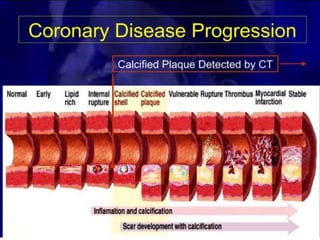
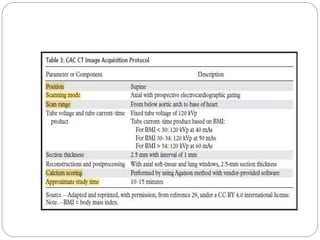
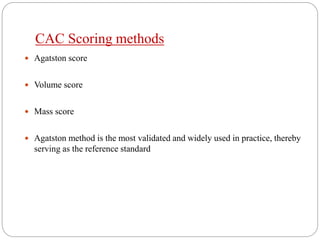
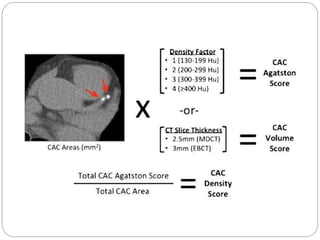
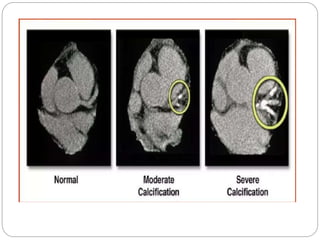
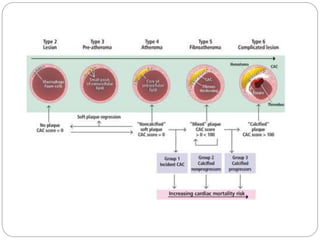
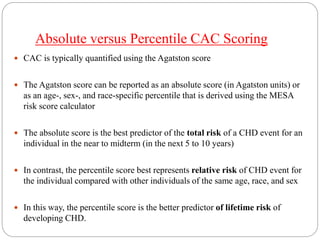
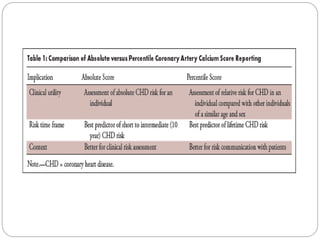
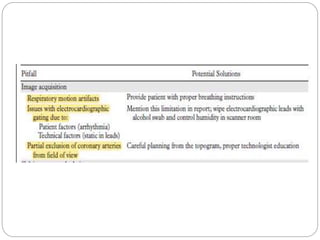
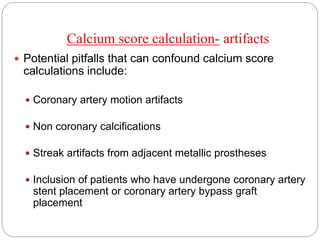
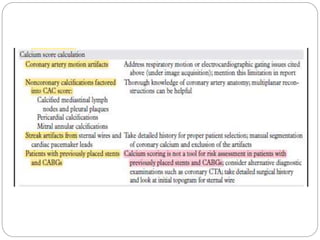
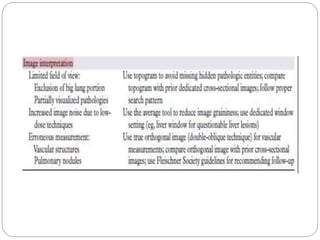
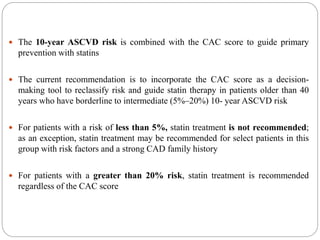
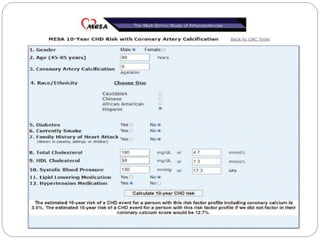
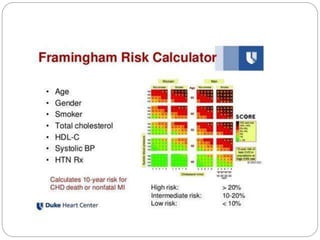
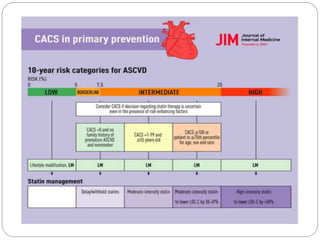
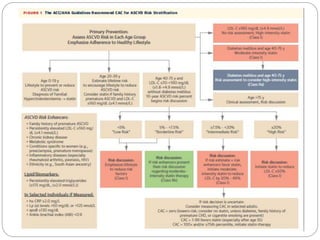
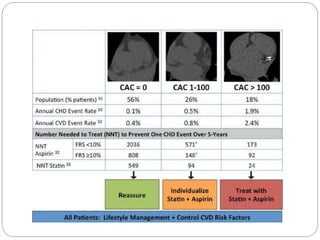
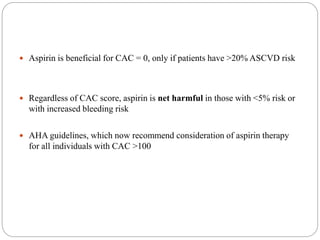
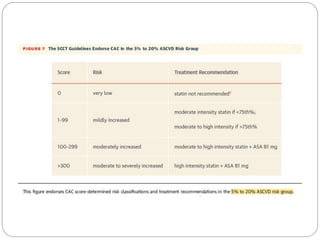
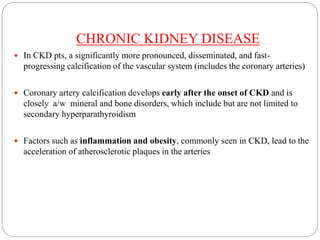
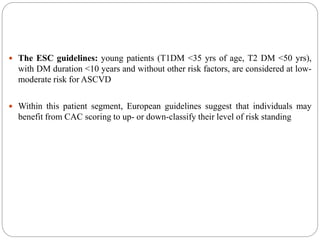
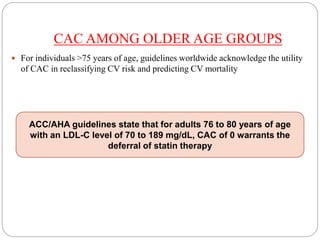
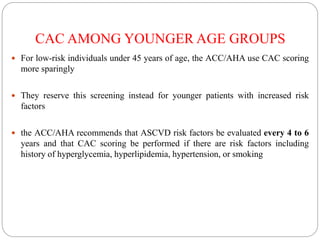
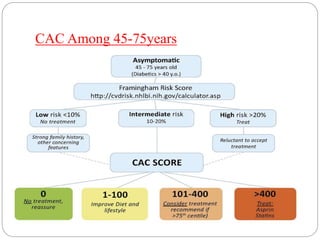
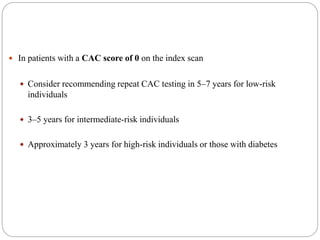
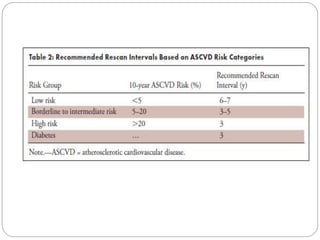
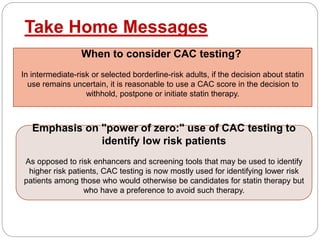
This document discusses coronary artery calcium (CAC) scoring, which is a noninvasive imaging technique used to assess risk of coronary heart disease. It begins by introducing CAC and its role in atherosclerosis. It then covers various CAC scoring methods and discusses interpreting absolute versus percentile scores. The document also addresses pitfalls in CAC scoring and how it can be used to guide statin and aspirin therapy. It concludes by covering special considerations for CAC scoring in patients with chronic kidney disease, diabetes, different age groups, and very high CAC scores.