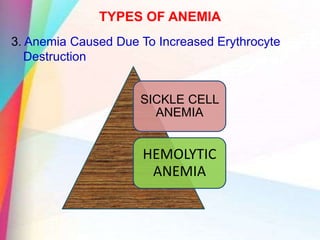
1. The document discusses various types of anemia including iron deficiency anemia, megaloblastic anemia, thalassemia, and aplastic anemia.
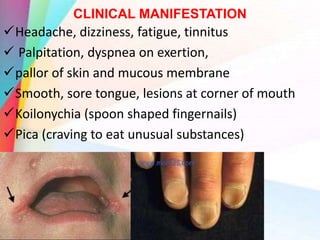
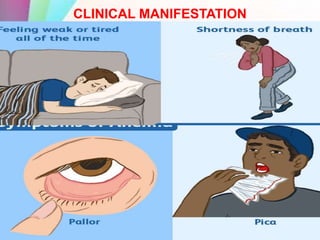
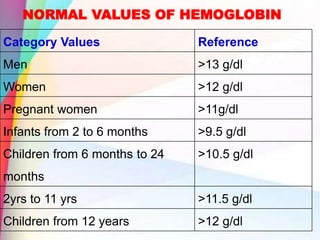
2. It provides definitions, causes, pathophysiology, clinical manifestations and management for each type.
3. The types are classified based on their etiology and morphology. Iron deficiency anemia is the most common type globally.













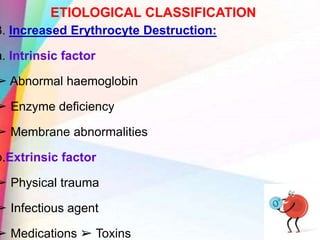
![ETIOLOGICAL CLASSIFICATION
1. Decreased erythrocyte production:
a. Decreased haemoglobin synthesis
➢ Iron deficiency
b. Defective DNA synthesis
➢ Cobalamine [ vitamin b12 ] deficiency
➢ Folic acid deficiency
c. Decreased number of erythrocyte precussors
➢ Aplastic anemia
➢ Anemia of myleoproliferative disease](https://image.slidesharecdn.com/anemia-200717043003/85/Anemia-20-320.jpg)





















































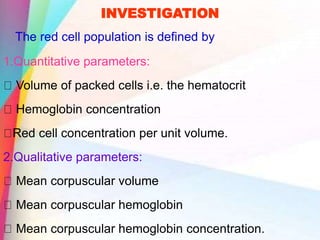
![INVESTIGATIONS
Red Cell Count: Total number of Red Cells per unit
volume of blood sample. [ No.of RBC/ cu.mm]
– Men - 4.2-5.4*106//mm3
– Women- 3.6-5.0*106/mm3](https://image.slidesharecdn.com/anemia-200717043003/85/Anemia-110-320.jpg)
![INVESTIGATIONS
Mean corpuscular Volume: It is the average volume a
RBC. [ fL ]
➢ Normal 82-98mm3or 82-98fL
Mean Corpuscular Hemoglobin: It is the average
hemoglobin content per RBC.
➢ Normal value is 27 to 31 pL
Mean Corpuscular Hemoglobin Concentration: It is the
average concentration of hemoglobin in a given Red Cell
Volume. [Gms/ dL ]
➢ Normal 32-36 g/Dl I](https://image.slidesharecdn.com/anemia-200717043003/85/Anemia-111-320.jpg)