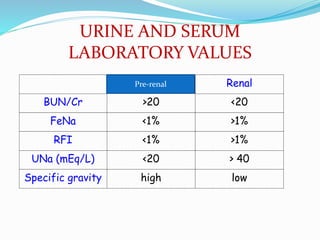
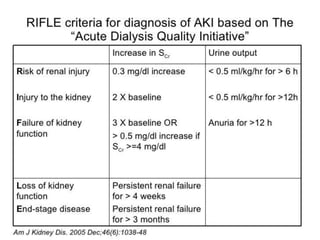
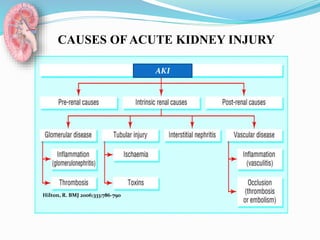
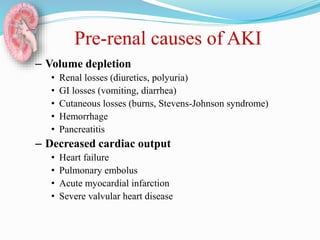
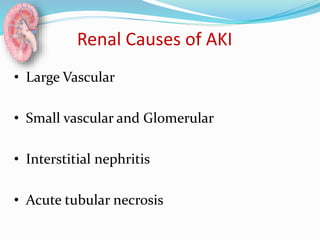
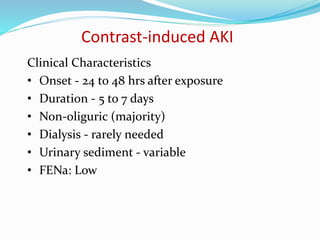
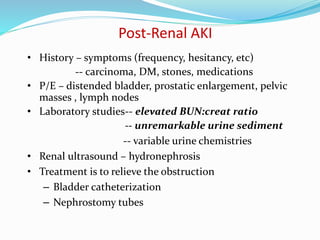
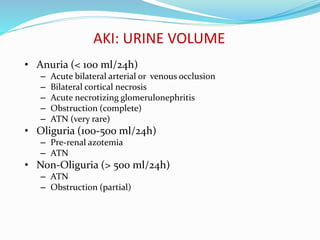
This document discusses acute kidney injury (AKI), formerly known as acute renal failure. It defines AKI and provides causes and characteristics of pre-renal, renal, and post-renal AKI. Pre-renal AKI is caused by decreased renal perfusion due to issues like volume depletion or heart failure. Renal AKI can be caused by issues affecting the glomeruli, interstitium, or tubules, such as acute tubular necrosis. Post-renal AKI is due to urinary tract obstruction. The document outlines evaluation of AKI including history, exam, urine and serum tests, imaging, and novel biomarkers. It also discusses complications of AKI and general management strategies.

![‘ACUTE KIDNEY INJURY’
Abrupt reduction [<48 hrs] in kidney
function, defined as an absolute increase in S
creatinine of ≥0.3 mg/dL
A percentage increase in S creatinine of ≥ 50%
[1.5 fold from baseline] or
a reduction in urine output-- documented
oliguria of < 0.5 ml/kg/hr, for more than six
hours.](https://image.slidesharecdn.com/acuterenalfailurearf-161119142307/85/Acute-renal-failure-arf-3-320.jpg)

![Post-renal causes of AKI
– Ureteric obstruction
• Stone disease,
• Tumor,
• Fibrosis,
• Ligation during pelvic surgery
– Bladder neck obstruction
• Benign prostatic hypertrophy [BPH]
• Cancer of the prostate
• Neurogenic bladder
• Drugs(Tricyclic antidepressants, ganglion blockers,
• Bladder tumor,
• Stone disease, hemorrhage/clot)
– Urethral obstruction (strictures, tumor)](https://image.slidesharecdn.com/acuterenalfailurearf-161119142307/85/Acute-renal-failure-arf-8-320.jpg)

























![Fractional Excretion of Na
• Since urinary indices depend on urine sodium
concentration, they should be interpreted cautiously if the
patient has received diuretic
Spot urine Na may be affected (raised) by diuretic use and
baseline impaired kidney function (CKD where maximum
urine Na reabsorption is impaired)
Fractional excretion of Na accounts for this by including
creatinine:
FxExNa = urine [Na] ÷ plasma [Na] X 100
urine creatinine ÷ plasma creatinine](https://image.slidesharecdn.com/acuterenalfailurearf-161119142307/85/Acute-renal-failure-arf-39-320.jpg)
![RENAL INDICES
• Renal Failure Index (RFI)
RFI = urine [Na]
urine creatinine /serum creatinine](https://image.slidesharecdn.com/acuterenalfailurearf-161119142307/85/Acute-renal-failure-arf-40-320.jpg)