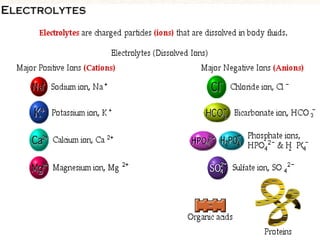
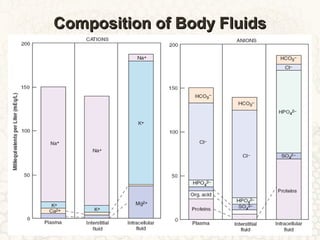
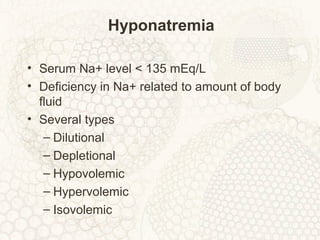
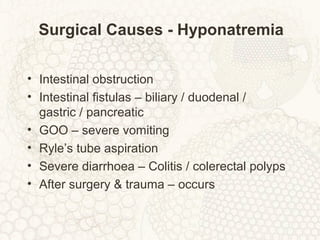
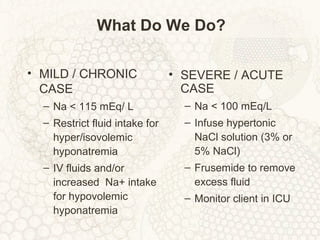
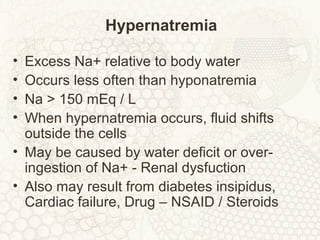
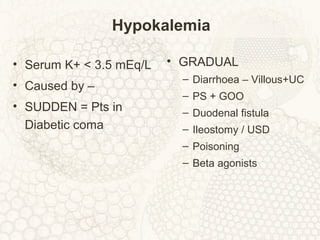
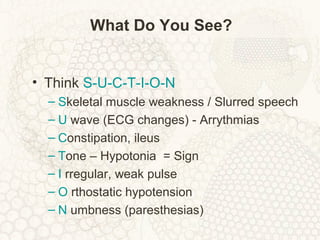
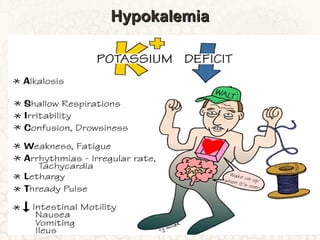
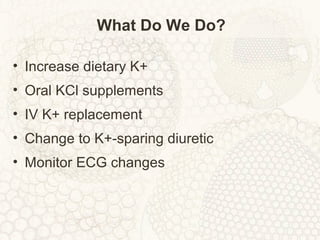
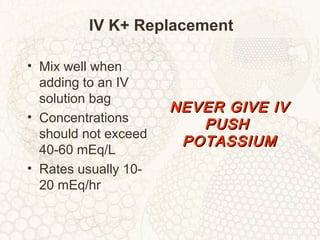
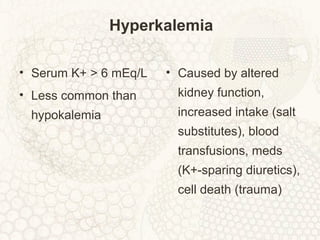
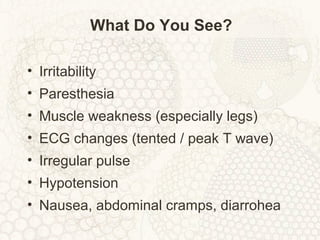
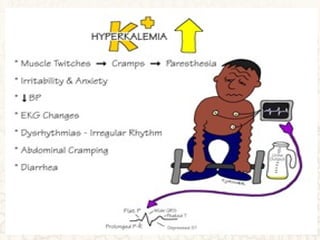
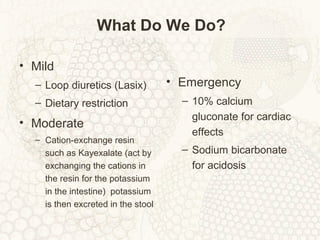
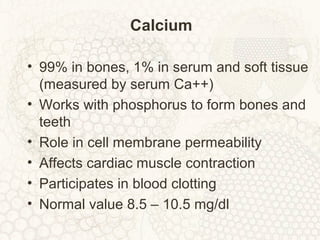
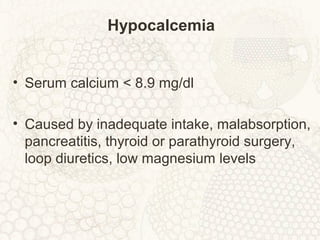
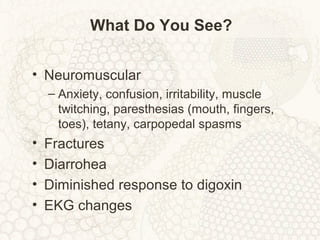
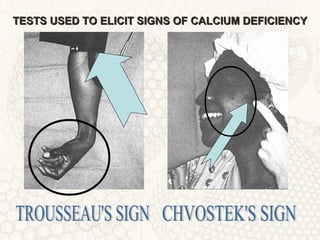
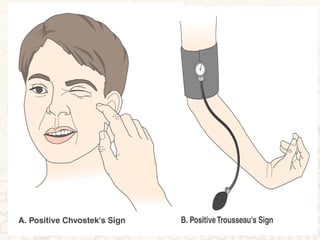
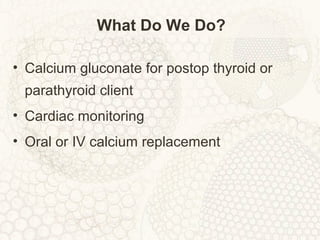
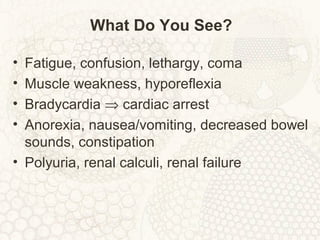
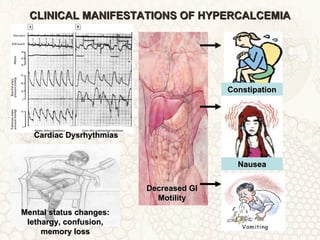
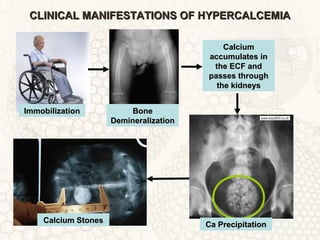
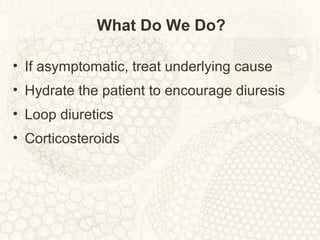
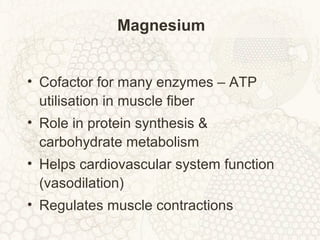
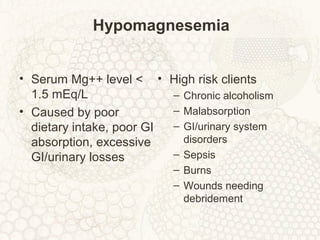
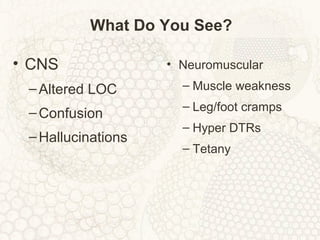
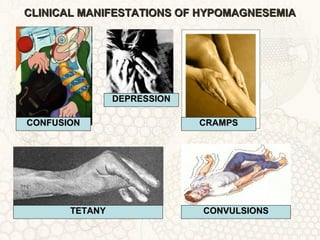
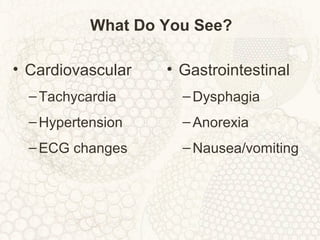
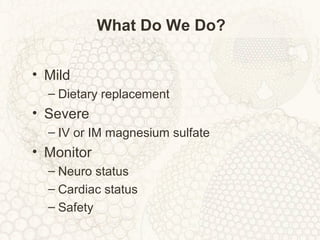
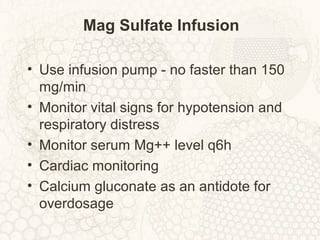
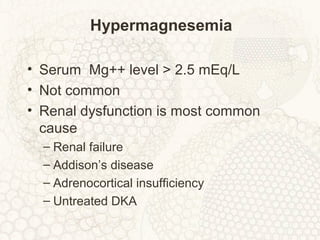
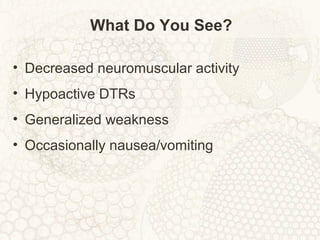
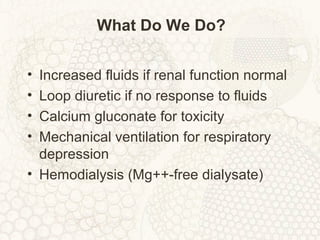
This document discusses electrolyte imbalances, including causes, signs and symptoms, and treatment approaches. It covers the major electrolytes: sodium, potassium, calcium, magnesium, and their roles in the body. Key points include how electrolytes are involved in neuromuscular function, acid-base balance, and fluid distribution. Electrolyte imbalances like hyponatremia, hyperkalemia, hypocalcemia and hypomagnesemia are described in terms of their definitions, causes, and clinical manifestations that clinicians should look for as well as treatment goals.