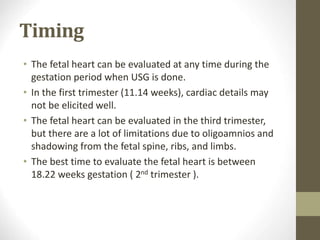
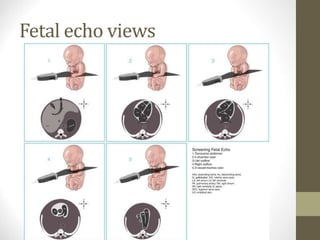
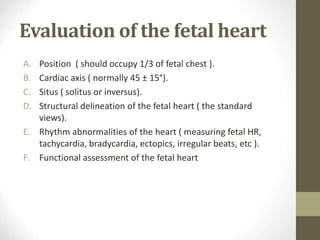
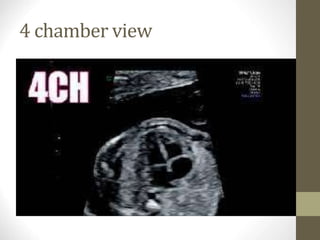
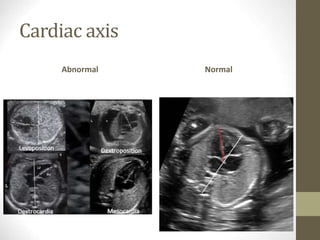
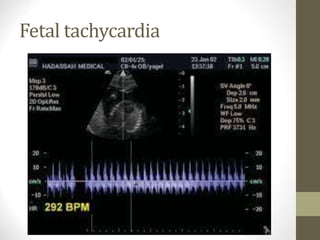
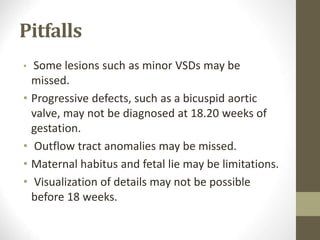
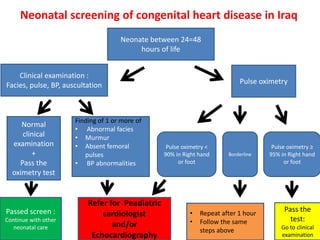
This document discusses fetal echocardiography, which is an important diagnostic tool used to detect congenital heart disease (CHD) in fetuses. It provides indications for fetal echocardiography including maternal factors like diabetes or autoimmune disorders, and fetal factors like a family history of CHD or abnormalities found on other scans. The best time for a fetal echocardiogram is between 18-22 weeks gestation. The exam evaluates heart structure, rhythm, positioning and function. It can detect various defects but may miss some minor issues. The document also discusses limitations and neonatal screening for CHD in Iraq.