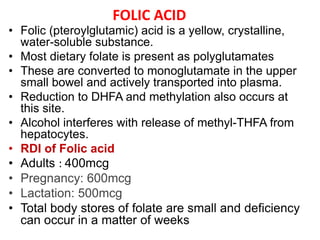
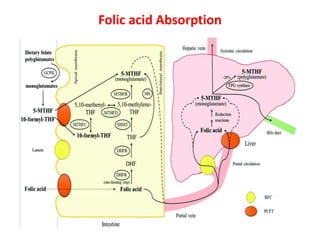
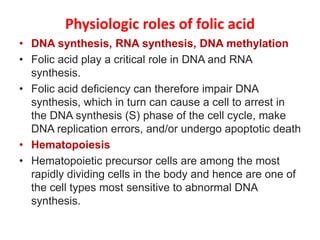
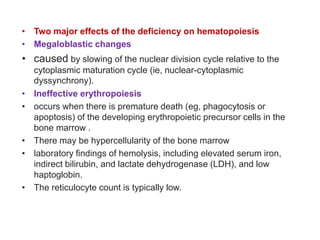
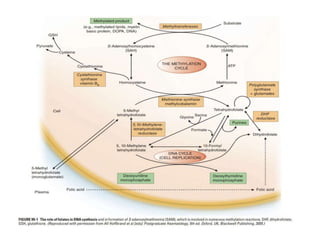
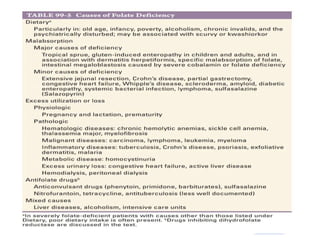
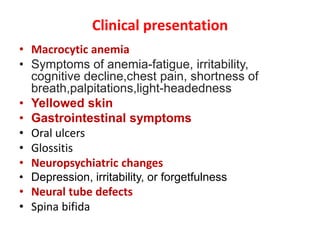
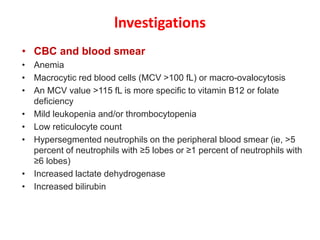
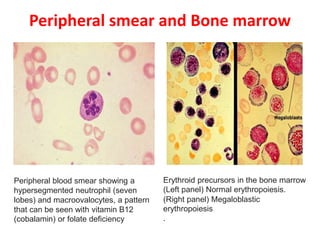
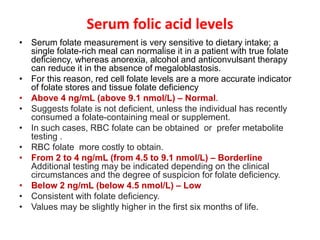
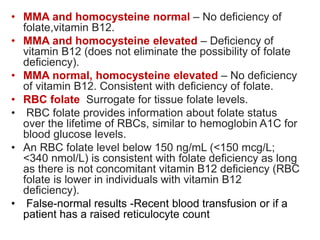
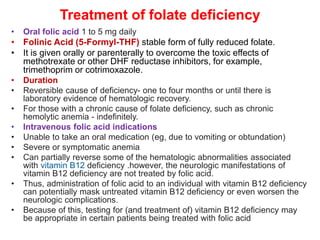
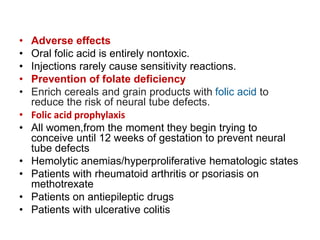
This document summarizes folic acid deficiency, including its physiologic roles, clinical presentation, investigations, treatment, and prevention. It notes that folic acid is important for DNA and RNA synthesis and hematopoiesis. Deficiency can cause macrocytic anemia and megaloblastic changes in the bone marrow. It is investigated through CBC, serum and red blood cell folate levels, and metabolites. Treatment involves oral folic acid supplementation.