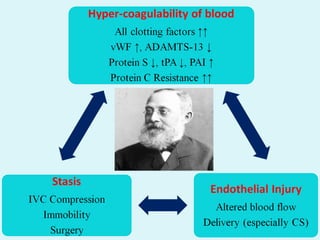
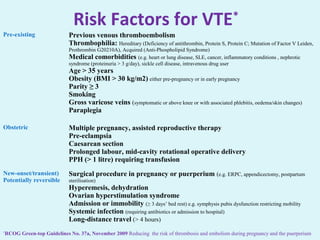
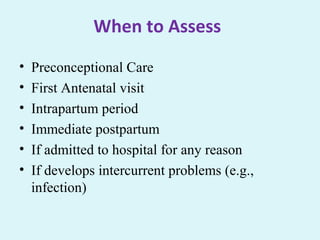
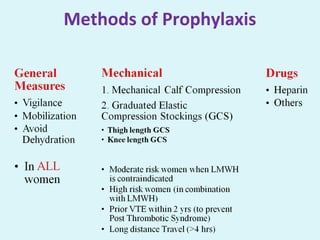
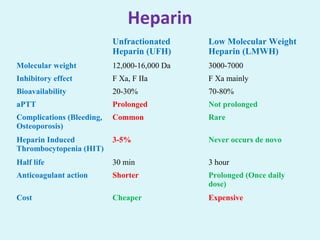
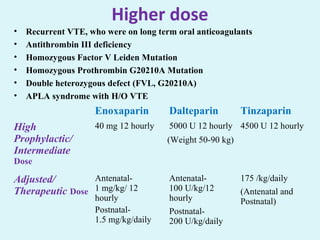
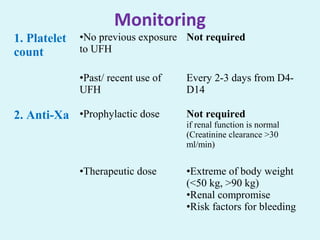
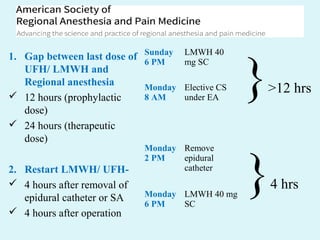
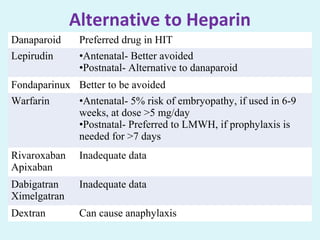
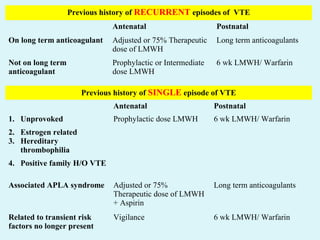
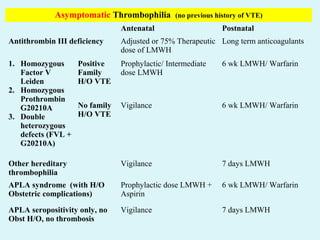
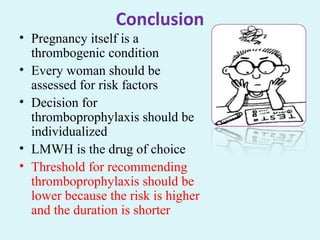
The document discusses the importance of thrombo-prophylaxis during pregnancy, detailing the incidence and risk factors associated with venous thromboembolism (VTE). It emphasizes the need for risk assessment and personalized prophylactic measures, recommending low molecular weight heparin as the preferred treatment. The document also highlights that VTE is a significant concern in both pregnant and postpartum women, particularly in India, where awareness and treatment remain inadequate.